Abstract
Purpose
Facial palsy (FP) is the most significant complication of parotidectomy. Currently, the use of intermittent intraoperative neuromonitoring (iIONM) in parotid surgery facilitates nerve detection, which is paramount to nerve protection. Continuous IONM (cIONM), as applied in thyroid surgery, enables real-time information on electrophysiological nerve status through continuous nerve stimulation, thereby allowing consequent amplitude analysis. To date, the application of cIONM in parotid surgery has not been noted in literature.
Methods
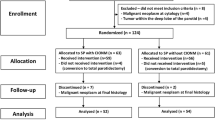
We performed parotidectomies with anterograde facial nerve visualization using cIONM in 32 consecutive patients in a prospective study (German Register of clinical studies—DRKS 00011051) during the period October 2016 to January 2020. After the facial trunk had been exposed, an atraumatic stimulation electrode was placed and the nerve was stimulated at 3 Hz, at a low threshold (0.62 ± 0.06 mA), for the entire duration of the preparation. Selected electrophysiological parameters were collected and compared to postoperative facial nerve function, measured by the House-Brackmann grading system.
Results
In the post hoc analysis, a significant correlation between a drop in amplitude (< 50% of the “baseline” amplitude) and postoperative FP was recorded (p = 0.001). True positive prediction of FP was noted in 14 out of 16 patients and true negative in 10 out of 16. The sensitivity was 87.5% (AUC 0.75), with a high negative predictive value of 83.3%.
Conclusion
cIONM has significant value in predicting postoperative FP in parotidectomy. Future development of an acoustic/optic warning system in IONM devices could prevent nerve injury in real time.





Similar content being viewed by others
References
Kadletz L, Grasl S, Grasl MC, Perisanidis C, Erovic BM (2017) Extracapsular dissection versus superficial parotidectomy in benign parotid gland tumors: the Vienna Medical School experience: outcomes of parotid gland surgery. Head Neck 39(2):356–360. https://doi.org/10.1002/hed.24598
Grosheva M, Klussmann JP, Grimminger C et al (2009) Electromyographic facial nerve monitoring during parotidectomy for benign lesions does not improve the outcome of postoperative facial nerve function: a prospective two-center trial. Laryngoscope 119(12):2299–2305. https://doi.org/10.1002/lary.20637
Bova R, Saylor A, Coman WB (2004) Parotidectomy: review of treatment and outcomes. ANZ J Surg 74(7):563–568. https://doi.org/10.1111/j.1445-2197.2004.02988.x
Prats-Golczer VE, Gonzalez-Cardero E, Exposito-Tirado JA, Montes-Latorre E, Gonzalez-Perez LM, Infante-Cossio P (2017) Impact of dysfunction of the facial nerve after superficial parotidectomy: a prospective study. Br J Oral Maxillofac Surg 55(8):798–802. https://doi.org/10.1016/j.bjoms.2017.07.006
Savvas E, Hillmann S, Weiss D, Koopmann M, Rudack C, Alberty J (2016) Association between facial nerve monitoring with postoperative facial paralysis in parotidectomy. JAMA Otolaryngol Neck Surg 142(9):828. https://doi.org/10.1001/jamaoto.2016.1192
Gaillard C, Perie S, Susini B, St Guily JL (2005) Facial nerve dysfunction after parotidectomy: the role of local factors. Laryngoscope 115(2):287–291. https://doi.org/10.1097/01.mlg.0000154735.61775.cd
Guntinas-Lichius O, Gabriel B, Peter KJ (2006) Risk of facial palsy and severe Frey’s syndrome after conservative parotidectomy for benign disease: analysis of 610 operations. Acta Otolaryngol (Stockh) 126(10):1104–1109. https://doi.org/10.1080/00016480600672618
Sood AJ, Houlton JJ, Nguyen SA, Gillespie MB (2015) Facial nerve monitoring during parotidectomy: a systematic review and meta-analysis. Otolaryngol Neck Surg 152(4):631–637. https://doi.org/10.1177/0194599814568779
Chiesa-Estomba CM, Larruscain-Sarasola E, Lechien JR et al (2021) Facial nerve monitoring during parotid gland surgery: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol 278(4):933–943. https://doi.org/10.1007/s00405-020-06188-0
Schneider R, Sekulla C, Machens A, Lorenz K, Nguyen Thanh P, Dralle H (2015) Postoperative vocal fold palsy in patients undergoing thyroid surgery with continuous or intermittent nerve monitoring. Br J Surg 102(11):1380–1387. https://doi.org/10.1002/bjs.9889
Stankovic P, Wittlinger J, Georgiew R, Dominas N, Hoch S, Wilhelm T (2020) Continuous intraoperative neuromonitoring (cIONM) in head and neck surgery—a review. HNO 68(S2):86–92. https://doi.org/10.1007/s00106-020-00824-1
House J, Brackmann D (1985) Facial nerve grading system. Otolaryngol Head Neck Surg 93(2):146–147. https://doi.org/10.1177/019459988509300202
Haring CT, Ellsperman SE, Edwards BM et al (2019) Assessment of intraoperative nerve monitoring parameters associated with facial nerve outcome in parotidectomy for benign disease. JAMA Otolaryngol Neck Surg 145(12):1137. https://doi.org/10.1001/jamaoto.2019.1041
Eren SB, Dogan R, Ozturan O, Veyseller B, Hafiz AM (2017) How deleterious is facial nerve dissection for the facial nerve in parotid surgery: an electrophysiological evaluation. J Craniofac Surg 28(1):56–60. https://doi.org/10.1097/SCS.0000000000003186
Ozturk K, Akyildiz S, Gode S, Turhal G, Gursan G, Kirazli T (2016) The effect of partial superficial parotidectomy on amplitude, latency and threshold of facial nerve stimulation. Eur Arch Otorhinolaryngol 273(6):1527–1531. https://doi.org/10.1007/s00405-015-3622-9
Psychogios G, Bohr C, Constantinidis J et al (2021) Review of surgical techniques and guide for decision making in the treatment of benign parotid tumors. Eur Arch Otorhinolaryngol 278(1):15–29. https://doi.org/10.1007/s00405-020-06250-x
Mantsopoulos K, Koch M, Klintworth N, Zenk J, Iro H (2015) Evolution and changing trends in surgery for benign Parotid tumors: trends in surgery for benign parotid tumors. Laryngoscope 125(1):122–127. https://doi.org/10.1002/lary.24837
Grosheva M, Pick C, Granitzka T et al (2019) Impact of extent of parotidectomy on early and long-term complications: a prospective multicenter cohort trial. Head Neck 41(6):1943–1951. https://doi.org/10.1002/hed.25651
Schneider R, Randolph GW, Sekulla C et al (2013) Continuous intraoperative vagus nerve stimulation for identification of imminent recurrent laryngeal nerve injury: continuous IONM for Thyroid Surgery. Head Neck 35(11):1591–1598. https://doi.org/10.1002/hed.23187
Amano M, Kohno M, Nagata O, Taniguchi M, Sora S, Sato H (2011) Intraoperative continuous monitoring of evoked facial nerve electromyograms in acoustic neuroma surgery. Acta Neurochir (Wien) 153(5):1059–1067. https://doi.org/10.1007/s00701-010-0937-6
Ulkatan S, Waner M, Arranz-Arranz B et al (2014) New methodology for facial nerve monitoring in extracranial surgeries of vascular malformations. Clin Neurophysiol 125(4):849–855. https://doi.org/10.1016/j.clinph.2013.08.030
Funding
This project was funded entirely by the Department of the corresponding author.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have indicated that they have no conflict of interest.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Saxonian Physician’s Chamber, Germany (EK-BR-53/16-1) in September 2016.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stanković, P., Hoch, S., Stuck, B.A. et al. Continuous intraoperative neuromonitoring of the facial nerve predicts postoperative facial palsy in parotid surgery: a prospective study. Eur Arch Otorhinolaryngol 281, 1483–1492 (2024). https://doi.org/10.1007/s00405-023-08384-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-08384-0