Abstract
Purpose
To study the efficacy of virtual reality (VR) interventional programs as a vestibular rehabilitative method for patients with uncompensated peripheral vestibular disorders.
Methods
The databases PubMed, Google scholar, Embase and Cochrane Library were used (up to July 2021). Studies selected in this study were controlled trials in which virtual reality was used as vestibular rehabilitative therapy in comparison to any other vestibular rehabilitative methods or medical or dietary recommendations. Comparison was made in at least one of these outcomes measures; Subjective measures such as Dizziness Handicap Inventory, Vertigo Symptom Scale—Short Form questionnaire, Activities-specific Balance Confidence questionnaire, Dizziness Analogue Scale or Visual Analogue Scale, besides objective measures as posturography. Six articles were included in the meta-analysis; tested for heterogeneity of the estimates using chi-squared and I2 tests, outcomes were expressed as mean difference and 95% CI. Estimates from included studies were pooled using the random-effect model.
Results
virtual reality as a vestibular rehabilitative intervention was able to improve scores of Dizziness Handicap Inventory, Vertigo Symptom Scale—Short Form questionnaire, Visual Analogue sale and posturography as outcome measures of vestibular rehabilitation.
Conclusion
virtual reality has a potential clinical benefit for vestibular rehabilitation in peripheral vestibular dysfunction compared with conventional vestibular rehabilitation methods. However, further research is needed to document the exact parameters of an optimal protocol for virtual reality rehabilitation, the period needed for effective rehabilitation and its side effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vestibular rehabilitation (VR) therapy is considered a safe and effective treatment for uncompensated peripheral vestibular dysfunction [1]. It can also improve static and dynamic balance and gait, as well as reduce comorbid symptoms of dizziness such as depression and anxiety, resulting in an increase in patients' self-confidence and quality of life [2]. Vestibular rehabilitation integrates proprioceptive, visual, and residual vestibular function to improve balance, including gaze, gait and postural stability, and physical mobility [3]. However, many factors may negatively affect the outcome of vestibular rehabilitation, including incorrect exercises performance and the necessity of active efforts and motivation of the patient [4].
VR-based vestibular rehabilitative therapy is one of the most innovative and promising recent developments in rehabilitation technology in which the users interact with displayed images, move and manipulate virtual objects and perform other actions in a way that attempts to "immerse” them within the simulated environment engendering a feeling of presence in the virtual world [5]. VR systems can be equipped with real-time simulation, interactive functions, and game features enabling adaptation, habituation, and substitution exercises to fulfill vestibular rehabilitation objectives [6].
With complete control over the stimuli presented to the subject, VR offers a standardized and reproducible setting for vestibular rehabilitation that has several benefits [7]. Additionally, the facts that VR is a pleasurable training tool motivate patients to continue their rehabilitation [8]. Compared to traditional rehabilitative therapy approaches, it provides more feedback, stimulating and enriching development [9]. Additionally, it improves gait capability, lower extremity function, and consequently balance [10].
Meanwhile, there are some limitations of virtual reality such as the latency of the system; all the steps from the capture of information (motion, center of pressure, etc.) to the multisensory feedback (i.e., visual) take time, this delay can be perceived by the patient, consequently he may modify his reactions, so there is a different perception of distances and underestimation in VR compared to the real situation [8]. In addition, Cyber-sickness experienced, especially with the more immersive virtual environments [11]. Nausea, vomiting, headache, somnolence, loss of balance, and altered eye–hand coordination are all common symptoms of cyber-sickness [12]. Sometimes the inconsistency between the information received by the body and the eyes in virtual reality leads to dizziness, headache and sickness [13].
However, many studies were done exploring the efficacy of VR as a rehabilitative tool, but no standardized guidelines have been settled in the literature and there is also a high diversity of settings and protocols involving virtual reality for vestibular rehabilitation. Accordingly, this study aimed to search, critically appraise, and synthesize the best available evidence on whether virtual reality interventions are effective in the rehabilitation of peripheral vestibular dysfunction or not. This research systematically reviewed the previous studies to summarize the published protocols documenting the use of virtual reality settings for peripheral vestibular disorders rehabilitation.
Methods
This systematic review was performed following the (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) PRISMA 2020 guidelines [14].
The criteria for considering studies
Studies included in this study are the controlled trials in which VR was used as vestibular rehabilitative therapy in comparison to any other vestibular rehabilitative (conventional) modalities, medical treatment or dietary recommendations.
Research question: Is virtual reality-based vestibular rehabilitation therapy effective in the rehabilitation of uncompensated peripheral vestibular dysfunction? This research question was established following recommendations from the PICO format (Participants, Intervention, Comparison and Outcome measures) [15].
-
Type of participants: Included male and female patients, over 18 years of age, clinically diagnosed with unilateral or bilateral peripheral vestibular dysfunction with no specifically diagnosed neurological disorder.
-
Type of interventions: Balance, gaze and gait training using any virtual reality system, with no restrictions on the technique used in rehabilitation or duration of the rehabilitation.
-
Comparison: virtual reality methods were compared to any other vestibular rehabilitative methods as well as medical treatment or dietary recommendations.
-
Types of outcome measures: In the studies, at least one of the following outcome measures required to be used to compare the experimental and control groups:
-
Subjective measures such as Dizziness Handicap Inventory (DHI), Vertigo Symptom Scale—Short Form questionnaire (VSS-SF), Activities-specific Balance Confidence questionnaire (ABC), Dizziness Analogue Scale or Visual Analogue Scale (VAS) (SAT) Score of patient satisfaction.
-
Objective measures such as posturography.
Exclusion criteria included studies without a comparison group (as case studies, observational studies etc.), studies with participants younger than 18 years, patients with central or mixed causes vestibular dysfunctions, studies with target outcome other than those mentioned previously in inclusion criteria, studies comparing two types of virtual reality, as well as studies involving healthy subjects and studies not in the English language.
Research method
Review process included procedures, considerations, and decisions that lead to a consolidated list of articles to be reviewed in-depth. This article review process consisted of the following steps;
Definition of the review scope, keywords, and research question
Although the research questions have been identified, defining the scope and keywords was quite challenging because, in fact, VR research is extensive and the number of publications in this area is abundant.
The search was done by extracting key information from documents indexed in four scientific digital libraries; PubMed, Google Scholar, Cochrane and Embase.
Initial paper search.
The search was conducted using MeSH (Medical Subject Headings) by changing between the following keywords: (virtual reality—video games—vestibular rehabilitation—peripheral vestibular dysfunction) as shown in Table 1, and the terms were used as keywords in the title and abstract in all databases, with one or more concept of these keywords, the simple or advanced search when possible was conducted using the Boolean operators ‘‘AND’’ and ‘‘OR”. These databases were searched until July 2021.
Removing duplicate documents
Once the papers were identified; the duplicated studies were removed using the EndNote program [computer program], Version X9, Clarivate Analytics, 2018.
Manual filtering by reading the titles and abstracts
Articles were selected by two independent reviewers who analyzed the title and the abstract. If there were disagreements, the remaining two authors would also judge the abstracts.
Manual filtering by reading the contents and excluding irrelevant entries
At this stage, the full text was analyzed, the results were compared, and discrepancies between articles were discussed.
Data collection methods
This was created manually by the authors by summarizing the information for qualitative and quantitative synthesis from the included studies by using Excel files. The study characteristics (the author's name, year of publication, journal, site in which the study was done, comparison groups, type of intervention, measurements of efficacy, and outcome measures) were determined. Any disagreements on data extraction or quality assessment were resolved by consensus between the authors.
Data management and analysis methods
Data was revised for completeness and consistency. The program used for building the meta-analysis model was Review Manager (RevMan) [Computer program], Version 5.4, The Cochrane Collaboration, 2020. The used models were tested by random effect. The graphical presentation was extracted from Review Manager 5.4.
Studies included in the meta-analysis were tested for heterogeneity of the estimates using the following tests: the chi-squared (χ2, or Chi2), the I2 test and the p value. A forest plot was used to display effect estimates and confidence intervals for both individual studies and meta-analyses .
Results
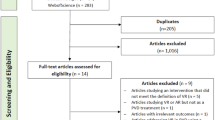
The search in the databases; PubMed, Google Scholar, Embase, and Cochrane Library, (up to July 2021) yielded 501 articles.
After removing duplicates, 480 articles remained. Of these, 252 were excluded based on the title and abstract due to various causes as shown in Fig. 1; studies focused on other diseases such as stroke, multiple sclerosis, and Parkinson’s disease. Other studies focused on traumatic causes of imbalance. Studies that included children, studies not in the English language and review articles were also excluded. After reading the full text of 228 articles; 222 were excluded, due to the presence of normal subjects in the studies, the presence of central or mixed vestibular cases, Alzheimer, acute vestibular neuritis or undetected causes of fall or imbalance. Also uncontrolled studies, studies compared two types of virtual reality, studies without proposed outcomes and studies in which virtual reality was used as a diagnostic tool were also excluded. The full text of some studies was not available so they were excluded.
Finally, six articles were included in our study as shown in the flowchart in Fig. 1.
Summary of studies
Two hundred fifty-eight patients participated in the included six studies. Patients were diagnosed with peripheral vestibular lesions whether unilateral or bilateral.
A summary of these studies can be found in the following Tables 2, 3, 4.
Pooling of estimates
Outcomes were expressed as mean difference (MD) and 95% confidence interval (CI) Due to the presence of some heterogeneity between the studies in some scales as determined by the chi-squared test and I2 test, the data was analyzed using the random effect model as it is the more conservative approach even if there is no heterogeneity. In cases of high unaccepted heterogeneity between the included studies, the results of the meta-analysis were insignificant so qualitative analysis had to be done.
Posturography (COP) on firm surface with closed eye
See Fig. 2.
Vertigo Symptom Scale Short Form (VSS-SF)
See Fig. 3.
Visual analogue scale (VAS) (SAT) score of patient satisfaction
See Fig. 4.
Dizziness Handicap Inventory (DHI) total score
See Fig. 5.
Activities-specific balance confidence (ABC) scale
See Fig. 6.
Dizziness analogue scale (DAS)
Discussion
The aim of this study is to study the efficacy of virtual reality-based vestibular rehabilitation in patients with peripheral vestibular disorders. There are previously published systematic reviews that evaluated this issue; Bergeron et al. [27], demonstrated the promising potential of VR in vestibular rehabilitation, despite the significant differences in terms of protocols used and outcome evaluation among their selected studies. They mentioned that none of the selected seven studies had low methodological quality; as four studies only had a control group. In addition, few studies used validated questionnaires, so direct and standardized comparison between studies was not applicable. Meanwhile, they concluded that time spent in VR-based training contributed more in its efficiency than the number of sessions. So, longer sessions in a shorter period of time could be effective and convenient.
In 2019, Kinne et al. [28] conducted a systematic review to evaluate the efficacy of home-based virtual reality systems on vestibular rehabilitation outcomes, concluding that these interventions effectively achieved the primary objectives of vestibular rehabilitation; but the use of these interventions was equally as effective as the use of traditional vestibular rehabilitation program. In addition, they reported that it may be most beneficial to combine home-based virtual reality with traditional vestibular rehabilitation methods.
Heffernan et al. [29] included five randomized controlled trials in their review. Meta-analysis was done on 4 of them using the DHI total score only, concluding that virtual reality vestibular rehabilitation improves DHI scores significantly more than conventional vestibular rehabilitation alone 0–3 months’ post-intervention.
Regarding the current meta-analysis, the authors tried to improve some of the methodological aspects of the previous systematic reviews. The six studies included in this study were controlled studies, all of them were randomized except Rosiak et al. [20] which was a non-randomized controlled trial. This helps to increase the level of evidence of the included studies. Also objective as well as subjective outcome measures were used. The use of the objective measure revealed more strength to the current study; as although subjective outcomes are more important in establishing clinical benefit, evidence of similar improvements in objective outcomes can enhance the internal validity of the studies.
This study attempts to synthesize the results of the included studies into one pooled estimate providing a meta-analysis. They included two hundred fifty-eight (258) patients diagnosed with peripheral vestibular lesions (unilateral in 5 studies and bilateral in 1 study).
The meta-analysis performed in this study on posturography (COP on a firm surface with a closed eye) (Fig. 2) was reported by 3 of the included studies. The test of heterogeneity is 0%, which shows no heterogeneity and the P value of the overall effect estimate is highly significant (P ˂ 0.00001). So, virtual reality is better than the other methods in improving postural control and increasing stability limits. This was explained as VR improves the vestibular source of spatial information and subsequent central reweighting and related postural control [18].
Regarding the subjective outcomes; VSS-SF, VAS- SAT and DHI total score, their meta-analyses revealed that virtual reality is superior with high significance (P ˂ 0.00001) to the traditional vestibular rehabilitation activities as shown in Figs. 3, 4 and 5. VSS-SF reduced scores were as a result of decreased overall sensation of dizziness (physical and emotional states), intensity decreased more with the virtual reality group. Furthermore, the Visual Analog Scale (VAS)—SAT revealed that patients in virtual reality groups were more satisfied with the VR-rehabilitative method. Virtual reality is characterized as being an enjoyable and easily accessible form of therapy. The test of heterogeneity is 0% (showing no heterogeneity), and the P value of the overall effect estimate is highly significant (P ˂ 0.0001). Additionally, Stankiewicz et al. [21] added that the beneficial therapeutic effects are experienced earlier with VR therapy than the conventional methods.
On the other hand, the Activities-specific balance confidence (ABC) scale that was reported by two of the included studies, Meldrum et al. and Micarelli et al.. In Meldrum et al. [17], there was no significant difference between the virtual reality group and the traditional vestibular rehabilitative group for the ABC scale. Although their patients reported VR was more enjoyable, less fatigable and less difficult in balance exercises, taking in consideration that Meldrum et al. used a home-based VR program. While in Micarelli et al. [18], there was a significant post-treatment effect change in the ABC scale which is in agreement with the systematic review Xie et al. [30].
While there was a significant post-treatment change in the ABC scale in Micarelli et al. [18], this is consistent with the systematic review by Xie et al. [30]. Accordingly, there was substantial high heterogeneity (73%) between the results of the ABC scale between these two included studies and the results of pooling of their estimates were not significant (P = 0.69) (Fig. 6).
The meta-analysis performed on the Dizziness Analogue Scale (DAS) that was used by two of the included studies, Garcia et al. and Stankiewicz et al., revealed that the virtual reality group showed more significant score reductions in the Dizziness analogue scale and, therefore, improvements from dizzy spells when compared against controls. But there was moderate heterogeneity (58%), and the results of the pooling of estimates were not significant (P = 0.10) (Fig. 7).
Side effects of virtual reality interventions were studied by Micarelli et al. using the validated simulator sickness questionnaire (SSQ). They examined how the patients were habituated to the intervention at the end of each week of rehabilitation. Symptoms decreased over time; there was a significant decrease in nausea, oculomotor stress, and disorientation scores from the first to the fourth week of the VR rehabilitation program. They suggested that patients were safely habituating to the virtual reality stimuli. Also, Pavlou et al. [31] revealed nearly the same results. While Meldrum et al. [17] found low back pain, neck pain, and severe nausea (in 2/35 patients).
No study reported major side effects following the use of virtual reality and no significant incident or fall was reported.
Criticism for the included studies
The games used in the virtual reality programs were not fully described as in Meldrum et al. [17] and Phillips et al. [19]. Also, most of the studies did not monitor or report the side effects of the rehabilitation programs, and some studies did not document clearly the time, and a number of sessions spent in rehabilitation or the time between sessions.
Conclusion
This systematic review and meta-analysis show that virtual reality as a vestibular rehabilitation measure has potential clinical benefit as it improves DHI, VSS-SF, VAS-SAT and posturography parameters in peripheral vestibular disorders, besides providing more satisfaction and pleasure than the conventional rehabilitative methods.
Recommendations
Further research is needed to document the exact parameters of an optimal protocol, the period needed for effective rehabilitation, and the number of sessions, as well as report the side effects of virtual reality in patients with peripheral vestibular dysfunction.
References
Hillier S, McDonnell M (2011) Vestibular rehabilitation for unilateral peripheral vestibular dysfunction; Cochrane Database Syst Rev. https://pubmed.ncbi.nlm.nih.gov/21328277/
Ricci N, Aratani M, Dona F, Macedo C, Caovilla H, Gananca F (2010) A systematic review about the effects of the vestibular rehabilitation in middle-age and older adults. Braz J Phys Ther 14(5):361–371
Badke M, Miedaner J, Shea T (2005) Effects of vestibular and balance rehabilitation on sensory organization and dizziness handicap. Ann Otol Rhinol Laryngol 114:48–54
Bamiou D, Luxon L (2008) Vertigo: clinical management and rehabilitation, 7th edn, pp 3791–3817
Nash E, Edwards G, Thompson J, Barfield W (2000) A review of presence and performance in virtual environments. Int J Hum Comput Interact 12(1):1–41
Whitney S, Sparto P, Hodges L, Babu S, Furman J, Redfern M (2006) Responses to a virtual reality grocery store in persons with and without vestibular dysfunction. CyberPsychol Behav 9(2):152–156
Tarr M, Warren W (2002) Virtual reality in behavioral neuroscience and beyond. Nat Neurosci 5(11):1089–1092
Morel M, Bideau B, Lardy J, Kulpa R (2015) Advantages and limitations of virtual reality for balance assessment and rehabilitation. Clin Neurophysiol 45(4–5):315–326
Meldrum D, Herdman S, Moloney R, Murray D, Duffy D, Malone K, McConn-Walsh R (2012) Effectiveness of conventional versus virtual reality based vestibular rehabilitation in the treatment of dizziness, gait and balance impairment in adults with unilateral peripheral vestibular loss: a randomised controlled trial. BMC Ear Nose Throat Disord 12(1):1–8
Gibbons E, Thomson A, de Noronha M, Joseph S (2016) Are virtual reality technologies effective in improving lower limb outcomes for patients following stroke—a systematic review with meta-analysis. Top Stroke Rehabil 23(6):440–457
Stanney K, Kennedy R, Drexleer J, Harm D (1999) Motion sickness and proprioceptive after effects following virtual environment exposure. Appl Ergon 30(1):27–38
Holden M (2005) Virtual environments for motor rehabilitation: review. Cyberpsychol Behav 8(3):187–211
Roettl J, Terlutter R (2018) The same video game in 2D, 3D or virtual reality—how does technology impact game evaluation and brand placements? PLoS ONE 13(7):e0200724. https://doi.org/10.1371/journal.pone.0200724
Page M, McKenzie J, Bossuyt P, Boutron I, Hoffmann T, Mulrow C (2020) The PRISMA statement: an updated guideline for reporting systematic reviews. Br Med J 372:n71
Schardt C, Adams M, Owens T, Keitz S, Fontelo P (2007) Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med Inform Decis Mak 7(1):1–6. https://doi.org/10.1186/1472-6947-7-16
Garcia A, Ganança M, Cusin F, Tomaz A, Ganança F, Caovilla H (2013) Vestibular rehabilitation with virtual reality in Ménière’s disease. Braz J Otorhinolaryngol 79(3):366–374
Meldrum D, Herdman S, Vance R, Murray D, Malone K, Duffy D, Glennon A, McConn-Walsh R (2015) Effectiveness of conventional versus virtual reality-based balance exercises in vestibular rehabilitation for unilateral peripheral vestibular loss: results of a randomized controlled trial. Arch Phys Med Rehabil 96(7):1319–1328
Micarelli A, Viziano A, Augimeri I, Micarelli D, Alessandrini M (2017) Three-dimensional head-mounted gaming task procedure maximizes effects of vestibular rehabilitation in unilateral vestibular hypofunction: a randomized controlled pilot trial. Int J Rehabil Res 40(4):325–332
Phillips J, Fitzgerald J, Phillis D, Underwood A, Nunney I, Bath A (2018) Vestibular rehabilitation using video gaming in adults with dizziness: a pilot study. J Laryngol Otol 132(3):202–206
Rosiak O, Krajewski K, Woszczak M, Jozefowicz-Korczynska M (2018) Evaluation of the effectiveness of a virtual reality-based exercise program for unilateral peripheral vestibular deficit. J Vestib Res 28(5–6):409–415
Stankiewicz T, Gujski M, Niedzielski A, Chmielik L (2020) Virtual reality vestibular rehabilitation in 20 patients with vertigo due to peripheral vestibular dysfunction. Med Sci Monit Int Med J Exp Clin Res 31:26
Castro A, Gazzola J, Natour J, Ganança F (2007) Versão brasileira do Dizziness Handicap Inventory. Pró-Fono revista de atualização científica. 19(1):97–104
Cusin F, Ganança M, Ganança F, Ganança C, Caovilla H (2010) Balance rehabilitation unit (BRUTM) posturography in Ménière’s disease. Braz J Otorhinolaryngol 76(5):611–617
Powell L, Myers A (1995) The activities-specific balance confidence (ABC) scale. J Gerontol Ser A Biol Sci Med Sci 50(1):28–34
Jacobson G, Newman C (1990) The development of the Dizziness Handicap Inventory. Arch Otolaryngol Head Neck Surg 116(4):424–427
Yardley L, Jahanshahi N, Hallam S (2004) Psychosocial aspects of disorders affecting balance and gait. Clin Disord Balance Posture Gait. 2:360–381
Bergeron M, Lortie C, Guitton M (2015) Use of virtual reality tools for vestibular disorders rehabilitation: a comprehensive analysis. Adv Med 3:1–9
Kinne B, Owens K, Rajala B, Ticknor S (2019) Effectiveness of home-based virtual reality on vestibular rehabilitation outcomes: a systematic review. Phys Ther Rev 24(6):280–290. https://doi.org/10.1080/10833196.2019.1647382
Heffernan A, Abdelmalek M, Nunez D (2021) Virtual and augmented reality in the vestibular rehabilitation of peripheral vestibular disorders: systematic review and meta-analysis. Sci Rep 11(1):1–11
Xie M, Zhou K, Patro N, Chan T, Levin M, Gupta M, Archibald J (2021) Virtual reality for vestibular rehabilitation: a systematic review. Otol Neurotol 42(7):967–977
Pavlou M, Kanegaonkar R, Swapp D, Bamiou D, Slater M, Luxon L (2012) The effect of virtual reality on visual vertigo symptoms in patients with peripheral vestibular dysfunction: a pilot study. J Vestib Res 22(5–6):273–281
Acknowledgements
None.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
NMH formulated the research question, refined the search algorithm, assisted in data collection and revised the manuscript; AFM conducted data collection, data analysis and revised the manuscript; EY conducted data collection, data analysis and drafted the manuscript; EG drafted the protocol, conducted data collection, revised data analysis and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest was declared by the authors.
Ethics approval and consent to participate
This study was approved by the research ethical committee (REC), Ain Shams University under number; FAW00017585.
Submission declaration and verification
This work has not been published previously.
Consent for publication
Not applicable.
Availability of data and material
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hazzaa, N.M., Manzour, A.F., Yahia, E. et al. Effectiveness of virtual reality-based programs as vestibular rehabilitative therapy in peripheral vestibular dysfunction: a meta-analysis. Eur Arch Otorhinolaryngol 280, 3075–3086 (2023). https://doi.org/10.1007/s00405-023-07911-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-07911-3