Abstract
Purpose
This study aimed to investigate the variability of the retrotympanum in patients undergoing surgical treatment for cholesteatoma.
Methods
We included 59 ears of patients undergoing middle ear surgery for cholesteatoma who had preoperative computed tomography scans. A retrospective analysis of the medical records was conducted. The sinus tympani (ST), subtympanic sinus (STS) and facial recess (FR) were classified into types A–C based on the relationship of their extension to the facial nerve. The mastoid and petrous apex were assessed and categorized as normal pneumatized or sclerotic.
Results
Type A extension was the most frequently found in all sinuses (ST 64%, FR 77%, STS 69%), Type B extension was found more often in ST (34%) and STS (24%) than in FR (15%). A very deep extension was found only rarely (ST 2%, FR 8%, STS 7%). A sclerotic mastoid was found in 67% of cases. Those cases showed a statistically significant difference regarding retrotympanum pneumatization when compared with normal mastoid.
Conclusion
The most frequent variant of retrotympanic pneumatization in relation to the facial nerve was type A in all subsites in cholesteatoma patients. The variability among patients with cholesteatoma is different to previously published results in healthy subjects. Moreover, the pneumatization of the retrotympanum is associated with mastoid pneumatization.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The retrotympanum represents the posterior wall of the tympanic cavity and hosts important anatomical structures, such as the facial nerve and the round window niche [1]. It is characterized by multiple bony bridges and sinuses, which show marked complexity and variability, as illustrated in Fig. 1. Moreover, middle ear diseases—especially cholesteatoma—frequently involve the retrotympanum [2]. Therefore, this hidden region of the middle ear plays an important role when performing surgical treatment of middle ear cholesteatoma. Owing to its localization and posterior extension, cholesteatoma removal is often surgically challenging. Indeed, several authors have shown that persistence of cholesteatoma is frequent in this region [3,4,5]. Accordingly, knowledge of the anatomy, its variability and the identification of difficult variants on preoperative computed tomography (CT) scans are important for planning and performing surgery.
The introduction of the endoscope for middle ear surgery allowed a greater insight into this hidden region, and endoscopic and radiologic classifications of subsites have recently been published. The current groupings classify the pneumatization of the sinus tympani (ST), sinus subtympanicus (STS) and facial recess (FR) in relation to the facial nerve as follows [6,7,8,9]:
-
Type A no extension of the sinus in relation to the level of the facial nerve.
-
Type B extension of the sinus posterior to the level of the facial nerve.
-
Type C extension medial and posterior to the level of the facial nerve.
The radiological presentation of these different types is illustrated in Fig. 2.
However, a recent comprehensive comparison between endoscopic visibility and radiologic extension revealed the limitations of endoscopic exploration of extensively pneumatized retrotympanic subsites [8, 9]. Even the use of 70° angled lenses did not permit the complete exploration of the sinus in cases of extensive pneumatization [9].
Furthermore, most classifications rely on data collected in healthy specimens of temporal bone. In contrast, most ears affected by cholesteatoma show some degree of reduced pneumatization [10]. We therefore hypothesized a difference in the anatomical variability of diseased ears as compared to the healthy specimens as reported in the literature.
Methods
Ethical issues
The local ethics committee reviewed and approved the present study (Kantonale Ethikkommission Bern 2019-00555) which was performed according to the Declaration of Helsinki [11].
Patients
Medical records from our tertiary referral center were retrospectively analyzed and details of patients undergoing endoscopic surgery of the middle ear for cholesteatoma were extracted (n = 84). Endoscopic cholesteatoma infiltration was based on reviewed surgical reports and videos. In cases of extension of the cholesteatoma to the mastoid, an additional retroauricular microscopic approach—canal wall up (CWU) was performed. In extensive cases with infiltration of the external auditory canal, lateral semicircular canal fistula or infiltration of the internal auditory canal, a canal wall down (CWD) tympanomastoidectomy was performed to completely eradicate the disease. For inclusion in the present study, patients had to have histological confirmation of cholesteatoma and a preoperative high-resolution temporal bone CT scan. Patients undergoing revision surgery for cholesteatoma were excluded (n = 16) as were patients without suitable preoperative imaging (n = 9).
Image acquisition
All in-house CT scans were acquired using our 128-slice CT scanner (SOMATOM1 Definition Edge; Siemens Healthcare, Erlangen, Germany). A certified reporting workstation (Sectra IDS7, Linköping, Sweden) was used for evaluation by the 2 neuroradiologists, who were blinded to the clinical data. All the images collected were of sufficiently good quality to allow an accurate assessment of the middle ear. The standard in-house temporal bone CT scan parameters (Somatom Edge, Siemens, Erlangen, Germany) are as follows: slice thickness (SL) 0.6.mm, field of view (FoV) 160 mm, total acquisition time of 1 s by tube current–time product of 230 mA, and tube voltage 120 kV. This resulted on average in a computed tomography dose index (CTDI) of 35 mGy and a dose–length product (DLP) of 330mGycm.
Image reconstruction according to our standard in-house temporal bone protocol included a soft tissue window (kernel J45s) and a bone window (kernel J70h) of the acquired CT scans, each in the axial, coronal, and an oblique (Stenvers) plane. For our retrospective data analysis, both neuroradiologists additionally reconstructed the CT scans in the multiplanar reconstruction mode (MPR-mode) to provide a different view of the ossicular chain, the retrotympanum and middle ear cavity. Both 2D and MPR3 were used for evaluation.
The external CTs of the temporal bone were scanned with a maximum of a SL 1 mm and a minimum of a SL 0.4 mm, the FoV differed between 150 and 250 mm with resulting range of exposure parameters.
Image analysis
Two board-certified neuroradiologists with more than 10 years of experience separately performed blinded imaging analysis. According to the classification described above, the tympanic sinus, subtympanic sinus and facial recess were classified as type A, B or C. After a first independent rating, a consensus meeting was held to review all cases subject to disagreement after which consensus was reached on all cases, resulting in a single rating per subsite. In addition, the mastoid part of the temporal bone was examined and classified: “normal pneumatization” for good pneumatization or hyperpneumatization and “sclerotic” for moderate pneumatization or hypopneumatization according to Dexian Tan et al. [12]. The petrous apex was examined and classified: “pneumatized” for pneumatized air cells medial to the labyrinth or “not pneumatized” for no air cells in the proximity of the inner ear as described by Dexian Tan et al. (2018). The data were analyzed using GraphPad Prism 9.2 (La Jolla, USA). Comparative statistics were performed with a two-tailed α set to < 0.05.
Results
Fifty-four patients were enrolled in the present study with a total of 59 affected ears. Of these, 56% were left ears. All patients underwent preoperative high-resolution CT scanning of the temporal bone, with a mean slice thickness of 0.63 mm (range 0.3–1 mm). The chosen surgical approach was exclusively endoscopic in 36 patients (61%), combined (endoscopic for middle ear and microscopic for mastoid surgery) CWU in 17 (29%) and combined CWD in 6 patients (10%). An endoscopic infiltration of the retrotympanum was observed in 30 ears (51%), requiring endoscopic cholesteatoma removal.
After the first round of image analysis and classification of the retrotympanic sinus into Type A, B or C by the experienced neuroradiologists as described above, there was disagreement of 49% for sinus tympani, 47% for facial recess and 24% for subtympanic space. A consensus meeting was held during which the retrotympanic spaces were re-classified. Finally, a consensus was achieved in all cases. Type A extension was most often observed in all sinuses. Type B extension was seen most often in the sinus tympani (34%). A very deep extension medial and posterior to the facial nerve was only rarely observed in any of the subsites, as summarized in Table 1 and illustrated in Fig. 3. Poor mastoid pneumatization was observed in 67% of the cases and the petrous apex was pneumatized in only 1 case.
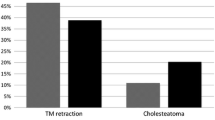
Comparison between cases with a sclerotic mastoid and those with a pneumatized mastoid revealed a statistically significant difference in pneumatization of the retrotympanum (p < 0.001). This association is illustrated in Fig. 4. No association between presence of disease in the retrotympanum and its anatomical variability was observed.
Discussion
This study investigated the variability of the retrotympanum in patients undergoing surgical treatment for cholesteatoma. The preoperative radiological analysis revealed the highest anatomical variability regarding extension of the retrotympanum in relation to the facial nerve in the sinus tympani. A type A extension was most common at all subsites. Patients with a sclerotic mastoid, indicating long-standing impairment of ventilation of the mastoid and the middle ear showed a significant difference in pneumatization as compared to patients with normal mastoid pneumatization. Therefore, an association between mastoid and retrotympanum pneumatization may be hypothesized on the basis of our results.
The retrotympanum is of particular interest to surgeons treating patients with chronic middle ear diseases and especially those with cholesteatoma. It is well known that the retrotympanum is the most frequent site of postoperative disease persistence [9], leading to continuous expansion of the cholesteatoma and a requirement for revision surgery. Therefore, a thorough knowledge of retrotympanic anatomy, appropriate preoperative planning and complete cholesteatoma removal are of the utmost importance in ensuring the best surgical outcome. The sinus tympani has been classified as a difficult access site in the most recent classification by the European and Japanese Otological Societies [13]. The introduction of endoscopes led to considerable advances in the surgical management of the retrotympanum allowing full exploration and cholesteatoma removal in most cases, as reported by Marchioni et al. [6]. So far, this is the only report on the morphological variability of the retrotympanum in patients with chronic middle ear disease. The subsequently published results and classifications of the retrotympanum were based on studies on cadavers of healthy donors [7, 8, 14]. The currently available results on retrotympanic variability are summarized in Table 2.
When comparing these data to our results in patients undergoing surgery for cholesteatoma, we observed a higher prevalence of Type A configuration in all retrotympanic subsites as follows: sinus tympani: 64% (literature: 52.5%), facial recess: 77% (literature: 59%) and subtympanic sinus: 69% (literature: 59%). Overall, Type A configuration was observed in 70% of cholesteatoma cases as compared to 59.5% in healthy ears.
Recently, Bonali et al. [9] investigated the correlation of radiologic configuration of the retrotympanic subsites to the visibility of the medial and posterior walls during a transcanal endoscopic approach. They revealed limitations of the endoscopic approach in deeply pneumatized retrotympanic spaces in healthy body donors. Even using 70° lenses it was not possible fully visualize a type C facial recess and subtympanic sinus in as many as 50% of the investigated ears. The sinus tympani was fully explorable using 70° lenses even in type C variants. This is clearly relevant to the surgical treatment of cholesteatoma in deeply pneumatized retrotympanic spaces. The surgeon needs to identify such cases preoperatively and, where necessary, to be prepared to perform a retrofacial approach to the middle ear to remove the cholesteatoma completely. However, according to our results, these deeply pneumatized variants appear to be even less frequent than previously reported. Interestingly, impaired pneumatization of the mastoid appeared to be associated with a less pneumatized retrotympanum in our cohort, when comparing cholesteatoma patients with sclerotic mastoid spaces to those with pneumatized ones. These findings are in line with a recently published study which found the pneumatization of the mastoid of patients with chronic otitis media was associated with the depth of the sinus tympani only [15]. Our study found that this association applied to the facial recess and the subtympanic sinus as well. However, involvement of the retrotympanum by cholesteatoma was not associated with its pneumatization.
Although our findings relevant to preoperative planning based on the high-resolution CT scans are important, image analysis and classification is challenging. In our experience, this applies even to expert neuroradiologists with many years of experience and; in our study, there was disagreement in many cases, requiring resolution at a consensus meeting. However, re-examination of the CT scans finally resulted in consensus regarding all cases. This finding is exemplary of the need for ear surgeons to be familiar with this kind of anatomy not only from a surgical, but also from a radiological perspective in order to correctly assess and interpret preoperative CT findings. In our opinion, it is important for every ear surgeon to interpret the CT images independently, especially if no experienced and appropriately trained neuroradiologists are available, otherwise important findings on the retrotympanum could be simply overlooked.
However, there are certain limitations of this study. One of the limitations of our study is its retrospective character and the lack of uniform CT scans of the temporal bone during the time period of CT acquisition. In addition, we are aware that the interpretation of a temporal bone CT, with its complex anatomy and microstructures, depends on the experience of the reader. Furthermore, previous description of anatomical variants of retrotympanic subsites were conducted in healthy cadaver specimens, leading to limited comparability with patients with chronic middle ear diseases.
Conclusion
In cholesteatoma patients, the most frequent variant of retrotympanic pneumatization in relation to the facial nerve is type A at all subsites. The variability of patients with disease is different to previously published results of studies in healthy subjects. Moreover, the pneumatization of the retrotympanum is associated with mastoid pneumatization. These findings may be especially important for preoperative planning of cholesteatoma resection in this difficult to access area of the middle ear.
References
Nogueira JF, Mattioli F, Presutti L, Marchioni D (2013) Endoscopic anatomy of the retrotympanum. Otolaryngol Clin N Am 46(2):179–188. https://doi.org/10.1016/j.otc.2012.10.003
Palva T (1990) The pathogenesis and treatment of cholesteatoma. Acta Otolaryngol 109(5–6):323–330. https://doi.org/10.3109/00016489009125151
James AL, Cushing S, Papsin BC (2016) Residual cholesteatoma after endoscope-guided surgery in children. Otol Neurotol 37(2):196–201. https://doi.org/10.1097/MAO.0000000000000948
Thomassin JM, Korchia D, Doris JM (1993) Endoscopic-guided otosurgery in the prevention of residual cholesteatomas. Laryngoscope 103(8):939–943. https://doi.org/10.1288/00005537-199308000-00021
Weiss MH, Parisier SC, Han JC, Edelstein DR (1992) Surgery for recurrent and residual cholesteatoma. Laryngoscope 102(2):145–151. https://doi.org/10.1288/00005537-199202000-00008
Marchioni D, Mattioli F, Alicandri-Ciufelli M, Presutti L (2009) Transcanal endoscopic approach to the sinus tympani: a clinical report. Otol Neurotol 30(6):758–765. https://doi.org/10.1097/MAO.0b013e3181b0503e
Alicandri-Ciufelli M, Fermi M, Bonali M et al (2018) Facial sinus endoscopic evaluation, radiologic assessment, and classification. Laryngoscope 128(10):2397–2402. https://doi.org/10.1002/lary.27135
Anschuetz L, Alicandri-Ciufelli M, Bonali M et al (2018) Novel Surgical and radiologic classification of the subtympanic sinus: implications for endoscopic ear surgery. Otolaryngol Head Neck Surg 159(6):194599818787180. https://doi.org/10.1177/0194599818787180
Bonali M, Fermi M, Alicandri-Ciufelli M et al (2020) Correlation of radiologic versus endoscopic visualization of the middle ear: implications for endoscopic ear surgery. Otol Neurotol 41(9):e1122–e1127. https://doi.org/10.1097/MAO.0000000000002787
Sato Y, Nakano Y, Takahashi S, Ikarashi H (1990) Suppressed mastoid pneumatization in cholesteatoma. Acta Otolaryngol Suppl 471:62–65. https://doi.org/10.3109/00016489009124811
World Medical A (2013) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310(20):2191–2194. https://doi.org/10.1001/jama.2013.281053
Dexian Tan A, Ng JH, Lim SA, Low DYM, Yuen HW (2018) Classification of temporal bone pneumatization on high-resolution computed tomography: prevalence patterns and implications. Otolaryngol Head Neck Surg 159(4):743–749. https://doi.org/10.1177/0194599818778268
Yung M, Tono T, Olszewska E et al (2017) EAONO/JOS Joint Consensus Statements on the definitions, classification and staging of middle ear cholesteatoma. J Int Adv Otol 13(1):1–8. https://doi.org/10.5152/iao.2017.3363
Bonali M, Anschuetz L, Fermi M et al (2017) The variants of the retro- and hypotympanum: an endoscopic anatomical study. Eur Arch Otorhinolaryngol 274(5):2141–2148. https://doi.org/10.1007/s00405-017-4492-0
Baklaci D, Kuzucu I, Guler I et al (2019) Effect of mastoid bone pneumatization on the conformation and depth of the sinus tympani, a high-resolution computed tomography study. Surg Radiol Anat 41(8):921–926. https://doi.org/10.1007/s00276-019-02246-3
Funding
Open access funding provided by University of Bern. No funding has been received for this study.
Author information
Authors and Affiliations
Contributions
S-LH: Data collection/management, data analysis, manuscript writing/editing and final approval. SB: data collection, manuscript writing/editing, final approval of manuscript. AH: data collection/management, data analysis, final approval of manuscript. AY: protocol/project development, data collection, final approval of manuscript. MC: protocol/project development, critical review and final approval of manuscript. Franca Wagner: Data collection/management, data analysis, critical review and final approval of manuscript. LA: protocol/project development, data collection/management, data analysis, manuscript writing/editing, final approval of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
L. Anschuetz is a consultant physician for STRYKER ENT. He has not received any financial compensation for his contribution to this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hool, SL., Beckmann, S., Hakim, A. et al. Variability of the retrotympanum and its association with mastoid pneumatization in cholesteatoma patients. Eur Arch Otorhinolaryngol 280, 131–136 (2023). https://doi.org/10.1007/s00405-022-07465-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07465-w