Abstract
Purpose
There is no guidance surrounding postoperative venous thromboembolism (VTE) prophylaxis using pharmacological agents (chemoprophylaxis) in patients undergoing skull base surgery. The aim of this study was to compare VTE and intracranial haematoma rates after skull base surgery in patients treated with/without chemoprophylaxis.
Methods
Review of prospective quaternary centre database including adults undergoing first-time skull base surgery (2009–2020). VTE was defined as deep vein thrombosis (DVT) and pulmonary embolism (PE) within 6 months of surgery. Multivariate logistic regression was used to determine factors predictive of postoperative intracranial haematoma/VTE. Propensity score matching (PSM) was used in group comparisons.
Results
One thousand five hundred fifty-one patients were included with a median age of 52 years (range 16–89 years) and female predominance (62%). Postoperative chemoprophylaxis was used in 81% of patients at a median of 1 day postoperatively. There were 12 VTE events (1.2%), and the use of chemoprophylaxis did not negate the risk of VTE entirely (p > 0.99) and was highest on/after postoperative day 6 (9/12 VTE events). There were 18 intracranial haematomas (0.8%), and after PSM, chemoprophylaxis did not significantly increase the risk of an intracranial haematoma (p > 0.99). Patients administered chemoprophylaxis from postoperative days 1 and 2 had similar rates of intracranial haematomas (p = 0.60) and VTE (p = 0.60), affirmed in PSM.
Conclusion
Postoperative chemoprophylaxis represents a relatively safe strategy in patients undergoing skull base surgery. We advocate a personalised approach to chemoprophylaxis and recommend it on postoperative days 1 or 2 when indicated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Venous thromboembolism (VTE) is the composite of deep vein thrombosis (DVT) and pulmonary embolism (PE), which are serious and potentially fatal postoperative complications. Such complications are potentially preventable. The risk of VTE can be reduced through mechanical thromboprophylaxis with compression stockings and intermittent pneumatic compression, along with pharmacological thromboprophylaxis (chemoprophylaxis). These measures are often used in conjunction as there is limited evidence for mechanical thromboprophylaxis alone [6, 21]. In contrast, there is strong evidence of benefit for chemoprophylaxis in hospitalised patients [19], though data for patients undergoing intracranial surgery are limited.
The American Heart Association recommends against using chemoprophylaxis in patients undergoing major neurosurgical procedures, except in those deemed at high risk, such as those experiencing prolonged immobility [5]. These guidelines are open to interpretation and do not specifically address skull base surgery, which is also the case for European guidelines [3]. In the UK, the National Institute for Health and Care Excellence (NICE) guidelines suggest initiation of chemoprophylaxis 24–48 h after cranial surgery where benefits outweigh risks [20]. As such, decision-making surrounding chemoprophylaxis must be made on a case-by-case basis by balancing the benefits of VTE reduction with the potentially increased risk of bleeding events. Meta-analyses and prior institutional series including neurosurgical patients from different subspecialties have demonstrated that pharmacological thromboprophylaxis with heparin agents can be used postoperatively to decrease the rate of VTE with minimal risk of bleeding [4, 10, 11, 14, 16, 23]. However, there is sparse outcome data for patients undergoing skull base surgery. In this cohort of patients, the potential risks of chemoprophylaxis include postoperative haematoma with serious associated morbidity due to the proximity of the brainstem, optic nerves and critical neurovascular structures. This must be balanced against the VTE risk inferred by the long operative times in this patient group, reported as an independent risk factor for VTE in population-based studies [17]. Indeed, the VTE risk in skull base patients can be as high as 10% [2].
We recently presented data on the benefits of early chemoprophylaxis in patients undergoing trans-sphenoidal pituitary surgery [25]. Patients undergoing skull base surgery represent a distinct cohort from these patients, given that their operative time is significantly longer, with greater intra-arachnoid brain and vessel manipulation. It is therefore important to present data in this specific patient group. Our institution represents a quaternary and national referral centre for skull base pathology in the United Kingdom. The aims of this study were to describe our experience of chemoprophylaxis following skull base surgery, to describe the absolute risks of haematoma/VTE events in patients treated with/without chemoprophylaxis and to provide guidance and recommendations from our experience.
Methods
Institutional review board approval was obtained. Patient consent was not required for this study type. We interrogated a prospectively maintained electronic database of locally performed skull base operations. All adults (age ≥ 16 years) undergoing first-time skull base surgery between April 2009 and December 2020 were included. Patients with redo operations were excluded. Patients undergoing trans-sphenoidal pituitary operations were also excluded from this study and analysed separately [25].
Electronic patient records were reviewed and data extracted on demographics, histological diagnosis, operative intervention, postoperative course (including use of chemoprophylaxis) and the development of VTE or postoperative haematomas. We defined VTE as that occurring within 6 months of surgery. This encompassed DVT and PE. The time limitation to our definition of VTE excluded only one upper limb deep vein thrombosis that occurred two years postoperatively from total VTE events. In accordance with national standards and the National Health Service contract, the institution thrombosis committee maintains a separate electronic and prospectively maintained database of VTE-positive events occurring during hospital admission or after hospital discharge, following inpatient admission (Hospital acquired thrombosis). This dataset was cross-referenced to identify any missed VTE events within the included cohort.
At our institution, antiplatelet medication is discontinued 1 week prior to surgery. Anticoagulant medication is discontinued 5 days (warfarin) or 48 h (novel oral anticoagulants) before surgery. Postoperatively, patients are nursed in a specialist monitored bed for at least 24 h. Patients are encouraged to mobilise postoperatively, and there are no bed rest restrictions. The decision to commence postoperative chemoprophylaxis is made after the procedure on daily patient rounds. Potential factors that can influence this decision and the exact day of commencement (e.g. postoperative day 1 vs. subsequent days vs. not at all) include the degree of difficulty encountered with intraoperative haemostasis, coagulation state, preoperative comorbidities and antiplatelet/anticoagulant use and patient mobility.
The preferred low molecular weight heparin (LMWH) agent at our institute is tinzaparin, with dose adjustment to weight and renal function, administered subcutaneously once daily at 1800 h. Chemoprophylaxis is used together with mechanical prophylaxis at our institute; all patients had mechanical prophylaxis with Flowtron® boots (intraoperatively) and TED stockings from hospital admission to discharge as per our institutional protocol. Chemoprophylaxis was discontinued on the day of discharge, with no routine discharge course.
Imaging is not routinely performed in the immediate postoperative period unless clinically indicated. Therefore, postoperative haematomas described in the present study were clinically detected (e.g. with a deterioration in neurology for intracranial haematomas) and confirmed with subsequent imaging where relevant.
Statistical analysis was performed in R version 4.0.5 (R Foundation for Statistical Computing; Vienna, Austria). Descriptive statistics were used to describe patient cohort characteristics. Categorical variables were compared using tests of proportions (Fisher’s exact and Chi-squared). Forward-stepwise multivariate logistic regression was performed to evaluate factors predictive of postoperative intracranial/any haematoma formation. Propensity score matching was used to compare patient groups (chemoprophylaxis versus no chemoprophylaxis and chemoprophylaxis on postoperative day 1 versus day 2) to create 1:1 matching cohorts based age, gender, prior antiplatelet/anticoagulant use, procedure type and surgical approach.
Results
One thousand five hundred fifty-one patients were included. Patient characteristics are shown in Table 1. The median age was 52 years (range 16–89 years). There was a female predominance (N = 955, 62%). Antiplatelets and anticoagulants were used by 7% of patients overall. The most common skull base surgical approaches included retrosigmoid (N = 538, 35%) and translabyrinthine/transmastoid (N = 514, 33%). The majority of procedures were performed for oncological lesions (N = 926, 60%) or microvascular decompression (N = 370, 24%).
Postoperative chemoprophylaxis was used in the majority of patients (N = 1249, 81%) at a median of 1 day postoperatively (range 1–16 days). Indeed, 81% of cases (1014/1249) had chemoprophylaxis commenced on the first postoperative day. Chemoprophylaxis was employed with tinzaparin (1217, 97%; median dose 4500 units once daily) or enoxaparin (32, 3%; median dose 40 mg once daily). The median duration of chemoprophylaxis was 4 days (range 1–217 days), and chemoprophylaxis was routinely discontinued at discharge.
Within the study period, there was a change in practice from infrequent use of postoperative chemoprophylaxis (2009–2011, chemoprophylaxis used in 157/360 patients, 44%) to more routine use (2018–2020, chemoprophylaxis used in 312/329 patients, 95%).
Table 2 shows differences between patients who did/did not receive chemoprophylaxis. The chemoprophylaxis group had significantly more oncology cases (63% vs. 44%), whereas the no chemoprophylaxis group had a relative excess of foramen magnum decompressions (10% vs. 16%; Chi-squared, χ2 = 38.3, p < 0.001). There were also more frontal/pterional approaches in the chemoprophylaxis group (11% vs. 4%; Chi-squared, χ2 = 26.1, p < 0.001).
Postoperative haematomas
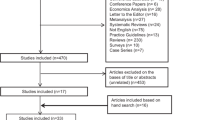
There were 31 postoperative haematomas, of which 18 were intracranial (0.8% incidence; Fig. 1). A summary of patients that sustained postoperative intracranial haematomas is displayed in Supplementary Table 1. The median time from operation date to diagnosis of an intracranial haematoma was 2 days (range 0–11 days). Management was either surgery (10/18, 56%) or conservative (8/18, 44%).
Postoperative risk of intracranial haematoma and venous thromboembolism after skull base surgery. This figure summarises the study results overall. In a cohort of 1551 patients undergoing first-time skull base surgery, the overall risk of haematoma formation was 1.2% and the risk of a DVT/PE was 0.8%. Chemoprophylaxis was used in 80.5% of patients and did not negate the risk of VTE events overall
Table 3 displays factors that were predictive of postoperative intracranial haematoma. In multivariate analysis, prior chemoprophylaxis was associated with a significantly reduced incidence of postoperative intracranial haematoma formation (p < 0.001), and oncological pathology was associated with a significantly increased incidence (p < 0.001). Analysis including other haematoma types is provided in Supplementary Table 2 and affirmed these associations.
The mortality rate of patients with haematomas was 2/31. One of these occurred in a patient that had translabyrinthine removal of a vestibular schwannoma that sustained a superficial skin haematoma that was surgically evacuated, but deteriorated from hydrocephalus that was unrelated. The second patient underwent a retrosigmoid craniotomy for a petrous meningioma and sustained an intracranial haematoma on postoperative day 1, which was surgically evacuated, without having ever received chemoprophylaxis, and died on postoperative day 4.
Venous thromboembolism
There were 12 VTE events overall (1.2%; Fig. 1) within 6 months of surgery including 3 DVTs and 9 PEs. A summary of patients that sustained a VTE event is provided in Supplementary Table 3 and included a single case that sustained a PE within 24 h of surgery, prior to commencement of chemoprophylaxis. The median time from operation date to diagnosis was 8 days (range 1–201 days). Prior use of chemoprophylaxis did not significantly influence the rate of VTE formation (Fisher’s exact, p > 0.99). No VTE event was fatal.
Chemoprophylaxis risk–benefit analysis
Propensity scoring was used to match 302 patients treated with/without chemoprophylaxis (Supplementary Table 4). This data re-affirmed the relative safety of chemoprophylaxis with equivalent rates of intracranial haematomas (p > 0.99) and VTE events (p > 0.99).
Figure 2 displays the number of intracranial haematomas and VTE events diagnosed on each postoperative day. The use of chemoprophylaxis did not negate the risk of VTE entirely and was highest on/after postoperative day 6 (9/12 VTE events).
Longitudinal risk of postoperative intracranial haematoma and VTE after skull base surgery. This figure displays the number of intracranial haematomas and VTE events after each successive postoperative day (POD). Data are displayed separately for A all patients, B patients in whom chemoprophylaxis was commenced on POD1 and C patients in whom chemoprophylaxis was commenced on POD2. There was no significant difference in the overall rate of post-chemoprophylaxis intracranial haematomas between patients commenced on chemoprophylaxis on POD1 versus POD2 (Fisher’s exact, p = 0.60). This data also demonstrates a relatively low rate of VTE overall that was not negated entirely with chemoprophylaxis
The risk of intracranial haematoma formation was particularly high in the first 48 h after surgery. Then, 10/18 (56%) intracranial haematomas occurred within 48 h of surgery, of which 6/10 required surgical intervention (Supplementary Table 1). This is compared to 4/8 patients requiring surgery for intracranial haematomas occurring beyond 48 h (Supplementary Table 1).
Chemoprophylaxis on postoperative day 1 versus 2
The overall rate of post-chemoprophylaxis intracranial haematoma formation was equivalent between patients administered chemoprophylaxis from postoperative day 1 (7/1013, 0.7%) and postoperative day 2 (1/123, 0.8%; Fisher’s exact, p = 0.60). The overall rate of post-chemoprophylaxis VTE was also similar for these groups, respectively (6/1013, [0.6%] vs. 1/123 [0.8%], Fisher’s exact, p = 0.60).
Propensity scoring was used to match 123 patients treated with chemoprophylaxis on postoperative days 1 and 2 (Supplementary Table 5). The rate of post-chemoprophylaxis intracranial haematomas was not significantly different between postoperative day 1 (0/123) versus day 2 (1/123, 1%; Fisher’s exact, p > 0.99). The rates of VTE were also comparable between postoperative day 1 (1/123, 1%) versus day 2 (1/123, 1%; Fisher’s exact, p > 0.99).
Discussion
In this novel study, we presented data on haematoma and VTE risk after skull base surgery. In a large cohort of 1551 patients, of which over half had oncological pathology, chemoprophylaxis was used in 80% of patients usually from the first postoperative day. The overall risks of postoperative intracranial haematoma and VTE were 1.2% and 0.8%, respectively. The overall rate of VTE was relatively low and not negated entirely even with chemoprophylaxis. Use of chemoprophylaxis was safe and associated with a reduced overall risk of postoperative intracranial haematoma formation, which was highest in the first 48 h of surgery. We further presented data on the risks/benefits of chemoprophylaxis on different postoperative days and found equivalent outcomes when chemoprophylaxis was commenced on postoperative day 1 versus 2.
The proportion of patients receiving chemoprophylaxis in the present study was much greater than other large neuro-oncological series describing rates of 30–40% that have also found a tendency for a lower rate of chemoprophylaxis with primary brain tumours [26]. The widespread reluctance to use chemoprophylaxis routinely in patients undergoing intracranial surgery is likely due to the perceived risks of postoperative intracranial haematomas, which can be associated with significant morbidity, especially in skull base patients. Indeed, in the traditional sense, the possibility of a potentially fatal PE (0% incidence in the present series) has to be weighed up against the possibility of a fatal/life-changing haematoma (< 1% incidence). In some centres, postoperative imaging is routinely employed to guide decision-making relating to postoperative chemoprophylaxis. However, our data demonstrates the relative safety of chemoprophylaxis from the first postoperative day based on clinical grounds without the use of routine imaging. Indeed, patients in whom it was utilised had a reduced incidence of postoperative intracranial haematomas. In a retrospective analysis, this finding could be attributed to use in patients with a lower perceived risk of developing a haematoma, so we place greater emphasis on our propensity-score matched outcomes.
There was a relatively low rate of intracranial haematomas in the present series despite the relatively high utilisation of chemoprophylaxis. Other studies have reported a higher rate of haematomas ranging from 2 to 4%, albeit with different intracranial pathologies [13]. Mortality that was potentially attributable to an intracranial haematoma occurred only in a single case, and there was no mortality attributable to an intracranial haematoma in a patient that received chemoprophylaxis. Overall, therefore, our data demonstrates that, in patients who make it to their first postoperative day without bleeding-related complication, chemoprophylaxis is safe but can also be deferred to the second postoperative day. This is because we observed the highest incidence of intracranial haematomas within the first 48 h of surgery. In patients in whom chemoprophylaxis is contraindicated or deemed too risky, the risk of VTE remains low with mechanical measures alone. We only found oncological pathology as a baseline variable that increased the risk of an intracranial haematoma, but other intraoperative factors (e.g. haemostasis/procedural time and surgical adjuncts) could also be contributory given the timing of most haematomas and should be explored in future [22]. Our data support a personalised approach to chemoprophylaxis in patients undergoing skull base surgery (Fig. 3). This is a useful resource given the lack of dedicated postoperative VTE prophylaxis protocols in different neurosurgical pathologies [13]. Developing such tools is useful given the strong rationale for tailoring postoperative VTE prophylaxis in surgical patients [18].
Chemoprophylaxis after skull base surgery. Skull base procedures are associated with an elevated but relatively low risk of VTE, which is apparent from postoperative day 1 and not negated entirely even with chemoprophylaxis. Chemoprophylaxis represents a safe strategy to utilise in this patient group. Chemoprophylaxis is discouraged on the day of surgery given the elevated early risk of spontaneous intracranial haematomas. An individualised risk assessment should occur on postoperative day 1. If chemoprophylaxis is indicated, it can be commenced on postoperative day 1 or 2, which have comparable safety and efficacy profiles. If chemoprophylaxis is not indicated or contraindicated, patients should be offered mechanical thromboprophylaxis measures alone, which still result in a relatively low rate of VTE. We do not advocate post-discharge chemoprophylaxis. Abbreviations: POD, postoperative day
The rate of VTE in this series was relatively low, although not negligible given the occurrence of VTE events prior to commencement of chemoprophylaxis and the occurrence of VTE events whilst on chemoprophylaxis. This is likely multifactorial and could be attributed to the significant duration of skull base procedures, the high incidence of oncological pathology and requirement for postoperative high-dependency care that itself can involve prolonged immobility. Our data therefore supports prior studies reporting an elevated VTE risk after prolonged (> 45 min) surgery for oncological pathology [8]. Our reported rates of VTE are also in keeping with prior meta-analyses describing reduction in VTE after chemoprophylaxis [14, 24]. This also corroborates our experience with trans-sphenoidal pituitary surgery where a similarly high rate of chemoprophylaxis (73%) yielded zero VTE events in 651 patients within 3 months of surgery [25]. Notably, our VTE rate was also lower than a prior series that utilised delayed postoperative chemoprophylaxis after 72 h in skull base patients, reporting a VTE rate of 10% through serial venous Doppler ultrasound scans [2]. We also only reported data on acquired VTE as defined by DVT/PE, not including cerebral venous sinus thrombosis, which is attributed to surgery near dural venous sinuses and therefore has a high incidence in this patient group [1, 9].
We do not employ post-discharge chemoprophylaxis for skull base patients. This practise is utilised in some patient groups postoperatively for a limited time period when the rates of VTE are particularly high/patient mobility is affected by surgery [7]. Our data does not support this practise for skull base surgery as at least 25% of VTE events occurred beyond 4 weeks—which may be considered a reasonable time period to offer post-discharge chemoprophylaxis (Supplementary Table 3). Furthermore, our patient demographic tends to be fully mobile in the weeks following surgery.
Limitations of the present study include its single-centre design and retrospective data extraction, albeit with interrogation of prospective databases. Over the study period, there was a change in practice towards increased VTE prophylaxis, and bias from this effect was minimised using propensity score matching. Matched comparisons between patients did not consider intention to treat. Factors that therefore determined the decision to commence chemoprophylaxis at all or on postoperative day 1 versus 2 were not clear. Data were not available on variables that are associated with VTE risk such as diabetes mellitus, body mass index, ethnicity, and smoking history [12, 15].
Conclusion
In this study which represents the first of its kind, we described the benefits and risks of chemical thromboembolism prophylaxis (chemoprophylaxis) after skull base surgery. Skull-base procedures are associated with a relatively low risk (0.8%) of VTE in our cohort. There is also a low rate of postoperative intracranial haematomas (1.2%), which are most likely to occur in the first 48 h of surgery. Chemoprophylaxis represents a safe strategy to reduce the risk of DVT/PE without significantly increasing the risk of postoperative haematoma. Our data demonstrates similar VTE/intracranial haematoma rates between patients commenced on chemoprophylaxis from postoperative day 1 versus 2. We therefore support a personalised approach to chemoprophylaxis, considering it from postoperative days 1 or 2 when indicated. Future studies should consider the timing of chemoprophylaxis in relation to the VTE/haematoma risk in this patient group.
Data availability
Not applicable.
Code availability
Not applicable.
References
Abou-Al-Shaar H, Gozal YM, Alzhrani G, Karsy M, Shelton C, Couldwell WT (2018) Cerebral venous sinus thrombosis after vestibular schwannoma surgery: a call for evidence-based management guidelines. Neurosurg Focus 45:E4. https://doi.org/10.3171/2018.4.FOCUS18112
Abunimer AM, Lak AM, Calvachi P, Smith TR, Aglio LS, Almefty KK, Dunn IF, Bi WL, Goldhaber SZ, Al-Mefty O (2022) Early detection and management of venous thrombosis in skull base surgery: role of routine doppler ultrasound monitoring. Neurosurgery 91:115–122. https://doi.org/10.1227/neu.0000000000001936
Afshari A, Ageno W, Ahmed A, Duranteau J, Faraoni D, Kozek-Langenecker S, Llau J, Nizard J, Solca M, Stensballe J, Thienpont E, Tsiridis E, Venclauskas L, Samama CM, Force EVGT (2018) European guidelines on perioperative venous thromboembolism prophylaxis: executive summary. Eur J Anaesthesiol 35:77–83. https://doi.org/10.1097/EJA.0000000000000729
Alshehri N, Cote DJ, Hulou MM, Alghamdi A, Alshahrani A, Mekary RA, Smith TR (2016) Venous thromboembolism prophylaxis in brain tumor patients undergoing craniotomy: a meta-analysis. J Neurooncol 130:561–570. https://doi.org/10.1007/s11060-016-2259-x
Anderson DR, Morgano GP, Bennett C, Dentali F, Francis CW, Garcia DA, Kahn SR, Rahman M, Rajasekhar A, Rogers FB, Smythe MA, Tikkinen KAO, Yates AJ, Baldeh T, Balduzzi S, Brozek JL, Ikobaltzeta IE, Johal H, Neumann I, Wiercioch W, Yepes-Nunez JJ, Schunemann HJ, Dahm P (2019) American Society of Hematology 2019 guidelines for management of venous thromboembolism: prevention of venous thromboembolism in surgical hospitalized patients. Blood Adv 3:3898–3944. https://doi.org/10.1182/bloodadvances.2019000975
Arabi YM, Al-Hameed F, Burns KEA, Mehta S, Alsolamy SJ, Alshahrani MS, Mandourah Y, Almekhlafi GA, Almaani M, Al Bshabshe A, Finfer S, Arshad Z, Khalid I, Mehta Y, Gaur A, Hawa H, Buscher H, Lababidi H, Al Aithan A, Abdukahil SAI, Jose J, Afesh LY, Al-Dawood A, Trials SCC, G, (2019) Adjunctive intermittent pneumatic compression for venous thromboprophylaxis. N Engl J Med 380:1305–1315. https://doi.org/10.1056/NEJMoa1816150
Arcelus JI, Kudrna JC, Caprini JA (2006) Venous thromboembolism following major orthopedic surgery: what is the risk after discharge? Orthopedics 29:506–516. https://doi.org/10.3928/01477447-20060601-16
Bahl V, Hu HM, Henke PK, Wakefield TW, Campbell DA Jr, Caprini JA (2010) A validation study of a retrospective venous thromboembolism risk scoring method. Ann Surg 251:344–350. https://doi.org/10.1097/SLA.0b013e3181b7fca6
Benjamin CG, Sen RD, Golfinos JG, Sen C, Roland JT, McMenomey S, Pacione D (2018) Postoperative cerebral venous sinus thrombosis in the setting of surgery adjacent to the major dural venous sinuses. J Neurosurg 1–7. https://doi.org/10.3171/2018.4.JNS18308
Chang R, Scerbo MH, Schmitt KM, Adams SD, Choi TJ, Wade CE, Holcomb JB (2017) Early chemoprophylaxis is associated with decreased venous thromboembolism risk without concomitant increase in intraspinal hematoma expansion after traumatic spinal cord injury. J Trauma Acute Care Surg 83:1088–1094. https://doi.org/10.1097/TA.0000000000001675
Chibbaro S, Cebula H, Todeschi J, Fricia M, Vigouroux D, Abid H, Kourbanhoussen H, Pop R, Nannavecchia B, Gubian A, Prisco L, Ligarotti GKI, Proust F, Ganau M (2018) Evolution of prophylaxis protocols for venous thromboembolism in neurosurgery: results from a prospective comparative study on low-molecular-weight heparin, elastic stockings, and intermittent pneumatic compression devices. World Neurosurg 109:e510–e516. https://doi.org/10.1016/j.wneu.2017.10.012
Dengler BA, Mendez-Gomez P, Chavez A, Avila L, Michalek J, Hernandez B, Grandhi R, Seifi A (2016) Safety of chemical DVT prophylaxis in severe traumatic brain injury with invasive monitoring devices. Neurocrit Care 25:215–223. https://doi.org/10.1007/s12028-016-0280-8
Ganau M, Prisco L, Cebula H, Todeschi J, Abid H, Ligarotti G, Pop R, Proust F, Chibbaro S (2017) Risk of deep vein thrombosis in neurosurgery: state of the art on prophylaxis protocols and best clinical practices. J Clin Neurosci 45:60–66. https://doi.org/10.1016/j.jocn.2017.08.008
Hamilton MG, Yee WH, Hull RD, Ghali WA (2011) Venous thromboembolism prophylaxis in patients undergoing cranial neurosurgery: a systematic review and meta-analysis. Neurosurgery 68:571–581. https://doi.org/10.1227/NEU.0b013e3182093145
Jacobs LJ, Woods BI, Chen AF, Lunardini DJ, Hohl JB, Lee JY (2013) Safety of thromboembolic chemoprophylaxis in spinal trauma patients requiring surgical stabilization. Spine (Phila Pa 1976) 38:E1041–1047. https://doi.org/10.1097/BRS.0b013e31829879cc
Khan NR, Patel PG, Sharpe JP, Lee SL, Sorenson J (2018) Chemical venous thromboembolism prophylaxis in neurosurgical patients: an updated systematic review and meta-analysis. J Neurosurg 129:906–915. https://doi.org/10.3171/2017.2.JNS162040
Kim JY, Khavanin N, Rambachan A, McCarthy RJ, Mlodinow AS, De Oliveria GS Jr, Stock MC, Gust MJ, Mahvi DM (2015) Surgical duration and risk of venous thromboembolism. JAMA Surg 150:110-117. https://doi.org/10.1001/jamasurg.2014.1841
Lobastov K, Sautina E, Alencheva E, Bargandzhiya A, Schastlivtsev I, Barinov V, Laberko L, Rodoman G, Boyarintsev V (2021) Intermittent pneumatic compression in addition to standard prophylaxis of postoperative venous thromboembolism in extremely high-risk patients (IPC SUPER): a randomized controlled trial. Ann Surg 274:63–69. https://doi.org/10.1097/SLA.0000000000004556
Mismetti P, Laporte-Simitsidis S, Tardy B, Cucherat M, Buchmuller A, Juillard-Delsart D, Decousus H (2000) Prevention of venous thromboembolism in internal medicine with unfractionated or low-molecular-weight heparins: a meta-analysis of randomised clinical trials. Thromb Haemost 83:14–19
NICE Venous thromboembolism in over 16s: reducing the risk of hospital-acquired deep vein thrombosis or pulmonary embolism. https://www.nice.org.uk/guidance/ng89/chapter/Recommendations#interventions-for-people-having-elective-spinal-surgery-or-cranial-surgery-or-people-with-spinal. Accessed 23rd June 2020
Shalhoub J, Lawton R, Hudson J, Baker C, Bradbury A, Dhillon K, Everington T, Gohel MS, Hamady Z, Hunt BJ, Stansby G, Warwick D, Norrie J, Davies AH, investigators Gt (2020) Graduated compression stockings as adjuvant to pharmaco-thromboprophylaxis in elective surgical patients (GAPS study): randomised controlled trial. BMJ 369:m1309. https://doi.org/10.1136/bmj.m1309
Takami M, Yoshida M, Minamide A, Hashizume H, Yukawa Y, Nakagawa Y, Iwasaki H, Tsutsui S, Nagata K, Taiji R, Nishi H, Schoenfeld AJ, Simpson AK, Yamada H (2021) Does prophylactic use of topical gelatin-thrombin matrix sealant affect postoperative drainage volume and hematoma formation following microendoscopic spine surgery? A randomized controlled trial. Spine J 21:446–454. https://doi.org/10.1016/j.spinee.2020.11.004
Tanweer O, Boah A, Huang PP (2013) Risks for hemorrhagic complications after placement of external ventricular drains with early chemical prophylaxis against venous thromboembolisms. J Neurosurg 119:1309–1313. https://doi.org/10.3171/2013.7.JNS13313
Wang X, Zhang Y, Fang F, Jia L, You C, Xu P, Faramand A (2021) Comparative efficacy and safety of pharmacological prophylaxis and intermittent pneumatic compression for prevention of venous thromboembolism in adult undergoing neurosurgery: a systematic review and network meta-analysis. Neurosurg Rev 44:721–729. https://doi.org/10.1007/s10143-020-01297-0
Waqar M, Chadwick A, Kersey J, Horner D, Kearney T, Karabatsou K, Gnanalingham KK, Pathmanaban ON (2021) Venous thromboembolism chemical prophylaxis after endoscopic trans-sphenoidal pituitary surgery. Pituitary. https://doi.org/10.1007/s11102-021-01195-8
Zacharia BE, Youngerman BE, Bruce SS, Hershman DL, Neugut AI, Bruce JN, Wright JD (2017) Quality of postoperative venous thromboembolism prophylaxis in neuro-oncologic surgery. Neurosurgery 80:73–81. https://doi.org/10.1227/NEU.0000000000001270
Acknowledgements
The authors would like to thank Dr. Calvin Heal, Centre for Biostatistics, The University of Manchester for oversight in relation to propensity-score matching in this study.
Author information
Authors and Affiliations
Contributions
Data collection: MW, OY, AC, JL and GK. Data analysis: MW, OY, AC, AJ, AF, DGE, SL, RB, CHW, SAR, ATK, and ONP. Drafting first version: MW, OY, DJ, AJ, SF, RB, SL and ONP. Editing of final submitted version: all authors. Concept and supervision: DGE, DH, DJ, SF, RB, SL, CHW, SAR, ATK and ONP.
Corresponding author
Ethics declarations
Ethics approval
Not required for this study type. Institutional review board approval is obtained.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mueez Waqar and Omar Yaseen denote joint first authorship.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Waqar, M., Yaseen, O., Chadwick, A. et al. Venous thromboembolism chemical prophylaxis after skull base surgery. Acta Neurochir 166, 165 (2024). https://doi.org/10.1007/s00701-024-06035-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00701-024-06035-9