Abstract
Objective
Eosinophilic chronic rhinosinusitis (eCRS) is a refractory subtype of CRS. This study aimed to compare the differences in clinical features and peripheral blood indices between eCRS and non-eCRS Chinese patients and identify the predictive factors for eCRS.
Methods
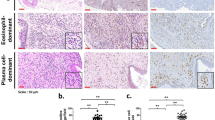
In this study, a total of 1352 patients with CRS were enrolled and divided into eCRS and non-eCRS groups based on the degree of eosinophilic infiltration in histopathology, and their demographic and clinical characteristics, as well as peripheral blood indices, were compared. Logistic regression analysis was used to identify the factors associated with eCRS, and the optimal cut-off values of predictors were determined using subject working curves.
Results
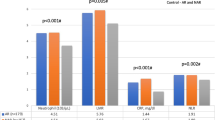
As compared to those in the non-eCRS group patients, the proportion of males, age, proportion of smokers, peripheral blood eosinophil count, and erythrocyte count were significantly higher, while the peripheral blood neutrophil count, platelet count, neutrophil/lymphocyte count ratio (NLR), platelet/lymphocyte count ratio (PLR), and neutrophil × platelet/lymphocyte count ratio (SII index) were significantly lower in the eCRS group patients. Logistic regression analysis showed that age, peripheral blood neutrophil count, eosinophil count, and platelet count were independent predictors of eCRS, and eosinophil count > 2.05 × 108/L could be used as a diagnostic marker for eCRS with a sensitivity and specificity of 87.1% and 78.3%, respectively.
Conclusions
There were significant differences in the clinical features of eCRS and non-eCRS patients. Peripheral blood eosinophil count could early and more accurately predict eCRS.

Similar content being viewed by others
Data availability
The data are available from the corresponding author on reasonable request.
References
Fokkens WJ, Lund VJ, Hopkins C et al (2020) European position paper on rhinosinusitis and nasal polyps 2020. Rhinology 58(Suppl S29):1–464. https://doi.org/10.4193/Rhin20.600
Hong SJ, Lee JK, Lee HS et al (2014) Availability of preoperative systemic steroids on endoscopic sinus surgery for chronic rhinosinusitis with nasal polyposis. Yonsei Med J 55(6):1683–1690. https://doi.org/10.3349/ymj.2014.55.6.1683
Brescia G, Barion U, Zanotti C et al (2017) The prognostic role of serum eosinophil and basophil levels in sinonasal polyposis. Int Forum Allergy Rhinol 7(3):261–267. https://doi.org/10.1002/alr.21885
Zhang Z, Li G, Yu L et al (2023) Causal relationships between potential risk factors and chronic rhinosinusitis: a bidirectional two-sample Mendelian randomization study. Eur Arch Otorhinolaryngol 280(6):2785–2793. https://doi.org/10.1007/s00405-022-07798-6
Orlandi RR, Kingdom TT, Smith TL et al (2021) International consensus statement on allergy and rhinology: rhinosinusitis 2021. Int Forum Allergy Rhinol 11(3):213–739. https://doi.org/10.1002/alr.22741
Kim DH, Kim SW, Basurrah MA et al (2022) Clinical and laboratory features of various criteria of eosinophilic chronic rhinosinusitis: a systematic review and meta-analysis. Clin Exp Otorhinolaryngol 15(3):230–246. https://doi.org/10.21053/ceo.2022.00052
Christensen DN, Franks ZG, McCrary HC et al (2018) A systematic review of the association between cigarette smoke exposure and chronic rhinosinusitis. Otolaryngol Head Neck Surg 158(5):801–816. https://doi.org/10.1177/0194599818757697
Sedaghat AR, Kuan EC, Scadding GK (2022) Epidemiology of chronic rhinosinusitis: prevalence and risk factors. J Allergy Clin Immunol Pract 10(6):1395–1403. https://doi.org/10.1016/j.jaip.2022.01.016
Krzeski A, Galewicz A, Chmielewski R et al (2011) Influence of cigarette smoking on endoscopic sinus surgery long-term outcomes. Rhinology 49(5):577–582. https://doi.org/10.4193/Rhino.10.038
Fujieda S, Imoto Y, Kato Y et al (2019) Eosinophilic chronic rhinosinusitis. Allergol Int 68(4):403–412. https://doi.org/10.1016/j.alit.2019.07.002
Zhang N, Van Zele T, Perez-Novo C et al (2008) Different types of t-effector cells orchestrate mucosal inflammation in chronic sinus disease. J Allergy Clin Immunol 122(5):961–968. https://doi.org/10.1016/j.jaci.2008.07.008
Sivrice ME, Okur E, Yasan H et al (2020) Can the systemic immune inflammation index preoperatively predict nasal polyp subtypes? Eur Arch Otorhinolaryngol 277(11):3045–3050. https://doi.org/10.1007/s00405-020-06174-6
Delemarre T, Holtappels G, De Ruyck N et al (2021) A substantial neutrophilic inflammation as regular part of severe type 2 chronic rhinosinusitis with nasal polyps. J Allergy Clin Immunol 147(1):179-188.e172. https://doi.org/10.1016/j.jaci.2020.08.036
Stone RM, Gilliland DG, Klion AD (2004) Platelet-derived growth factor receptor inhibition to treat idiopathic hypereosinophilic syndrome. Semin Oncol 31(2 Suppl 6):12–17. https://doi.org/10.1053/j.seminoncol.2004.03.035
Takabayashi T, Schleimer RP (2020) Formation of nasal polyps: the roles of innate type 2 inflammation and deposition of fibrin. J Allergy Clin Immunol 145(3):740–750. https://doi.org/10.1016/j.jaci.2020.01.027
Shimizu S, Ogawa T, Takezawa K et al (2015) Tissue factor and tissue factor pathway inhibitor in nasal mucosa and nasal secretions of chronic rhinosinusitis with nasal polyp. Am J Rhinol Allergy 29(4):235–242. https://doi.org/10.2500/ajra.2015.29.4183
Rha MS, Jeong Y, Kim J et al (2022) Is obstructive sleep apnea associated with erythrocytosis? A systematic review and meta-analysis. Laryngoscope Investig Otolaryngol 7(2):627–635. https://doi.org/10.1002/lio2.751
Wojan F, Stray-Gundersen S, Nagel MJ et al (1985) (2021) Short exposure to intermittent hypoxia increases erythropoietin levels in healthy individuals. J Appl Physiol 130(6):1955–1960. https://doi.org/10.1152/japplphysiol.00941.2020
Grayson JW, Li W, Ho J et al (2020) Topography of polyp recurrence in eosinophilic chronic rhinosinusitis. Int Forum Allergy Rhinol 10(5):604–609. https://doi.org/10.1002/alr.22529
Wang X, Meng Y, Lou H et al (2021) Blood eosinophil count combined with asthma history could predict chronic rhinosinusitis with nasal polyp recurrence. Acta Otolaryngol 141(3):279–285. https://doi.org/10.1080/00016489.2020.1844288
Zhong B, Yuan T, Du J et al (2021) The role of preoperative blood eosinophil counts in distinguishing chronic rhinosinusitis with nasal polyps phenotypes. Int Forum Allergy Rhinol 11(1):16–23. https://doi.org/10.1002/alr.22636
Ikeda K, Shiozawa A, Ono N et al (2013) Subclassification of chronic rhinosinusitis with nasal polyp based on eosinophil and neutrophil. Laryngoscope 123(11):E1-9. https://doi.org/10.1002/lary.24154
Hu Y, Cao PP, Liang GT et al (2012) Diagnostic significance of blood eosinophil count in eosinophilic chronic rhinosinusitis with nasal polyps in Chinese adults. Laryngoscope 122(3):498–503. https://doi.org/10.1002/lary.22507
Acknowledgements
The authors would like to thank all the reviewers who participated in the review and MJEditor (www.mjeditor.com) for its linguistic assistance during the preparation of this manuscript.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by grants from the National Natural Science Foundation of China (81770978), Medicine and Health Science Technology Development Program of Shandong Province (202207010780), Qingdao Natural Science Foundation (23-2-1-199-zyyd-jch), Medicine and Health Science Technology Development Program of Qingdao (2021-WJZD175).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
This study was approved by the Medical Ethics Committee of the Affiliated Hospital of Qingdao University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, S., Zhang, Z., Wang, L. et al. Diagnostic significance of peripheral blood indices for eosinophilic chronic rhinosinusitis in Chinese adults. Eur Arch Otorhinolaryngol 281, 1337–1345 (2024). https://doi.org/10.1007/s00405-023-08324-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-08324-y