Abstract
Purpose
To analyze and stratify the possible risk factors of venous thromboembolism (VTE) in lateral skull base surgery (LSBS) using the Caprini risk assessment model.
Methods
In a single center, a retrospective study was conducted with patients who underwent LSBS from June 2016 to August 2021. The clinical characteristics and blood chemistry tests were collected. The incidence of VTE within 30 days of surgery was recorded. The Caprini risk score was calculated to assess the postoperative VTE risk.
Results
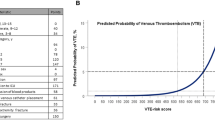
Among the 123 patients in this study, the VTE incidence within 30 postoperative days was 8.9%. The total Caprini risk score in VTE patients (5.6 ± 1.9 points) was significantly higher than that of non-VTE patients (4.6 ± 1.4 points; p = 0.028). The binary logistic regression showed the total Caprini score as the only independent indicator of postoperative VTE. The receiver operating characteristic curve analysis showed that the Caprini score at 6.5 points had low sensitivity (36.4%) but high specificity (91.1%), with the largest area under the curve being 0.659. The VTE rate was significantly higher in patients with a total Caprini score ≥ 7 points (28.6%) compared to those with a total Caprini score ≤ 6 points (7.3%; p = 0.022).
Conclusion
LSBS patients have a high risk of developing postoperative VTE. Patients with a Caprini score ≥ 7 points had a significantly higher risk of developing VTE after LSBS. The Caprini risk system was useful in assessing the VTE risk in LSBS. However, more data, calibration, and validation are necessary to establish an exclusive Caprini risk system for LSBS.

Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Gavriel H, Thompson E, Kleid S, Chan S, Sizeland A (2013) Safety of thromboprophylaxis after oncologic head and neck surgery. Study of 1018 patients. Head Neck 35:1410–1414. https://doi.org/10.1002/hed.23158
Cramer JD, Dilger AE, Schneider A, Smith SS, Samant S, Patel UA (2018) Risk of venous thromboembolism among otolaryngology patients vs general surgery and plastic surgery patients. JAMA Otolaryngol Head Neck Surg 144:9–17. https://doi.org/10.1001/jamaoto.2017.1768
Al-Qurayshi Z, Walsh J, Rodrigo B, Kandil E (2019) Venous thromboembolism in head and neck surgery: risk, outcome, and burden at the national level. Head Neck 41:411–422. https://doi.org/10.1002/hed.25409
Clayburgh DR, Stott W, Cordiero T, Park R, Detwiller K, Buniel M, Flint P, Schindler J, Andersen P, Wax MK, Gross N (2013) Prospective study of venous thromboembolism in patients with head and neck cancer after surgery. JAMA Otolaryngol Head Neck Surg 139:1143–1150. https://doi.org/10.1001/jamaoto.2013.4911
Tipirneni KE, Bauter L, Arnold MA, Audlin JA, Ryan J, Marzouk M (2021) Association of prolonged-duration chemoprophylaxis with venous thromboembolism in high-risk patients with head and neck cancer. JAMA Otolaryngol Head Neck Surg 147:320–328. https://doi.org/10.1001/jamaoto.2020.5151
Anderson BP, Sioshansi PC, Conway RM, Minutello K, Bojrab DI, Hong RS, Sargent EW, Schutt CA, Bojrab DI 2nd, Zappia JJ, Babu SC (2022) Rate of development of venous thromboembolism in lateral skull base surgery. Laryngoscope 132:662–667. https://doi.org/10.1002/lary.29889
Casazza GC, Bowers CA, MacDonald JD, Couldwell WT, Shelton C, Gurgel RK (2018) What is the safety and efficacy of chemical venous thromboembolism prophylaxis following vestibular schwannoma surgery? Otol Neurotol 39:e131–e136. https://doi.org/10.1097/mao.0000000000001633
Garritano FG, Lehman EB, Andrews GA (2013) Incidence of venous thromboembolism in otolaryngology-head and neck surgery. JAMA Otolaryngol Head Neck Surg 139:21–27. https://doi.org/10.1001/jamaoto.2013.1049
Innis WP, Anderson TD (2009) Deep venous thrombosis and pulmonary embolism in otolaryngologic patients. Am J Otolaryngol 30:230–233. https://doi.org/10.1016/j.amjoto.2008.06.004
Caprini JA (2005) Thrombosis risk assessment as a guide to quality patient care. Dis Mon 51:70–78. https://doi.org/10.1016/j.disamonth.2005.02.003
Bahl V, Hu HM, Henke PK, Wakefield TW, Campbell DA Jr, Caprini JA (2010) A validation study of a retrospective venous thromboembolism risk scoring method. Ann Surg 251:344–350. https://doi.org/10.1097/SLA.0b013e3181b7fca6
Guyatt GH, Akl EA, Crowther M, Gutterman DD, Schuünemann HJ (2012) Executive summary: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141:7s–47s. https://doi.org/10.1378/chest.1412S3
Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, Gibbs JS, Huisman MV, Humbert M, Kucher N, Lang I, Lankeit M, Lekakis J, Maack C, Mayer E, Meneveau N, Perrier A, Pruszczyk P, Rasmussen LH, Schindler TH, Svitil P, VonkNoordegraaf A, Zamorano JL, Zompatori M (2014) 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J 35:3033–3069. https://doi.org/10.1093/eurheartj/ehu283. (3069a-3069k)
Liew NC, Alemany GV, Angchaisuksiri P, Bang SM, Choi G, Da DES, Hong JM, Lee L, Li YJ, Rajamoney GN, Suviraj J, Tan TC, Tse E, Teo LT, Visperas J, Wong RS, Lee LH (2017) Asian venous thromboembolism guidelines: updated recommendations for the prevention of venous thromboembolism. Int Angiol 36:1–20. https://doi.org/10.23736/s0392-9590.16.03765-2
Ugo Fisch DM (1988) Microsurgery of the skull base. Georg Thieme Verlag Stuttgart, Thieme Medical Publishers, Inc., New York
Zanoletti E, Martini A, Emanuelli E, Mazzoni A (2012) Lateral approaches to the skull base. Acta Otorhinolaryngol Ital 32:281–287
Cramer JD, Shuman AG, Brenner MJ (2018) Antithrombotic therapy for venous thromboembolism and prevention of thrombosis in otolaryngology-head and neck surgery: state of the art review. Otolaryngol Head Neck Surg 158:627–636. https://doi.org/10.1177/0194599818756599
Khan NR, Patel PG, Sharpe JP, Lee SL, Sorenson J (2018) Chemical venous thromboembolism prophylaxis in neurosurgical patients: an updated systematic review and meta-analysis. J Neurosurg 129:906–915. https://doi.org/10.3171/2017.2.Jns162040
Gerlach R, Krause M, Seifert V, Goerlinger K (2009) Hemostatic and hemorrhagic problems in neurosurgical patients. Acta Neurochir (Wien) 151:873–900. https://doi.org/10.1007/s00701-009-0409-z
Algattas H, Damania D, DeAndrea-Lazarus I, Kimmell KT, Marko NF, Walter KA, Vates GE, Jahromi BS (2018) Systematic review of safety and cost-effectiveness of venous thromboembolism prophylaxis strategies in patients undergoing craniotomy for brain tumor. Neurosurgery 82:142–154. https://doi.org/10.1093/neuros/nyx156
Wang X, Zhang Y, Fang F, Jia L, You C, Xu P, Faramand A (2021) Comparative efficacy and safety of pharmacological prophylaxis and intermittent pneumatic compression for prevention of venous thromboembolism in adult undergoing neurosurgery: a systematic review and network meta-analysis. Neurosurg Rev 44:721–729. https://doi.org/10.1007/s10143-020-01297-0
MacLellan DG, Fletcher JP (2007) Mechanical compression in the prophylaxis of venous thromboembolism. ANZ J Surg 77:418–423. https://doi.org/10.1111/j.1445-2197.2007.04085.x
Bahl V, Shuman AG, Hu HM, Jackson CR, Pannucci CJ, Alaniz C, Chepeha DB, Bradford CR (2014) Chemoprophylaxis for venous thromboembolism in otolaryngology. JAMA Otolaryngol Head Neck Surg 140:999–1005. https://doi.org/10.1001/jamaoto.2014.2254
Shuman AG, Hu HM, Pannucci CJ, Jackson CR, Bradford CR, Bahl V (2012) Stratifying the risk of venous thromboembolism in otolaryngology. Otolaryngol Head Neck Surg 146:719–724. https://doi.org/10.1177/0194599811434383
Chang MT, Jitaroon K, Song S, Roozdar P, Wangworat Y, Ibrahim N, Ma Y, Rao VK, Chang SD, Fernandez-Miranda JC, Patel ZM, Dodd RL, Hwang PH, Harsh GR, Nayak JV (2022) Venous thromboembolism rates and risk factors following endoscopic skull base surgery. Int Forum Allergy Rhinol 12:935–941. https://doi.org/10.1002/alr.22943
Ali NE, Alyono JC, Song Y, Kouhi A, Blevins NH (2021) Postoperative venous thromboembolism after neurotologic surgery. J Neurol Surg B Skull Base 82:378–382. https://doi.org/10.1055/s-0039-3400223
Rinaldo L, Brown DA, Bhargav AG, Rusheen AE, Naylor RM, Gilder HE, Monie DD, Youssef SJ, Parney IF (2019) Venous thromboembolic events in patients undergoing craniotomy for tumor resection: incidence, predictors, and review of literature. J Neurosurg 132:10–21. https://doi.org/10.3171/2018.7.Jns181175
Ganau M, Prisco L, Cebula H, Todeschi J, Abid H, Ligarotti G, Pop R, Proust F, Chibbaro S (2017) Risk of Deep vein thrombosis in neurosurgery: State of the art on prophylaxis protocols and best clinical practices. J Clin Neurosci 45:60–66. https://doi.org/10.1016/j.jocn.2017.08.008
Di Nisio M, van Es N, Büller HR (2016) Deep vein thrombosis and pulmonary embolism. Lancet 388:3060–3073. https://doi.org/10.1016/s0140-6736(16)30514-1
Caprini JA, Arcelus JI, Hasty JH, Tamhane AC, Fabrega F (1991) Clinical assessment of venous thromboembolic risk in surgical patients. Semin Thromb Hemost 17(Suppl 3):304–312
Angchaisuksiri P (2016) Cancer-associated thrombosis in Asia. Thromb J 14:26. https://doi.org/10.1186/s12959-016-0110-4
Tham T, Rahman L, Persaud C, Olson C, Costantino P (2018) Venous thromboembolism risk in head and neck cancer: significance of the preoperative platelet-to-lymphocyte ratio. Otolaryngol Head Neck Surg 159:85–91. https://doi.org/10.1177/0194599818756851
Zhang Y, Cao M, Ren J (2021) NLR value and IL-18 level and their clinical significance in patients with deep vein thrombosis after receiving the surgery for spinal degeneration. Am J Transl Res 13:7156–7163
Kurtipek E, Büyükterzi Z, Büyükterzi M, Alpaydın MS, Erdem SS (2017) Endothelial dysfunction in patients with pulmonary thromboembolism: neutrophil to lymphocyte ratio and platelet to lymphocyte ratio. Clin Respir J 11:78–82. https://doi.org/10.1111/crj.12308
Acknowledgements
We would like to thank all the patients for allowing us to review their medical findings and records.
Funding
This work was supported by National High Level Hospital Clinical Research Funding (2022-PUMCH-B-095).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declared no conflicts of interest, financial, or otherwise.
Ethical approval
This study was exempted from the Institutional Review Board (IRB) review by the Medical Ethics Committee of Peking Union Medical College Hospital (S-K1806).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sun, H., Xue, S., Huang, Y. et al. Stratifying the risks of venous thromboembolism in the lateral skull base surgery using Caprini risk assessment model. Eur Arch Otorhinolaryngol 280, 3219–3228 (2023). https://doi.org/10.1007/s00405-023-07984-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-07984-0