Abstract
Purpose
Investigate the effect of adenotonsillectomy on mixed apnea index (MAI) and central apnea index (CAI) in children with moderate-to-severe obstructive sleep apnea syndrome (OSAS).
Methods
Observational retrospective analysis of polysomnographic data in children diagnosed with moderate-to-severe OSAS and without comorbidity, submitted to adenotonsillectomy.
Results
Data were available for 80 children, 55 boys and 25 girls, with a median age of 3.6 years (2.1–5.9). Before surgery AHI was 14.1 (11.0–18.4) per hour, with a median preoperative OAI of 7.1 (4.1–10.6), MAI of 1.2 (0.6–1.6) and CAI of 1.0 (0.4–2.0). Adenotonsillectomy caused significant improvements in MAI, from 1.2 (0.6–1.6) to 0.5 (0.1–0.8) (p < 0.001) and CAI from 1.0 (0.4–2.0) to 0.5 (0.1–0.9) (p < 0.001). This represents a normalization of MAI in 91.7% and CAI in 75.6% of children that had an abnormal value prior surgery.
Conclusion
Non obstructive apneas are common in children with OSAS. Adenotonsillectomy caused significant decrease not only in OAI, but also in MAI and CAI in children with moderate-to-severe OSAS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep apnea is the result of respiratory airflow pauses and has three major types: obstructive sleep apnea (OSA), mixed sleep apnea (MSA) and central sleep apnea (CSA) [1]. OSA is thought to occur in about 4–18% of healthy children, MSA in 0–6% and CSA in 1–37% [2,3,4,5]. All three types of apnea indices are higher in neonatal period, and tend to decrease with age [6]. Current data suggest that in children, the upper limit of normal values for obstructive and mixed apnea indices is less than one per hour [3, 6]. The minimum number of CSA required to cause a specific disorder remains elusive, but despite that, some authors consider a central apnea index (CAI) ≥ 1 to be abnormal [3, 7]. A finding of ≥ 5 central apneas per hour is more consensually considered clinically relevant, as it can be associated with underlying conditions such as anatomical brain and brainstem abnormalities, neurogenetic conditions, upper airway abnormalities, prematurity, gastroesophageal reflux, obesity, hypothyroidism and in the context of other sleep-disordered breathing (SDB) [3, 7, 8].
MSA have characteristics from both central and obstructive apneas. The cause of mixed apneas in patients with obstructive sleep apnea syndrome (OSAS) seems to be ventilatory control instability and upper airway collapsibility, as they increase along with OSAS severity [9]. The clinical implication of MSA has not been fully understood, and so, the impact of MSA events in OSAS tends to be ignored, and considered to be part of OSAS [1, 10]. Some studies show that patients with OSAS and also MSA tend to show a poorer compliance to continuous positive airway pressure (CPAP), and also a poorer respiratory control stability [10]. Central apneas are common in children with OSAS, and seems to be caused by arousals due to obstructive events. The variability of CAI in children with OSAS may be due to individual sensitivity of chemoreceptors to changes in partial pressure of carbon dioxide [7, 8].
American Academies of Otorhinolaryngology, Pediatrics and Sleep Medicine agree that adenotonsillectomy (AT) should be considered the first-line treatment for children with OSAS. AT causes a significant improvement in SDB in the majority of otherwise healthy, non-obese children, with a success rate of approximately 75%. Despite that, it is defended that some groups of children with predominantly nonobstructive events may benefit from other management options, as tonsillectomy may not be indicated [11, 12]. More recent studies show that when severe CSA appears associated with OSAS, it is likely to resolve following AT, even in cases of children with neurologic abnormalities. More authors defend the treatment of OSAS with AT prior to additional workup to identify etiology of CSA in children with persistent central events [3, 7, 8].
This study aims to show the effect of AT on apnea events, namely on central and mixed, in children diagnosed with OSAS. We theorize that AT may improve not only obstructive events, but also mixed and central events.
Methods
This was a retrospective study, performed at a single medical center (Professor Doutor Fernando Fonseca Hospital, Lisbon) between 2010 and 2020. The study was approved by local health ethics committee, and it was designed and conducted in compliance with the principles of Good Clinical Practice regulations and the Helsinki declaration.
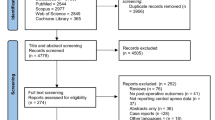
Since 2010, polysomnographic data from children with an Apnea Hypopnea Index (AHI) ≥ 10 per hour were recorded in a database system for evaluation of surgical success. Patient data were analyzed for possible inclusion in this study. Patients were considered for inclusion in this study if they were submitted to AT to treat OSAS and apart from the preoperative polysomnography (PSG) were also submitted to a postoperative PSG, 3–6 months following surgery. Patients with one or more of the following conditions were excluded: obesity (body mass index ≥ 2) or history of prematurity. None of the included patients were taking medication or had an underlying condition that might affect the respiratory pattern during sleep.
Polysomnography
Diagnosis of OSAS was based in a combination of clinical signs and symptoms and a full-night PSG. All children underwent nocturnal PSG at Pediatric Sleep Center at Professor Doutor Fernando Fonseca Hospital (level I PSG) and data were analyzed by the same department, according to American Academy of Sleep Medicine guidelines. The following variables were continuously measured and recorded by a computerized polysomnograph (Philips Respironics Alice): electroencephalography; electro-oculography; electromyography of anterior tibialis and chin muscles; electrocardiography; airflow was measured by means of nasal pressure cannula and thermistor; respiratory effort was measured by respiratory inductance plethysmography; transcutaneous oximetry and carbon dioxide monitoring; breathing noises; body position.
An apnea was considered when a drop of ≥ 90% in airflow compared with pre-event baseline respiration is seen. An apnea was classified as obstructive when it met apnea criteria for at least the duration of two breaths during baseline breathing and is associated with the presence of respiratory effort throughout the entire period of absent airflow. The obstructive apnea index (OAI) was defined as the number of obstructive apneas per hour of sleep. An apnea was classified as mixed when it met the apnea definition for at least the duration of two breaths during baseline breathing and was associated with absent respiratory effort during one portion of the event and the presence of inspiratory effort in another portion, regardless of which portion came first. The mixed apnea index (MAI) was defined as the number of mixed apneas per hour of sleep, and an MAI ≥ 1/h was considered abnormal. A central apnea was considered when it met apnea criteria and was associated with absent inspiratory effort throughout the entire duration of the event, and at least one of the following was met: the event lasted 20 s or longer, the event lasted at least the duration of two breaths during baseline breathing and was associated with an arousal or 3% or more oxygen desaturation. The central apnea index (CAI) was defined as the number of central apneas per hour of sleep, a CAI ≥ 1/h was considered abnormal and a central sleep apnea syndrome (CSAS) was defined when a CAI was superior to 5/h.
Surgeries
All patients were submitted to AT. Adenoidectomy was performed with curettes. The technique used to perform tonsillectomy was extracapsular dissection with bipolar cautery.
Statistical analysis
Statistical analysis was performed with SPSS version 26.0 software (International Business Machines Corporation, USA). Data were presented as median (25-75th percentile). Comparisons between groups were made by Wilcoxon Signed-Rank or Mann–Whitney U test, and correlations were made with Spearman’s Rank Correlation. Statistical significance was accepted at p < 0.05.
Results
Study population
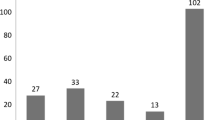
Eighty child were eligible for inclusion in this study: 55 boys and 25 girls, with a median age of 3.6 years (2.1–5.9) years. Pre-operative median AHI was 14.1 (11.0–18.4) per hour, with a median preoperative OAI of 7.1 (4.1–10.6), MAI of 1.2 (0.6–1.6) and CAI of 1.0 (0.4–2.0). Tonsils were graded using the scheme by Brodsky et al. [13]: 2.5% of patients were classified as grade I, 16.2% as grade II, 51.3% as grade III, and 30.0% as grade IV. Tonsil grade and corresponding success rates are displayed in Table 1. There was no significant differences in success rate, preoperative MAI, OIA or CAI between subgroups of children accordingly with tonsil grades.
All 80 children were submitted to adenotonsillectomy as a treatment of OSAS. After surgery 42.5% of children had an OAI < 1/h, 46.3% an OIA between 1 and < 5/h, 3.8% an OIA ≥ 5/h. After adenotonsillectomy 2.6% of children had an AHI < 1/h, 78.6% and AHI between 1 and < 5/h and 18.8% of children had an AHI ≥ 5/h.
Effect of adenotonsillectomy on mixed apneas
Adenotonsillectomy caused significant improvement in MAI, from 1.2 (0.6–1.6) to 0.5 (0.1–0.8) (p < 0.001). Preoperatively, a total of 61.3% of children had MAI ≥ 1/h, and 2.2% had an MAI > 5/h. After surgery 15.0% of children had an MAI ≥ 1/h. This represents a normalization of MAI in 91.7% of children that had an abnormal value prior surgery.
There was no significant correlation between MAI and AHI, OIA, CAI, mean and median oxygen saturation or age.
To investigate the effect of adenotonsillectomy on MAI, a group of 49 children with a MAI ≥ 1/h was selected. Characteristics of both groups are displayed in Table 2.
Children with an abnormal MAI had significant higher OAI, when compared with children with an MAI < 1/h.
Effect of adenotonsillectomy on central apneas
Surgery promoted significant improvements in CAI from 1.0 (0.4–2.0) to 0.5 (0.1–0.9) (p < 0.001). Preoperatively, a total of 51.3% of children had CAI ≥ 1/h, and 5.0% superior to 5/h. After surgery only 23.8% of children had a CAI ≥ 1/h, and none had a CAI > 5/h. This represents a normalization of CAI in 75.6% of children that had an abnormal value prior surgery. Pre-operative and postoperative comparisons of sleep parameters are displayed in Table 3.
A significant correlation was found between CAI and mean oxygen saturation (r = 0.3, p = 0.012). There was no significant correlation between CAI and AHI, OIA, minimum oxygen saturation or age.
Discussion
More than half of children otherwise healthy with OSAS also had abnormal MAI (61.3% of children) and CAI (51.3%) during sleep, and 5% had CSAS. The data show that abnormal values of nonobstructive apneas are common in children with OSAS.
The majority of children included in this study had tonsillar hypertrophy (grade III and IV). No significant differences were seen in success rates, preoperative MAI, OIA or CAI between subgroups of children accordingly with tonsil grades. Could be expected that an increased tonsil size would be related with a higher AHI. There are some factors reported in the literature that could explain why this is not always encountered. It is known that subjective tonsil size assessment have interrater reliability. It is difficult to get a clear visual assessment of the tonsil in children, as they usually are not cooperative with a throat exam. Tonsil size grading scale assesses the tonsil position relative to tonsillar pillars, and not necessarily the tonsil size [14]. Howard et al. suggest that intra-oral subjective size assessment of tonsil size do not closely correlate with pediatric preoperative AHI. The authors advocate that objective tonsil size, considering the three-dimensional size of the tonsils, is more useful to predict AHI [15].
Central apneas may be caused by physiologic or idiopathic mechanisms or may be secondary to other medical conditions [7]. It is believed that abnormal CAI values in children with OSAS are a relatively common finding, and probably secondary to post-arousal effects of obstructive apneas and hypopneas. In children with OSAS and abnormal CAI, a higher PaCO2 set point is stablished during sleep. Following an arousal occurs a drop in PaCO2, and this may cause a temporary cessation of respiratory drive, resulting in central apnea [7, 8]. Previous studies have found a prevalence of CAI ≥ 1/h in children with OSAS ranging from 15 to 64%, and this study found a prevalence within this range (51.3%) [7, 8, 16]. The clinical importance of an abnormal CAI in the context of OSAS is debated, even in children with CSAS. In the absence of OSAS, CSAS often indicates a neurologic abnormality, and the opposite is true for CSAS in context of OSAS. Abnormal CAI in the context of OSAS is likely to resolve after AT in the majority of children, even in cases of children with neurologic abnormalities. Therefore OSAS should be treated prior to additional workup for causes of persistent abnormal CAI following AT, namely central nervous system abnormalities [7].
Mixed apneas are rarely found in healthy children [2, 4, 17]. In this study, in a population of otherwise healthy children with OSAS, almost all children had one or more mixed apneas during sleep, and 61.3% of children had a MAI ≥ 1/h. Since mixed apneas are pathophysiologically considered to be part of OSAS, some studies do not differentiate obstructive from mixed events [10, 11, 18]. The mentioned may help to justify the lack of studies reporting the prevalence of mixed apneas in children with OSAS. Since the implication of mixed events in OSAS has not been well studied, their impact in this syndrome tends to be ignored. Yang et al. reported that MAI is found more frequently in patients with severe OSAS, proposing that mixed events was associated with higher loop gain and consequently with ventilatory control instability [1]. This may justify the high frequency of abnormal MAI found in this group of children with moderate-to-severe OSAS. Other studies suggest that patients with OSAS with mixed apneas have more breathing irregularities, suggesting that central respiratory control of this patients are different from the ones with pure obstructive events [19, 20].
Adenotonsillectomy is the first-line treatment for children with OSAS, as it causes significant improvement in sleep-disordered breathing (SDB) in the majority of children. Despite that, it is defended that some groups of children with predominantly nonobstructive events may benefit from other management options [11, 12]. Depending on the definition of surgical success and on the presence of additional comorbidities, previous studies report adenotonsillectomy success rates ranging from 23 to 90% of children with OSAS [12]. Considering success rate of a postoperative AHI < 5/h, this study found that 81.2% of children had a successful treatment, a value within the range described in the literature. In this study, after adenotonsillectomy, reductions were seen not only in OAI from 7.1 (4.1–10.6) to 1.1 (0.6–2.1) (p < 0.001), but also in MAI from 1.2 (0.6–1.6) to 0.5 (0.1–0.8) (p < 0.001) and CAI from 1.0 (0.4–2.0) to 0.5 (0.1–0.9) (p < 0.001).
Previous studies already report significant reductions in CAI following adenotonsillectomy, with a tendency for the resolution of CSAS [7, 8, 13]. In this study, after adenotonsillectomy only 23.8% of children had a CAI ≥ 1/h, and none had CSAS. This represents a normalization of CAI in 75.6% of children that had an abnormal value prior surgery. The major reason pointed for this results is that following resolution of OSAS, the arousals secondary to obstructive events resolves, which are the major stimulus for central apneas [7].
In this study, after surgery 15.0% of children had an MAI ≥ 1/h, compared with 61.3% of children prior adenotonsillectomy. This represents a normalization of MAI in 91.7% of children that had an abnormal value prior surgery. So far, mixed apnea is pathophysiologically considered to be part of obstructive events, and so, the decrease of mixed events should result from the resolution of the upper airway obstruction [1, 10, 11]. In this study, no correlation was found between MAI and AHI, OIA or CAI. Another cause pointed for the emergence of mixed apneas in patients with OSAS is the poor ventilatory control stability related with severe OSAS [7]. In this study, that included children with moderate-to-severe OSAS, none had severe OSAS after surgical treatment. The significative AHI decrease may have caused improvements in ventilatory control stability, which may ultimately lead to significant reductions in MAI.
There are some limitations in our study, some of them because of its retrospective nature. For example, some patients were excluded due to incomplete preoperative polysomnographic data. Another limitation was the homogenous population studied, and so, the results of this study are applicable only to a highly selected population. There is limited clinical interest in mixed events, because they tend to be considered obstructive, and so few data were published on about this subject [1, 11]. The results of our study offer some valuable insight into this topic. Future studies should include randomized prospective trials to confirm the findings.
Conclusion
Non obstructive apneas are common in children with OSAS. Adenotonsillectomy lead to significant improvements in nonobstructive events, with a tendency to resolution of mixed and central apneas abnormalities. The present study provides additional support to the increasing debate about the possible slight clinical relevance of CAI in children with OSAS, before AT, especially if CAI ≤ 5.
Data availability
The data that support the findings of this study cannot be shared openly to protect study participant privacy and are available from the corresponding author upon reasonable request and with permission from the local ethics committee. Data are located in controlled access data storage at Hospital Professor Doutor Fernando Fonseca.
References
Yang X, Xiao Y, Han B, Lin K et al (2019) Implication of mixed sleep apnea events in adult patients with obstructive sleep apnea-hypopnea syndrome. Sleep Breath 23:559–565. https://doi.org/10.1007/s11325-018-1745-0
Marcus CL, Omlin KJ, Basinki DJ et al (1992) Normal polysomnographic values for children and adolescents. Am Rev Respir Dis 146:1235–1239. https://doi.org/10.1164/ajrccm/146.5_Pt_1.1235
McLaren AT, Bin-Hasan S, Narang I (2019) Diagnosis, management and pathophysiology of central sleep apnea in children. Pediatr Respir Rev 30:49–57
Uliel S, Tauman R, Greenfield M et al (2004) Normal polysomnographic respiratory values in children and adolescents. Chest 125(3):872–878. https://doi.org/10.1378/chest.125.3.872
Moss D, Urschitz MS, Bodman A et al (2005) Reference values for nocturnal home polysomnography in primary schoolchildren. Pediatr Res 58(5):958–965. https://doi.org/10.1203/01.PDR.0000181372.34213.13
Ng DN, Chan CH (2013) A review of normal values of infant sleep polysomnography. Pediatr Neonatol 54:82–87
Judd RT, Mokhlesi B, Shogan A, Baroody FM (2021) Improvement in central sleep apnea following adenotonsillectomy in children. Laryngoscope 132(2):478–484. https://doi.org/10.1002/lary.29784
Boudewyns A, Van de Heyning P, Verhulst S (2016) Central apneas in children with obstructive sleep apnea syndrome: prevalence and effect of upper airway surgery. Sleep 25:93–97. https://doi.org/10.1016/j.sleep.2016.05.018
Herkenrath S, Pavsic K, Treml M, Hagmeyer L et al (2019) Mixed apnea metrics during diagnostic polydomnographies in obstructive sleep apnea patients with/without treatment-emergent central sleep apnea. Eur Respir J 54(Suppl 63):PA824. https://doi.org/10.1183/13993003.congress-2019.PA824
Liu P, Chen Q, Yuan F, Zhang Q et al (2022) Clinical predictors of mixed apneas in patients with obstructive sleep apnea (OSA). Nat Sci Sleep 14:373–380. https://doi.org/10.2147/NSS.S351946
The Report of an American Academy of Sleep Medicine Task Force (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep 1999(22):667–689
Boudewyns A, Abel F, Alexopoulos E et al (2017) Adenotonsillectomy to treat obstructive sleep apnea: is it enough? Pediatric Pulmonoloy 52(5):699–709. https://doi.org/10.1002/ppul.23641
Brodsky L, Moore L, Stanievich JF (1987) A comparison of tonsillar size and oropharyngeal dimensions in children with obstructive adenotonsillar hypertrophy. Int J Pediatr Otorhinolaryngol 13:149–156. https://doi.org/10.1016/0165-5876(87)90091-7
Nolan J, Brietzke SE (2011) Systematic review of pediatric tonsil size and polysomnogram-measured obstructive sleep apnea severity. Otolaryngol-Head Neck Surg 144(6):844–850. https://doi.org/10.1177/0194599811400683
Howard NS, Brietzke SE (2009) Pediatric tonsil size: objective vs subjective measurements correlated to overnight polysomnogram. Otolaryngol-Head Neck Surg 140:675–681. https://doi.org/10.1016/j.otohns.2009.01.008
Baldassari CM, Kepchar J, Bryant L et al (2012) Changes in central apnea index following pediatric adenotonsillectomy. Otolaryngol Head Neck Surg 1416:487–490
Montgomery-Downs HE, O’Brien LM, Gulliver TE et al (2014) Polysomnographic characteristics in normal preschool and early school-aged children. Pediatrics 117(3):741–753. https://doi.org/10.1542/peds.2005-1067
Kato I, Franco P, Groswasser J et al (2000) Frequency of obstructive and mixed sleep apneas in 1,023 infants. Sleep 23(4):487–492. https://doi.org/10.1093/sleep/23.4.1b
Yamauchi M, Tamaki S, Yoshikawa M et al (2011) Differences in breathing patterning during wakefulness in patients with mixed apnea-dominant vs obstructive-dominant sleep apnea. Chest 140(1):54–61. https://doi.org/10.1378/chest.10-1082
Xie A, Bedekar A, Skatrud JB et al (2011) The heterogeneity of obstructive sleep apnea (predominant obstructive vs pure obstructive apnea). Sleep 34(6):745–750. https://doi.org/10.5665/SLEEP.1040
Funding
Open access funding provided by FCT|FCCN (b-on).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests.
Additional information
This article is part of the Topical Collection on sleep apnea syndrome. Guest editors: Manuele Casale, Rinaldi Vittorio.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Antunes, J., Carvalho, J., Marinho, C. et al. Central and mixed apneas in children with obstructive sleep apnea: effect of adenotonsillectomy. Eur Arch Otorhinolaryngol 281, 3125–3130 (2024). https://doi.org/10.1007/s00405-023-08442-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-08442-7