Abstract
Introduction
The most common sensorineural disorder in humans is hearing impairment and approximately 60% of prelingual hearing disorders are genetic. Especially parents with a congenital deaf child want to know as early as possible whether their second born child has the same genetic defect or not. The aim of this study is to demonstrate that postnatal genetic umbilical cord analysis is both the earliest detection possibility and sufficient.
Methods
We included first born children with severe hearing impairment that underwent cochlear implantation. All included patients were analyzed genetically and exhibited mutations of either DFNB1 loci or SLC26A4 gene. Additionally, the umbilical cord of the sibling underwent genetic analysis to detect hereditary genetic mutations as early as possible.
Results
49 newborn children out of 22 families were included in this study. Genetic analysis revealed clinical relevant mutations in all first born children and in four siblings via umbilical cord analysis. All patients who have been diagnosed with a relevant genetic mutation that caused severe hearing impairment underwent hearing rehabilitation via cochlear implant surgery.
Conclusion
This study demonstrates the sufficient and early as possible detection of known genetically hearing disorders via umbilical cord analysis. In case of a known familial genetic hearing disorder, it is advisable to analyze newborn siblings for the corresponding genetic defect as soon as possible, to be able to plan and initiate clinical care for the patient as early as possible. It is also extremely important for the parents to obtain clear information about the auditory status of the newborn.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
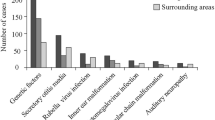
Hearing impairment is the most common sensorineural disorder in humans. Approximately 1–3/1000 newborns are affected by profound hearing impairment to deafness at birth or in the first years of life. The same number of children become deaf before reaching adulthood. The causes of severe hearing impairment are very heterogeneous. Based on the form of the physiological defect, hearing disorders are classified as conductive hearing loss, sensorineural hearing loss, or a combination of both. Reasons for hearing disorders may include environmental factors or viral infections, strong noise sources, ototoxic substances, and genetic causes. Hearing disorders can occur anytime in development and show a progressive course over several years from mild hearing loss to deafness [1, 2].
Approximately ~ 60% of all prelingual hearing disorders are genetic. Inherited hearing disorders are divided into syndromic or non-syndromic; non-syndromic hearing disorders (NSHL) occur in isolation, whereas syndromic hearing disorders (SHL) are associated with additional disorders. Nearly 70% of cases of inherited hearing loss are non-syndromic and predominantly due to sensorineural causes. Of these, about 80% of the cases follow an autosomal recessive (DFNB) and 18% an autosomal dominant (DFNA) mode of inheritance; about 2% are x-linked (DFNX) or mitochondrial linked (MT). A total of 193 gene loci have been described to date, for which 143 genes have been identified so far, and at least 50 genes are still unknown [3].
In most cases, NSHL is due to a monogenetic effect, i.e., one gene defect leads to the disease, but genetic heterogeneity is present. In a few cases, however, defects in multiple genes appear to be required to explain the pattern of inheritance.
Like NSHL, SHL has many different genetic causes. Syndromic hearing disorders are associated, for example, with malformations of the outer ear, inner ear, or petrous bone, and often are associated with other organic diseases, such as thyroid, renal dysfunction, or eye disease. To date, approximately 400 syndromes have been identified that are associated with hearing disorders. In many of these syndromes, hearing loss is mild to moderate and fluctuating, and some of these syndromes are very rare.
The locus DFNB1 [MIM 220290], localized in chromosomal segment 13q11-12, is caused by mutations in the gene GJB2 [MIM 121011] [4], which encodes connexin-26, and by deletions in the gene GJB6 (connexin-30) [MIM604418] [5].
Half of all cases of nonsyndromic recessive hearing impairment are due to alterations in this gene locus. This results in a prevalence rate of these heterozygous gene defects, at the DFNB1 gene locus of approximately 1/60 in the general population [6,7,8].
Pendred syndrome is one of the most common forms of genetic syndromic hearing disorders with about 1–8/100,000 cases. It is inherited in an autosomal recessive manner, clinically characterized by a sensorineural hearing disorder associated with thyroid dysfunction, which, however, occurs only at the beginning or in the middle of the second decade of life. Furthermore, a dilated aqueductus vestibuli (EVA = enlarged vestibular aqueduct) or Mondini dysplasia is present [1, 9]. Until now, changes in the gene SLC26A4 [MIM 605646] have been held responsible for the Pendred/EVA syndrome.
Our experience has shown that parents want to be informed as soon as possible whether their newborn child has the same genetic defect as their child with the genetical disease [10]. Previous studies could demonstrate that increased parenting stress leads to higher rates of behavior problems in both deaf and hearing children [11,12,13,14]. Parents of deaf children struggle with both communication difficulties, increased medical care and educational challenges [14, 15]. There are major stressors as concerns about the future of the child endorsed in parents of deaf children [14]. In this context, genetic analysis of umbilical cord tissue offers a simple and straightforward method to clarify the genetic status of the newborn as early as possible.
Materials and methods
We performed a retrospective analysis of second and third born siblings of genetically positive tested hearing impaired first born children out of 22 families at a quaternary university hospital and associated cochlear implant center, included between 2002 and 2022. All included first-born patients showed a severe hearing impairment in the first two years of life, so that a cochlear implant treatment was necessary.
We performed a genetic analysis of the gene locus DFNB1 in which the genes GJB2 (connexin-26) and GJB6 (connexin-30) are arranged in tandem orientation. In patients who had enlarged vestibular aqueduct on preliminary CI examination by high-resolution thin-slice CT, sequence analysis of the gene SLC26A4 (Pendrin) was performed as an alternative. Primers, PCR, and sequencing conditions were selected according to procedures described before [16, 17].
Immediately after birth of a sibling, a part of the umbilical cord (10–250 mg) was sent sterile to the molecular genetic laboratory of the University ENT Clinic Freiburg and promptly analyzed for the already known genetic defect of the sibling.
This study took place in the Department of Otorhinolaryngology, Head and Neck Surgery at the Implant Center of the University Hospital Freiburg. The study was approved by the Hospital’s Ethics Committee (local Ethics Committee of the Freiburg University) according to the Declaration of Helsinki (Washington, 2002) (Number of Ethics Committee approval, unlimited: (Number: 161/02, updated: 06/03)). Informed consent was obtained from all subjects and/or their legal guardian(s). The data that support the findings of this study are available from the department of otorhinolaryngology (Medical Center Freiburg) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of the Medical Center Freiburg and the local Ethics Committee of the Freiburg University.
Results
Bilateral severe hearing loss was diagnosed in 22 first born children in the first months of life. Inner ear malformations could be excluded in these cases by high-resolution computed tomography (CT) of the temporal bone. Two mutations were identified in 16 of the patients being homozygous carriers of the c.35delG mutation in the GJB2 gene (see Table 1). In five families (family 1, 4, 11, 12 and 15) the umbilical cord of two newborns each was analyzed. The patients in families 16 and 20 had early severe hearing impairment but no alteration in the DFNB gene locus, and the umbilical cord samples of the newborn siblings were accordingly not analyzed.
Three first born patients were diagnosed with Pendred syndrome and an enlarged vestibular aqueduct was confirmed radiologically (family 3, 4 and 6). Hearing loss was progressive in these patients. Two different mutations were identified in each of these three patients. The newborn sibling had no mutation in one case. In three cases a heterozygous mutation could be found.
Discussion
In the case of a proven genetic cause of hearing impairment, the affected families are interested in finding out soon after delivery to what extent their next born child is also affected by hearing impairment. The considerable emotional stress of the parents must also be taken into account in this context [18].
Practical experience shows newborn hearing screening (NHS) with OAE (otoacoustic emissions) or ABR (auditory brainstem response) is not always reliable. Especially in cases of progressive hearing loss, as is typical for Pendred syndrome, an unremarkable finding in newborn hearing screening can lead to a delay in diagnosis and thus treatment [19, 20].
In contrast, our results from eight cases (Table 1) clearly demonstrated that umbilical cord molecular genetic diagnosis is a simple and rapid method to obtain a definite result as soon as possible when genetic causes of hearing disorders are known in the family.
These analyses can be performed within 2–3 days. Only small amounts of the umbilical cord tissue are needed, 10 mg is approximately equivalent to the head of a pin. Ideally, the collection and shipment of umbilical cord tissue or blood is done in collaboration with the obstetrics department and no additional blood test is required.
On the one hand, mutation analysis of the umbilical cord tissue can rule out the disease and spare both the children and their parents other expensive and time-consuming diagnostic procedures. Alternatively, prenatal diagnosis can be applied to know the hearing status of the second child earlier. However, unlike umbilical cord diagnosis, this method poses a risk to both mother and child. A diagnosis one week after birth is early enough for hearing rehabilitation if necessary. If the condition is disclosed, all necessary steps can be taken to efficiently support speech development in the newborn. Furthermore, it is possible for the parents to be clear at an early stage that the hearing impairment is present or not.
Conclusion
In case of a known familial genetic hearing disorder, it is reasonable and easy to analyze newborn siblings for the corresponding genetic defect by umbilical cord analysis as soon as possible, to be able to plan and initiate clinical care for the patient as early as possible. It is also extremely important for the parents to obtain clear information about the health of the newborn.
Data availability
The data of this study are not openly available due to ethical reasons. The data are available from the corresponding author upon reasonable request.
References
Smith RJH, Jones MKN (2016) Nonsyndromic Hearing Loss and Deafness, DFNB1. 1998 Sep 28 [updated 2016 Aug 18]. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Stephens K, Amemiya A (eds) GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993–2019
Carpena NT, Lee MY (2018) Genetic hearing loss and gene therapy. Genomics Inform 16(4):e20
Kremer H (2019) Hereditary hearing loss; about the known and the unknown. Hear Res 376:58–68
Snoeckx RL, Huygen PL, Feldmann D et al (2005) GJB2 mutations and degree of hearing loss: a multicenter study. Am J Hum Genet 77:945–957
Kelsell DP, Dunlop J, Stevens HP et al (1997) Connexin 26 mutations in hereditary non-syndromic sensorineural deafness. Nature 387:80–83
Oonk AM, Huygen PL, Kunst HP, Kremer H, Pennings RJ (2016) Features of autosomal recessive non-syndromic hearing impairment: a review to serve as a reference. Clin Otolaryngol 41(5):487–497
Del Castillo FJ, Del Castillo I (2017) DFNB1 non-syndromic hearing impairment: diversity of mutations and associated phenotypes. Front Mol Neurosci 22(10):428
Zhou Y, Li C, Li M, Zhao Z, Tian S, Xia H, Liu P, Han Y, Ren R, Chen J, Jia C, Guo W (2019) Mutation analysis of common deafness genes among 1,201 patients with non-syndromic hearing loss in Shanxi Province. Mol Genet Genomic Med 28:e537
Van Camp G, Smith RJH. Hereditary hearing loss homepage. https://hereditaryhearingloss.org. Accessed July 2020
Richter B, Spahn C, Zschocke I et al (2000) Psychische Belastung, Informiertheit und Behandlungserwartung von Eltern mit einem Cochlear Implant versorgten Kind. HNO 48:675–683
Crnic K, Low C (2002) Everday stresses and parenting. In: Bornstein MH (ed) Handbook of Parenting: Practical Issues in Parenting, 2nd edn. Lawrence Erlbaum Associates, Mahwah, pp 243–268
Hintermair M (2006) Parental resources, parental stress, and socioemotional development of deaf and hard of hearing children. J Deaf Stud Deaf Educ 11(4):493–513
Lederberg AR, Everhart VS (2000) Conversations between deaf children and their hearing mothers: pragmatic and dialogic characteristics. J Deaf Stud Deaf Educ 5:303–322
Quittner AL, Barker DH, Cruz I et al (2010) Parenting stress among parents of deaf and hearing children: associations with language delays and behavior problems. Parent Sci Pract 10(2):136–155
Lederberg AR, Golbach T (2002) Parenting stress and social support in hearing mothers of deaf and hearing children: a longitudinal study. J Deaf Stud Deaf Educ 7:330–345
Birkenhäger R, Knapp FB, Klenzner T et al (2004) Identification of two heterozygous mutations in the SLC26A4 ⁄ PDS gene in a family with Pendred-syndrome. Laryngorhinootologie 83:831–835
Birkenhäger R, Zimmer AJ, Maier W et al (2006) Pseudodominants of two recessive connexin mutations in non-syndromic sensorineural hearing loss? Laryngorhinootologie 85:191–196
Burger T, Löhle E, Richter B et al (2008) ‘“Your child is hard of hearing”’—a longitudinal study of parental distress. Laryngorhinootologie 87:552–559
Morton CC, Nance WE (2006) Newborn hearing screening—a silent revolution. N Engl J Med 354:2151–2164
Prera N, Löhle E, Birkenhäger R (2014) Progressive hearing impairment with deletion in GJB2 gene despite normal newborn hearing screening. Laryngorhinootologie 93(4):244–248
Acknowledgements
The authors thank the Promotional Society “Taube Kinder lernen Hören e.V.”, which has supported the cochlear implant rehabilitation center in Freiburg for the past several years.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
MCK and RB analyzed data, provided statistical analysis and wrote the paper; RB provided critical revision; AA and SA performed the cochlear implant surgeries; MK performed the umbilical cord isolation; all coauthors provided critical revision.
Corresponding author
Ethics declarations
Conflict of interest
Manuel Christoph Ketterer declares no conflict of interest. Antje Aschendorff received travelling expenses and financial support for research from Cochlear Ltd, Australia; financial support for research and travelling expenses from Med-El, Innsbruck, Austria; financial support for research and travelling expenses from Oticon Inc., Somerset, NJ; financial support for research and travelling expenses from Advanced Bionics, Valencia, CA, USA. Susan Arndt received financial support for research and travelling expenses from Cochlear Ltd, Australia; financial support for research and travelling expenses from Med-El, Innsbruck, Austria travelling expenses from Advanced Bionics, Valencia, CA, USA; financial support for research and travelling expenses from Oticon Inc., Somerset, NJ. This study is not sponsored by industry.
Research involving human participants
No.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ketterer, M.C., Birkenhäger, R., Beck, R. et al. Postnatal genetic umbilical cord analysis for earliest possible detection of inherited hearing impairment. Eur Arch Otorhinolaryngol 280, 4811–4817 (2023). https://doi.org/10.1007/s00405-023-07986-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-07986-y