Abstract
Purpose
Arterial hypertension (AHTN), type 2 diabetes mellitus (DM), and atherosclerotic vascular disease (ASVD) are common vascular comorbidities in patients undergoing reconstruction of the head and neck region with a microvascular free flap. These conditions may affect flap perfusion (microvascular blood flow and tissue oxygenation), which is a prerequisite for flap survival and thus reconstruction success. This study aimed to investigate the impacts of AHTN, DM, and ASVD on flap perfusion.
Methods
Data from 308 patients who underwent successful reconstruction of the head and neck region with radial free forearm flaps, anterolateral thigh flaps, or fibula free flaps between 2011 and 2020 were retrospectively analyzed. Flap perfusion was measured intraoperatively and postoperatively with the O2C tissue oxygen analysis system. Flap blood flow, hemoglobin concentration, and hemoglobin oxygen saturation were compared between patients with and without AHTN, DM, and ASVD.
Results
Intraoperative hemoglobin oxygen saturation and postoperative blood flow were lower in patients with ASVD than in patients without ASVD (63.3% vs. 69.5%, p = 0.046; 67.5 arbitrary units [AU] vs. 85.0 AU, p = 0.036; respectively). These differences did not persist in the multivariable analysis (all p > 0.05). No difference was found in intraoperative or postoperative blood flow or hemoglobin oxygen saturation between patients with and without AHTN or DM (all p > 0.05).
Conclusion
Perfusion of microvascular free flaps used for head and neck reconstruction is not impaired in patients with AHTN, DM, or ASVD. Unrestricted flap perfusion may contribute to the observed successful use of microvascular free flaps in patients with these comorbidities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Reconstruction of the head and neck region with microvascular free flaps after ablative surgery or trauma is commonly performed in patients with comorbidities, including vascular comorbidities such as arterial hypertension (AHTN), type 2 diabetes mellitus (DM), and atherosclerotic vascular disease (ASVD) [1,2,3,4].
These vascular comorbidities or their related vascular changes are associated with impairment of systemic macrovascular and microvascular perfusion and therefore may also have an impact on the perfusion of microvascular free flaps [5,6,7,8,9]. AHTN and DM are associated with vascular changes such as endothelial dysfunction (with vasoconstriction), vascular fibrosis (with increased vessel stiffness), and capillary scarcity, leading to impaired macrovascular and microvascular perfusion [6,7,8]. In addition, ASVD is associated with vascular changes such as vascular plaque formation, vessel wall thickening, and progressive vessel lumen obstruction, leading to impaired macrovascular perfusion [5, 9].
Microvascular free flap perfusion (microvascular blood flow and tissue oxygenation) is a prerequisite for flap survival, and decreased flap perfusion has been shown to lead to microvascular free flap necrosis and failure [10,11,12,13,14]. Despite the potential impairment of microvascular free flap perfusion by AHTN, DM, and ASVD, several studies have found no associations between these comorbidities and flap failure in terms of a difference in flap failure rates between patients with and without AHTN, DM, or ASVD [2,3,4, 15, 16].
However, to date, no studies have explicitly examined the impacts of these comorbidities or their related vascular changes on microvascular free flap perfusion. Whether AHTN, DM, and ASVD or their related vascular changes affect microvascular free flap perfusion remains unknown in the perspective of getting insights into the physiology of microvascular free flap perfusion and finding an explanation for similar flap failure rates between patients with and without vascular comorbidities.
This study aimed to evaluate the impacts of vascular comorbidities such as AHTN, DM, and ASVD on microvascular free flap perfusion.
Materials and methods
Study population
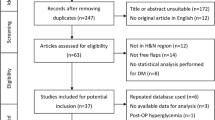
The local ethics committee of the Medical Faculty of RWTH Aachen University approved this retrospective study (EK 309-20). Datasets from a total of 308 patients treated for malignant or nonmalignant disease were used. All patients had undergone microvascular head and neck reconstruction in our Department of Oral and Maxillofacial Surgery between 2011 and 2020. The microvascular free flaps used were radial free forearm flaps (RFFF), anterolateral thigh flaps (ALTF), or fibula free flaps (FFF). Exclusion criteria for the study were flap failure with flap removal, intraoperative or postoperative flap revision, age less than 18 years, diabetes mellitus other than type 2, and missing or incomplete data records.
Clinical records, operation reports, and perfusion measurement protocols were used to obtain data for further analysis. AHTN and DM were diagnosed in accordance with discipline-specific guidelines. ASVD was diagnosed if coronary heart disease, cerebrovascular disease, and or peripheral arterial disease were diagnosed in accordance with discipline-specific guidelines [8, 9]. Smoking status was designated as positive if the patients had actually or in the past smoked on a daily basis for a period of at least 6 months [17]. Prior neck dissection or irradiation status was designated as positive if patients had undergone neck dissection, including an anatomic dissection of the recipient vessel, or neck irradiation, including the area of the recipient vessel, prior to actual surgery. Duration of surgery and flap ischemia was calculated as the time interval between the first incision and the last suture and between flap perfusion cessation on the donor site and flap perfusion onset after anastomosis release on the recipient side, respectively.
All microvascular free flap reconstructions were performed under general anesthesia, and the flaps pedicles were connected to the cervical vasculature as follows: end-to-end configuration for the arterial vessels and end-to-end or end-to-side configuration for the venous vessels. Postoperatively, all patients stayed in the intensive care unit with invasive mechanical ventilation and analgosedation at least until the morning of the first postoperative day. In addition, blood pressure was monitored with an invasive arterial catheter and regulated by continuous central venous vasopressor administration (norepinephrine) with a syringe pump as needed (with a target systolic pressure above 125 mmHg). Heparin (5000 IU) was injected intracutaneously three times daily for 7 days.
Measurement of perfusion parameters
Measurement of flap perfusion was performed using the O2C tissue oxygen analysis system (O2C Oxygen-to-see, LEA Medizintechnik, Giesen, Germany) described previously [11, 13, 18]. Blood flow (arbitrary units [AU]) was calculated using laser Doppler spectroscopy (830 nm; 30 mW), and hemoglobin concentration (AU) and hemoglobin oxygen saturation (%) were calculated using white light spectroscopy (500–800 nm; 50 W) [10, 11]. Measurements were performed intraoperatively (immediately after anastomosis release) and postoperatively (on the first postoperative morning), with the probe sealed in a sterile cover and placed centrally on the dried skin portion of the flap and a measurement time of 10 s (with a lead time of 4 s) under ambient light compensation control. Flap perfusion parameters, i.e., flap blood flow, hemoglobin concentration, and hemoglobin oxygen saturation, were determined as mean values from 2-mm and 8-mm tissue depth.
Statistical analysis
For statistical analysis, patients were divided into those with and without AHTN, DM, or ASVD. In addition, patients with AHTN, DM, and or ASVD were pooled as one group to be compared with patients without these comorbidities. They were also divided into those with and without an American Society of Anesthesiologists score (ASA) above 2. Differences between groups were analyzed as follows: for clinical parameters, the chi-squared test, Fisher’s exact test, or Freeman-Halton test for categorical data and the Mann–Whitney test for metric data were used; for flap perfusion parameters, i.e., blood flow, hemoglobin concentration, and hemoglobin oxygen saturation, the Mann–Whitney test for univariable analysis and multiple linear regression models for multivariable analysis were used. For multivariable comparison of patients with and without ASVD, adjustment was made for sex, age, ASA (≤ 2 vs. > 2), prior neck irradiation, flap type (RFFF vs. ALTF vs. FFF), flap location (intraoral vs. extraoral), mean arterial blood pressure (mmHg), and administered catecholamine dose (µg/min/kg). For multivariable comparison of patients with and without DM, adjustment was made for age, body mass index (BMI) (≤ 25 kg/m2 vs. > 25 kg/m2), flap type (RFFF vs. ALTF vs. FFF), flap location (intraoral vs. extraoral), mean arterial blood pressure (mmHg), and administered catecholamine dose (µg/min per kg body weight). Statistical significance was considered at p values < 0.05. For statistical analysis SPSS version 28 (SPSS, IBM, New York, USA) was used.
Results
Comparison of clinical parameters between groups
The study population included a total of 308 patients (112 patients with AHTN and 196 patients without AHTN, 40 patients with DM and 268 patients without DM, 42 patients with ASVD and 266 patients without ASVD, and 157 patients with AHTN, DM and or ASVD and 151 patients without AHTN, DM and or ASVD) (Table 1). Patients with and without AHTN or DM differed with respect to age (p < 0.001 and p = 0.005, respectively) and BMI (p < 0.001 and p < 0.001, respectively). Patients with and without ASVD differed in sex (p = 0.001), age (p = 0.030), ASA (p = 0.007), and prior neck irradiation (p = 0.037). Patients with and without AHTN, DM and or ASVD differed with respect to age (p < 0.001) and BMI (p < 0.001).
Comparison of flap perfusion parameters between groups
Intraoperative blood flow was similar between patients with and without AHTN, DM, or ASVD (p = 0.988, p = 0.926, and p = 0.058, respectively) (Table 2, Fig. 1). No differences were observed in intraoperative hemoglobin concentration between patients with and without AHTN, DM, or ASVD (p = 0.099, p = 0.694, and p = 0.258, respectively) (Table 2). Intraoperative hemoglobin oxygen saturation was similar in patients with and without AHTN or DM (p = 0.962 and p = 0.286, respectively) and lower in patients with ASVD than in patients without ASVD (63.3% vs. 69.5%, p = 0.046) (Table 2, Fig. 2). Upon adjustment for sex, age, ASA, prior neck irradiation, flap type, flap location, mean arterial blood pressure, and administered catecholamine dose, this difference did not persist (p = 0.094).
Intraoperative blood flow measurement. Box plot for blood flow (AU) for intraoperative measurement (separately described for patients without and with AHTN, for patients without and with DM, and for patients without and with ASVD); p values corresponding to testing for differences with Mann–Whitney test; AHTN arterial hypertension, DM diabetes mellitus, ASVD atherosclerotic vascular disease, AU arbitrary units.
Intraoperative hemoglobin oxygen saturation measurement. Box plot for hemoglobin oxygen saturation (%) for intraoperative measurement (separately described for patients without and with AHTN, for patients without and with DM, and for patients without and with ASVD); p values corresponding to testing for differences with Mann–Whitney test; significant p values are bold (*p = 0.094 upon adjustment for sex, age, ASA (1 + 2 vs. 3 + 4), prior neck irradiation, flap type (RFFF vs. ALTF vs. FFF), flap location (intraoral vs. extraoral), mean arterial blood pressure (mmHg), and administered catecholamine dose (µg/min/kg) in multiple linear regression analysis); AHTN arterial hypertension, DM diabetes mellitus, ASVD atherosclerotic vascular disease.
Postoperative blood flow was similar in patients with and without AHTN or DM (p = 0.924 and p = 0.396, respectively) and lower in patients with ASVD than in patients without ASVD (67.5 AU vs. 85.0 AU, p = 0.036) (Table 2, Fig. 3). Upon adjustment for sex, age, ASA, prior neck irradiation, flap type, flap location, mean arterial blood pressure, and administered catecholamine dose, this difference did not persist (p = 0.311). Postoperative hemoglobin concentration was similar in patients with and without AHTN or ASVD (p = 0.224 and p = 0.190, respectively) and lower in patients with DM than in patients without DM (43.5 AU vs. 47.5 AU, p = 0.028) (Table 2). This difference did not persist upon adjustment for age, BMI, flap type, flap location, mean arterial blood pressure, and administered catecholamine dose (p = 0.060). No differences were observed for postoperative hemoglobin oxygen saturation between patients with and without AHTN, DM, or ASVD (p = 0.635, p = 0.969, and p = 0.339, respectively) (Table 2, Fig. 4).
Postoperative blood flow measurement. Box plot for blood flow (AU) for postoperative measurement (separately described for patients without and with AHTN, for patients without and with DM, and for patients without and with ASVD); p values corresponding to testing for differences with Mann–Whitney test; significant p values are bold (*p = 0.311 upon adjustment for sex, age, ASA (1 + 2 vs. 3 + 4), prior neck irradiation, flap type (RFFF vs. ALTF vs. FFF), flap location (intraoral vs. extraoral), mean arterial blood pressure (mmHg), and administered catecholamine dose (µg/min per kg) in multiple linear regression analysis); AHTN arterial hypertension, DM diabetes mellitus, ASVD atherosclerotic vascular disease, AU arbitrary units.
Postoperative hemoglobin oxygen saturation measurement. Box plot for hemoglobin oxygen saturation (%) for postoperative measurement (separately described for patients without and with AHTN, for patients without and with DM, and for patients without and with ASVD); p values corresponding to testing for differences with Mann–Whitney test; AHTN arterial hypertension, DM diabetes mellitus, ASVD atherosclerotic vascular disease.
No differences were observed in all perfusion measurements between patients with and without AHTN, DM, and or ASVD (all p > 0.05) (Table 2).
Discussion
This study investigated the impact of vascular comorbidities, i.e., AHTN, DM, and ASVD, on microvascular free flap perfusion, as these comorbidities are associated with impaired systemic macrovascular and microvascular perfusion and are common in patients undergoing head and neck reconstruction with microvascular free flaps [1,2,3,4,5,6,7,8,9]. Impaired systemic macrovascular and microvascular perfusion caused by vasoconstriction, vascular stiffness, and capillary scarcity in patients with AHTN and DM, and impaired systemic macrovascular perfusion caused by vascular plaque formation, wall thickening, and lumen obstruction in patients with ASVD, might also compromise free flap perfusion as a prerequisite for flap viability and survival, and thus for reconstruction success [5,6,7,8,9,10,11,12, 14, 19, 20]. However, microvascular free flaps have been successfully used in patients with AHTN, DM, or ASVD despite presumably compromised physical conditions [2,3,4,5,6,7,8,9, 15, 16].
Hence, this study aimed to investigate the impact of these vascular comorbidities on microvascular free flap perfusion with a view to providing a possible explanation for the successful use of microvascular free flaps despite presumably compromised physical conditions. This study did not examine the impacts of these comorbidities on flap success nor evaluate flap perfusion cut-off values to determine flap failure, as several previous studies have already addressed both aspects [2,3,4, 11, 13, 15, 16].
In this study, patients were confirmed to have AHTN or DM when their diagnoses were confirmed according to the disease-specific guidelines. Patients with diabetes mellitus other than type 2 were only a minority and were excluded to reduce heterogenicity. Patients with confirmed diagnoses of cerebrovascular disease, coronary heart disease, and/or peripheral arterial disease were grouped together as patients with ASVD since these diseases are predominantly of atherosclerotic origin [21, 22]. In the multivariable analysis, adjustment was made for factors with observed differences between groups (e.g., sex, age, BMI, ASA and prior neck irradiation) and for factors with presumed impact on flap perfusion (e.g., flap type, mean arterial blood pressure, and catecholamine dose administered) [13, 18, 23].
The results of this study demonstrated that flap perfusion parameters, i.e., flap blood flow, hemoglobin concentration and hemoglobin oxygen saturation, were similar between patients with and without AHTN, DM, and ASVD, both intraoperatively (immediately after anastomosis release) and postoperatively (on the first postoperative morning). This suggests that these comorbidities have no impacts on the perfusion of microvascular free flaps used for reconstruction of the head and neck region. With regard for a comparable study that also measured microvascular free flap perfusion with the O2C device, the measured values for postoperative flap perfusion in this study were corresponding [24]. However, in univariable testing, some differences were found between groups. The lower intraoperative hemoglobin oxygen saturation in patients with ASVD compared to patients without ASVD in the univariable analysis may be attributed to the tendentially lower blood flow of patients with ASVD, since hemoglobin oxygen saturation depends on blood flow [11]. The lower postoperative hemoglobin concentration in patients with DM compared to patients without DM may reflect the capillary scarcity associated with DM, as hemoglobin is primarily located in the capillary-venous compartment of the microcirculation [11]. The tendentially lower intraoperative and significantly lower postoperative blood flow in patients with ASVD compared to patients without ASVD may be related to a lower adaptability of their flaps to the perfusion conditions at the cervical recipient sites in terms of vasodilatation (caused, for example, by ASVD-related vascular stiffness), as microvascular free flaps usually show an increase in blood flow after anastomosis to the cervical recipient vessel [5, 13]. Interestingly, in the present study, the commonly observed increase in flap blood flow between the intraoperative and postoperative perfusion measurements was relatively lowest in patients with ASVD (6.6% vs. 8.3–16.4%). However, neither difference persisted in the multivariable analysis, suggesting that differences were likely due to factors other than the presence of AHTN, DM, or ASVD. The comparable flap perfusion in patients with and without AHTN, DM, and ASVD may be explained by the absence—or, at least, insignificance—of presumably compromised physical conditions in the recipient and donor site vasculature and flap tissues [25].
With regard to the limitations of the current study, several aspects should be mentioned. Although the O2C device has been shown to be a reliable method for measuring flap perfusion, a moist environment due to salivatory flow and wound secretion as well as differences in skin temperature may influence the measurement [10, 18, 24, 26, 27]. However, all skin surfaces were dried prior to measurement, an adjustment for flap location (intraoral vs. extraoral) was made in the multivariable testing in view of potentially higher measurement difficulties with intraoral flaps due to the moist environment, and all measurements were performed in rooms (operating theater and intensive care unit) with room climate control, all which might mitigate these potential influences. Nevertheless, potential differences in several factors that might affect flap perfusion (e.g., the length and diameter of the pedicle vessel) among patients cannot be excluded. In addition, it cannot be precluded that groups were heterogenous with respect to the extent of vascular changes caused by AHTN and DM (e.g., owing to differences in disease duration). Moreover, the group of patients with ASVD included individuals with different diseases. Unfortunately, preoperative and postoperative reference values for flap perfusion before flap harvest and for the opposite donor site, respectively, were not available, and only smokers (current and former) and non-smokers could be distinguished due to the lack of information regarding the timepoints of smoking cessation. Notably, the success of microvascular free flaps depends on multiple factors (e.g., the technical requirements for anastomosis) and flap perfusion is only one contributing factor [14, 28]. Moreover, flap perfusion is a critical factor that affects flap viability and flap survival well beyond the short time frame examined in this study, and it cannot be ruled out that flap perfusion may change over time beyond the period investigated [14, 28].
This study demonstrated that vascular comorbidities such as AHTN, DM, and ASVD have no impact on initial microvascular free flap perfusion. Interestingly, in our data set, before exclusion of patients with flap failure, no difference was observed between patients with and without AHTN, DM or ASVD in terms of flap failure (1 (0.9%) vs. 4 (2.0%), Fisher’s exact test p = 0.657; 0 (0.0%) vs. 5 (1.8%), Fisher’s exact test p = 1.000; 2 (4.5%) vs. 3 (1.1%), Fisher’s exact test p = 0.146). Although the success of microvascular free flaps depends on multiple factors, unrestricted flap perfusion in patients with AHTN, DM, or ASVD may reflect both initial functionality of the technical procedure as well as an equivalent basis for the further course and thus contribute to the success of microvascular free flaps used for head and neck reconstruction in these patients [1,2,3,4, 11, 12, 14, 28].
Conclusion
In microvascular free flaps used for head and neck reconstruction, flap perfusion parameters (e.g., flap blood flow and hemoglobin oxygen saturation) did not differ between patients with and without AHTN, DM, and ASVD. These results indicate that these comorbidities have no initial impact on flap perfusion. This may contribute to the successful use of microvascular free flaps for reconstruction in the head and neck region in patients with AHTN, DM, and ASVD.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Valentini V, Cassoni A, Marianetti TM et al (2008) Diabetes as main risk factor in head and neck reconstructive surgery with free flaps. J Craniofac Surg 19:1080–1084. https://doi.org/10.1097/SCS.0b013e3181763531
Vandersteen C, Dassonville O, Chamorey E et al (2013) Impact of patient comorbidities on head and neck microvascular reconstruction. A report on 423 cases. Eur Arch Otorhinolaryngol 270:1741–1746. https://doi.org/10.1007/s00405-012-2224-z
Brady JS, Govindan A, Crippen MM et al (2018) Impact of diabetes on free flap surgery of the head and neck: a NSQIP analysis. Microsurgery 38:504–511. https://doi.org/10.1002/micr.30276
Crawley MB, Sweeny L, Ravipati P et al (2019) Factors associated with free flap failures in head and neck reconstruction. Otolaryngol Head Neck Surg 161:598–604. https://doi.org/10.1177/0194599819860809
Chen H-C, Coskunfirat OK, Ozkan O et al (2006) Guidelines for the optimization of microsurgery in atherosclerotic patients. Microsurgery 26:356–362. https://doi.org/10.1002/micr.20252
Harvey A, Montezano AC, Touyz RM (2015) Vascular biology of ageing-Implications in hypertension. J Mol Cell Cardiol 83:112–121. https://doi.org/10.1016/j.yjmcc.2015.04.011
Guzik TJ, Touyz RM (2017) Oxidative stress, inflammation, and vascular aging in hypertension. Hypertension 70:660–667. https://doi.org/10.1161/HYPERTENSIONAHA.117.07802
Petrie JR, Guzik TJ, Touyz RM (2018) Diabetes, hypertension, and cardiovascular disease: clinical insights and vascular mechanisms. Can J Cardiol 34:575–584. https://doi.org/10.1016/j.cjca.2017.12.005
Ziegler T, Abdel Rahman F, Jurisch V et al (2019) Atherosclerosis and the capillary network; pathophysiology and potential therapeutic strategies. Cells 9(1):50. https://doi.org/10.3390/cells9010050
Beckert S, Witte MB, Königsrainer A et al (2004) The impact of the micro-lightguide O2C for the quantification of tissue ischemia in diabetic foot ulcers. Diabetes Care 27:2863–2867. https://doi.org/10.2337/diacare.27.12.2863
Hölzle F, Loeffelbein DJ, Nolte D et al (2006) Free flap monitoring using simultaneous non-invasive laser Doppler flowmetry and tissue spectrophotometry. J Craniomaxillofac Surg 34:25–33. https://doi.org/10.1016/j.jcms.2005.07.010
Abdel-Galil K, Mitchell D (2009) Postoperative monitoring of microsurgical free tissue transfers for head and neck reconstruction: a systematic review of current techniques—part I. Non-invasive techniques. Br J Oral Maxillofac Surg 47:351–355. https://doi.org/10.1016/j.bjoms.2008.11.013
Hölzle F, Rau A, Loeffelbein DJ et al (2010) Results of monitoring fasciocutaneous, myocutaneous, osteocutaneous and perforator flaps: 4-year experience with 166 cases. Int J Oral Maxillofac Surg 39:21–28. https://doi.org/10.1016/j.ijom.2009.10.012
Mücke T, Wolff K-D, Rau A et al (2012) Autonomization of free flaps in the oral cavity: a prospective clinical study. Microsurgery 32:201–206. https://doi.org/10.1002/micr.20984
Lee MK, Blackwell KE, Kim B et al (2013) Feasibility of microvascular head and neck reconstruction in the setting of calcified arteriosclerosis of the vascular pedicle. JAMA Facial Plast Surg 15:135–140. https://doi.org/10.1001/2013.jamafacial.208
Kantar RS, Rifkin WJ, David JA et al (2019) Diabetes is not associated with increased rates of free flap failure: analysis of outcomes in 6030 patients from the ACS-NSQIP database. Microsurgery 39:14–23. https://doi.org/10.1002/micr.30332
Latza U, Hoffmann W, Terschüren C et al (2005) Rauchen als möglicher confounder in epidemiologischen studien: standardisierung der erhebung, quantifizierung und analyse. Gesundheitswesen 67:795–802. https://doi.org/10.1055/s-2005-858807
Mücke T, Rau A, Merezas A et al (2014) Changes of perfusion of microvascular free flaps in the head and neck: a prospective clinical study. Br J Oral Maxillofac Surg 52:810–815. https://doi.org/10.1016/j.bjoms.2014.07.001
Boss GR, Seegmiller JE (1981) Age-related physiological changes and their clinical significance. West J Med 135:434–440
Rahmanian-Schwarz A, Rothenberger J, Amr A et al (2012) A postoperative analysis of perfusion dynamics in deep inferior epigastric perforator flap breast reconstruction: a noninvasive quantitative measurement of flap oxygen saturation and blood flow. Ann Plast Surg 69:535–539. https://doi.org/10.1097/SAP.0b013e31821bd484
Kobiyama K, Ley K (2018) Atherosclerosis. Circ Res 123:1118–1120. https://doi.org/10.1161/CIRCRESAHA.118.313816
Flora GD, Nayak MK (2019) A brief review of cardiovascular diseases, associated risk factors and current treatment regimes. Curr Pharm Des 25:4063–4084. https://doi.org/10.2174/1381612825666190925163827
de Backer D, Foulon P (2019) Minimizing catecholamines and optimizing perfusion. Crit Care 23:149. https://doi.org/10.1186/s13054-019-2433-6
Hohlweg-Majert B, Ristow O, Gust K et al (2012) Impact of radiotherapy on microsurgical reconstruction of the head and neck. J Cancer Res Clin Oncol 138:1799–1811. https://doi.org/10.1007/s00432-012-1263-6
de Bree R, Quak JJ, Kummer JA et al (2004) Severe atherosclerosis of the radial artery in a free radial forearm flap precluding its use. Oral Oncol 40:99–102. https://doi.org/10.1016/s1368-8375(03)00133-7
Hölzle F, Mitchell DA, Rau A et al (2012) Assessment of the perfusion and morbidity of the buccal mucosal donor site for grafting of urethral strictures. J Craniomaxillofac Surg 40:47–50. https://doi.org/10.1016/j.jcms.2010.12.004
Dornseifer U, Fichter AM, von Isenburg S et al (2016) Impact of active thermoregulation on the microcirculation of free flaps. Microsurgery 36:216–224. https://doi.org/10.1002/micr.22523
Üstün GG, Aksu AE, Uzun H et al (2017) The systematic review and meta-analysis of free flap safety in the elderly patients. Microsurgery 37:442–450. https://doi.org/10.1002/micr.30156
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was approved by the local ethics committee of the Medical Faculty of RWTH Aachen University (EK 309-20) and was conducted retrospectively from data obtained for clinical purposes. The local ethics committee of the Medical Faculty of RWTH Aachen University allowed us to waive informed consent for this human study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ooms, M., Heitzer, M., Winnand, P. et al. Impacts of vascular comorbidities on free flap perfusion in microvascular head and neck reconstruction. Eur Arch Otorhinolaryngol 280, 3375–3382 (2023). https://doi.org/10.1007/s00405-023-07913-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-07913-1