Abstract
Purpose
The purpose is to analyze the incidence of acute infectious supraglottitis in our center between 2010 and 2020, define the characteristics and trends of those patients and identify factors associated with the need of airway intervention.
Methods
A retrospective single-center observational study of a cohort of patients diagnosed with acute infectious supraglottitis between January 2010 and December 2020. Patients were stratified according to airway management.
Results
Eighty eight patients were included: 59 men (67%) and 29 women (33%). A significant upward trend of 9% in the annual incidence rate of supraglottitis was seen during 2010–2020, with an important increase in cases during 2019. Muffled voice (41%) and respiratory distress (38%) were the most common presenting symptoms; and the median duration of symptoms before hospital admission was 2 days [IQR 1; 3]. Airway intervention was performed in fifteen patients (17%). Nine patients (10%) were intubated and six required tracheotomy (7%). Comparing the patients who required airway intervention with those who received a conservative treatment, younger patients (p < 0.01) were more likely to need airway intervention. In logistic regression analysis, we found that epiglottic abscess (p = 0.015), hypersalivation (p = 0.027) and smoking (p = 0.036) were independent factors with a significant association with airway intervention.
Conclusion
There was an important increase in cases and its severity in 2019, but due to COVID-19 pandemic, it was not possible to define if it was an isolate event or an upward trend. Epiglottic abscess, hypersalivation and smoking could be possible risk factors for airway intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute infectious supraglottitis, also known as epiglottitis, is a severe disease that can be life-threatening due to its risk of airway obstruction. Both terms have been used to refer to the same condition, but it is considered more accurate to term it acute supraglottitis, as it is an inflammation of the supraglottic region [1]. According to the literature, the overall incidence of this illness has not changed significantly [2, 3], but after the introduction of vaccination against Haemophilus influenzae, the incidence has decreased in pediatric population and increased in adults [2, 4]. It has been reported that around 10% of cases are severe and may require airway intervention [4, 5].
The main objective of this study is to analyze the incidence of cases of acute infectious supraglottitis in our center between 2010 and 2020, focusing on the variation in incidence and severity in the recent years. Secondary objectives are to define the characteristics and trends of this disease in our population of study, and the factors related to the need for airway intervention.
Methods
This study received approval from the institutional ethics committee. We conducted a single-center, retrospective observational study of a cohort of all patients diagnosed with acute infectious supraglottitis between January 2010 and December 2020 in our center. We performed a systematic review of the medical records of all patients evaluated in the emergency department and/or admitted to the hospital with a diagnostic code for infectious supraglottitis or epiglottitis. Inclusion criteria were symptoms suggestive of acute supraglottitis of infectious origin in patients older than 16 years. We excluded those patients with findings not consistent with infective supraglottitis, such as those caused by chemicals, trauma or allergic reactions. We also excluded patients with a history of head and neck neoplasia and/or previous cervical radiotherapy to avoid bias. Patients were stratified according to whether they required invasive airway maneuvers or conservative treatment was carried out. Data collection was performed from medical records. The information collected included sex, date of birth, date of consultation, body mass index (BMI), comorbidities and smoke status, history of previous supraglottitis, initial examination diagnosis and disease extension (“supraglottic swelling,” “only epiglottic swelling”, “epiglottic abscess”), antibiotic and corticosteroid treatment and its duration, severe symptoms on arrival (hypersalivation, voice change, stridor, respiratory distress) and its duration, initial management, airway management, days of admission, microbiology, evolution and complications. The initial diagnosis of “supraglottic swelling”, “only epiglottic swelling” and “epiglottic abscess” was performed using transnasal flexible laryngoscopy in all cases, and in selected patients also accompanied by a computed tomography (CT) scan. Criteria used to stratify the patients were: “supraglottic swelling” was defined as swelling of more than one supraglottic structure (epiglottis, arytenoid, false vocal cord, aryepiglottic fold or vallecula), “only epiglottic swelling” as swelling of epiglottis without swelling of other supraglottic structures, and “epiglottic abscess” as the presence of an abscess in the epiglottis.
Antibiotic treatment was prescribed according to the clinical practice protocols of our center. The therapeutic algorithm used as a general rule but with individualization in each patient was: patients without severe symptoms on arrival and without risk factors (immunosuppression or diabetes) were treated with amoxicillin with clavulanic acid; those with severe symptoms on arrival and without risk factors received treatment with third generation cephalosporin as monotherapy; and patients who were immunosuppressed, diabetic or had epiglottic abscesses were treated with third generation cephalosporin with metronidazole. We used other antibiotic treatments (quinolones, piperacillin with tazobactam) in patients allergic to penicillins or with resistant cultures. All patients received corticosteroids as initial treatment (bolus of 100 mg hydrocortisone), followed by 40 mg of methylprednisolone every 12 h until clinical improvement. We did not maintain corticosteroid treatment in patients who required drainage of an epiglottic abscess. A few patients had microbiological cultures taken since we do not routinely perform cultures on all supraglottitis patients at our center. Cultures were collected from epiglottic abscesses drained in the operating room under direct laryngoscopy and blood cultures from patients who were admitted to the intensive care unit (ICU).
Categorical variables were described using the number of observations and percentage. Continuous variables were evaluated for normal distribution using histogram. Normally distributed variables were described using mean and standard deviation (SD), and non-normally distributed variables were described using median and interquartile range (IQR).
Categorical variables were compared using the chi-squared test. Continuous non-normal variables were compared with Wilcoxon–Mann–Whitney test and normal variables using T test. To analyze the number of cases per year, a Poisson regression analysis was performed. Logistic regression was used to assess which variables were associated with airway intervention. Data management and statistical analyses were performed using R software 3.6.3 version and p value < 0.05 was considered as statistically significant.
Results
Demographics and comorbidities
A total of 148 patients were identified, of which 60 patients were excluded, as they did not meet the inclusion criteria. The study included 88 patients, 59 men (67%) and 29 women (33%), with a male to female ratio of 2.03:1. The average age at the time of diagnosis was 53 years (SD 15.59).
Sixteen patients (18%) reported a history of diabetes mellitus; one of them was also diagnosed of multiple myeloma. One patient was immunosuppressed because of cardiac transplantation. Median BMI in our cohort was 29 [IQR 26.13; 32.89]. Thirty-eight patients (43%) were smokers, and one patient had a previous episode of supraglottitis (Table 1).
The incidence of patients with acute supraglottitis admitted to our hospital showed a significant upward trend of 9% in the annual incidence rate of supraglottitis in the period 2010–2020 [IRR = 1.09; 95%CI = (1.02–1.16)], as we can see in Fig. 1. The average number of cases per year excluding 2019 was seven cases. In 2019, 17 cases were diagnosed, showing a significant increase compared to the other years studied.
Comparing the incidence by disease extension (Fig. 1), we could observe that during year 2015 a high proportion of patients presented only epiglottic swelling (83%) and that in year 2019 there were more patients presenting swelling of all supraglottic structures (53%) compared to the other years (37%). Another difference was that hypersalivation was present in 29% of patients in 2019, and 14% during the other years.
Symptoms and signs
Muffled voice (41%) and respiratory distress (38%) were the most common presenting symptoms (Table 1). The median duration of symptoms before hospital admission was 2 days [IQR 1;3].
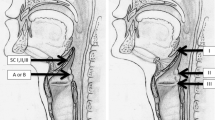
Diagnosis was made by flexible laryngoscopy in all patients, and if an epiglottic abscess was suspected, a cervical CT scan was performed (Fig. 2). Swelling of all supraglottic structures was present in 35 patients, 37 patients had only epiglottic swelling and 16 patients presented an epiglottic abscess.
Microbiology
Cultures were obtained in 17 patients (19%) and 4 patients tested positive (4 cultures of epiglottic abscesses and 1 blood culture). Three of the cultures from epiglottic abscesses were polymicrobial infections and one was positive for Candida albicans, Prevotella denticola and lactobacillus. The blood culture was positive for Streptococcus pneumoniae. Haemophilus influenzae was not isolated in any subject.
Treatment
The most frequently used antibiotic agent was amoxicillin with clavulanic acid in 41 patients (47%), followed by third generation cephalosporin as monotherapy in 21 patients (24%) and third generation cephalosporin with metronidazole in 18 patients (20%). All patients received intravenous corticosteroids.
Airway intervention
Fifteen patients underwent airway intervention (17%). Nine patients (10%) were intubated, eight in the operating room and one in the emergency room. Five of them also required transoral drainage of an epiglottic abscess. Four patients (5%) required emergency tracheostomy, three of them in the operating room and one in the emergency room after a failed intubation attempt; and two more patients (2%) required non-emergency tracheostomy with cervical drainage of an abscess. A total of six tracheotomies were performed (7%).
During year 2019, nine patients (53%) required airway intervention. Five of the other patients that required airway intervention were diagnosed in 2013, being a 63% of the total of patients that year, and they all had an epiglottic abscess that required drainage. One patient in 2020 required airway intervention (14%).
Younger patients (p < 0.01) and patients with epiglottic abscess (p = 0.01) were more likely to require airway intervention (Table 2). A logistic regression was performed in order to analyze the associated factors with airway intervention (Table 3). Epiglottic abscess was found to be a possible risk factor for airway intervention [OR = 8.31; IC95% = (1.65–53.40)], as well as smoking [OR = 5.15; IC95% = (1.24–28.80)] and hypersalivation [OR = 5.69; IC95% = (1.24–28.70)].
Figure 3 shows the predicted probabilities for airway intervention in relation to disease extension and age. Figure 4 illustrates the same predicted probabilities, but in relation to disease extension and days with symptoms before hospital admission. Patients with epiglottic abscess show higher probabilities of airway intervention in both figures. In Fig. 3, younger patients show a higher probability of airway intervention in the three groups of disease extension, mainly in the group “epiglottic abscess” (60% of probability). Patients with fewer days with symptoms before hospital admission have a higher probability of airway intervention in the three groups of disease extension (Fig. 4).
Predicted probability curves of airway intervention in relation to disease extension and age. These curves show the probability in our cohort of patients that a patient, according to age and disease extension, would require airway intervention. For example, a 20-year-old patient with an epiglottic abscess has a 60% of probability of airway intervention, and the same patient with supraglottic swelling a 25% of probability
Predicted probability curves of airway intervention in relation to disease extension and days with symptoms before hospital admission. These curves show the probability in our cohort of patients that a patient, according to days with symptoms before hospital admission and disease extension, would require airway intervention. For example, a patient with an epiglottic abscess and symptoms that started less than 24 h before hospital admission has almost a 70% of probability of airway intervention, while patients with other supraglottitis extensions have a probability of around 20%
Outcomes
Median duration of hospitalization was 5 days [IQR 4;7]. Seventy-nine patients (90%) had a good outcome and were discharged with outpatient follow-up. Three patients (3%) presented clinical worsening, requiring drainage of an abscess. Four patients (5%) requested voluntary discharge after treatment and improvement of their symptomatology, thus losing their follow-up.
Of the four patients who underwent emergency tracheostomy, two of them presented fatal complications. One patient died (1%) after a cardiorespiratory arrest during tracheostomy procedure in the operating room. The other patient presented with a post-anoxic encephalopathy (1%) after performing a tracheostomy in the emergency room following a failed intubation attempt. The delay in attending an emergency department, and the fact that they presented severe and critical symptoms when they were assessed, resulted in a fatality in both cases. In addition, both patients were obese and had very difficult cervical access.
Discussion
Nowadays, supraglottitis remains a dangerous disease that can lead to a low, but non-negligible, morbidity and mortality. Despite some principal characteristics of the disease have changed after widespread Haemophilus influenzae vaccination, the airway management and its complexities keep being the key point in the treatment of this disease. In the present study, we attempted to show the characteristics and trends of adult supraglottitis in our population of study during the last 11 years and to identify factors associated with the intervention.
Epidemiological analyses revealed a male to female ratio of 2.03:1 in our cohort, which is consistent with previous studies that reported ratios from 1,1:1 to 4:1. [3, 6, 7], showing a higher proportion of supraglottitis in male population. The mean age at diagnosis of our patients was 53 years, with similar results to others published [1, 4, 8,9,10].
An increased incidence of supraglottitis after widespread vaccination against Haemophilus influenzae was described in several papers [2,3,4,5]. Some authors attributed it to an increased identification of the disease due to greater physician awareness and/or improved diagnostic tools with the use of flexible laryngoscopy [5, 11], but others supported that there was a real rise in the incidence [3, 12]. An upward trend of 9% in the annual incidence rate of supraglottitis between 2010 and 2020 was seen in the present study; with an important increase in cases and in its severity during year 2019, and a drop in incidence in 2020 that could be attributed to public health measures due to Covid-19 pandemic. Flexible laryngoscopy was routinely used in all our patients avoiding bias, supporting the fact that there was a real increase in the incidence of supraglottitis in the last years, being consistent with findings published by Vaid et al. [12].
After the widespread use of Haemophilus influenzae vaccine in 1995 [2], a change in infectious supraglottitis etiology was observed, previously being the 75–90% due to this bacterium [8, 13]. At present, although H. influenzae continues to be one of the etiological agents, mainly in relation to vaccination failures and loss of herd immunity, there are other causal pathogens, like Streptococcus pneumoniae, Streptococcus pyogenes and Staphylococcus aureus [2, 13]. In our study, cultures were obtained in 17 out of 88 patients and only 4 patients had positive culture results, as microbiological cultures were not routinely performed in all patients. Previous published studies [8, 14] had similar results in terms of culture collection rates and culture positivity. It can be explained because of the emergency situation when faced with a patient with supraglottitis, the fact that surface cultures of the epiglottis have really low sensitivity, and that blood cultures are not a good diagnostic tool when patients started with antibiotics before culture is obtained [2]. In our study, it was not possible to identify a predominant pathogen responsible for the infections or to relate it to the increase of cases and its severity during 2019. None of our patients had a Haemophilus influenzae positive culture, which could be attributed to a correct immunity against Haemophilus influenzae in our area.
Antibiotics in supraglottitis are typically aimed at treating Haemophilus influenzae, Streptococcus pyogenes and Streptococcus pneumoniae [2]. On the other hand, use of corticosteroids is controversial. Guardiani et al. [2] demonstrated that steroid use reduces ICU and hospital stay, but other studies did not show any reduction in intubation duration or ICU stay [3, 11]. Most of our patients were treated with amoxicillin and clavulanic acid, and all of them with intravenous corticosteroids, with a good clinical response.
Laryngoscopy, especially transnasal flexible laryngoscopy, is considered the best way to evaluate the airway and perform diagnosis and assessment of supraglottitis [10]. In our study, we divided our patients in relation to the different laryngeal subsites that were affected with the infection. We found that epiglottic abscess was a risk factor for airway intervention. Neither swelling of all supraglottic structures nor only epiglottic swelling showed any correlation with airway intervention; moreover, their behavior on the predicted probability curves (Figs. 3 and 4) was very similar. Different scoring systems for prediction of airway intervention have been proposed in the literature [15], but none of them could be applied in our study due to its retrospective design.
Of 88 adult patients with acute infectious supraglottitis in our study population, 15 patients (17%) required airway intervention. Sideris et al. [5], in their meta-analysis, found that the overall prevalence of airway intervention in the post-vaccine era was 10.9%, although the overall prevalence from all studies taken into account in the meta-analysis between 1986 and 2017 was 15%. On the other hand, there are other single studies [2, 16] in the post-vaccine era with more than a 20% of airway intervention. In our cohort, the prevalence of airway intervention excluding year 2019 was 8%, which reflects that year 2019 had a really important impact on the high rate of airway intervention in our study.
All patients requiring airway intervention were admitted in the years 2013, 2019 and 2020. It was not possible to define the exact causes of the concentration of airway intervention in 2013 and 2019, apart from the presence of the previously defined risk factors for airway intervention. However, one can hypothesize that this may have been due to the presence of more virulent pathogens causing more inflammation and abscess formation, as well as a more interventionist trend in 2019 due to previous experience with cases that presented with adverse outcomes.
It is difficult to know whether the high increase in incidence and severity in supraglottitis during 2019 was an isolated event or whether it is an upward trend. Public health measures adopted in 2020 due to COVID-19 pandemic may have reduced the number of infections and, therefore, interfered with the 2020 data [12], so the incidence and severity of infectious supraglottitis need to be studied in the coming years to be able to define the real situation.
In addition, a recent study published by Piersiala et al. [17] described that the Omicron variant of SARS-CoV-2 virus, in some patients, presents with clinical manifestations similar to symptoms of supraglottitis, but without having upper airway edema. In such cases, a prompt examination of the larynx is essential to establish the correct diagnosis.
Intubation was performed in nine of the patients who required airway intervention. Most patients were intubated in the operating room with an otolaryngology surgical team ready to perform a tracheotomy, and one patient had to be intubated in the emergency room. A tracheostomy was performed in 6 of 88 patients (7%), which is consistent with other studies such as Suzuki et al. [4] who found 7.7% of patients requiring tracheostomy. Furthermore, Sideris et al. [5] in their meta-analysis described a 5.46% prevalence of tracheotomy, with a 4.53% taking into account only the post-vaccine era. However, other studies reported a lower proportion of tracheotomies, ranging from 0.9 to 2.89% [1, 6]. A study published by Tapiovaara et al. [9] reported that tracheotomy was a more economical way to manage the airway, and they did not encounter any significant difference in complication rates between intubation and tracheotomy.
In our study population, young age and the presence of epiglottic abscess were associated with airway intervention on univariate analysis. Epiglottic abscess was also associated with airway intervention on logistic regression analysis, as well as smoking and hypersalivation. Epiglottic abscess and hypersalivation have been previously described as possible predictors of airway intervention [3, 11, 18]. Although previous studies showed that smoking could be a possible risk factor for supraglottitis admission [4, 19], our study further showed an association between tobacco and airway intervention. Our results also suggested that the probability of airway intervention decreases in older patients. This could be explained because age may reduce acute inflammatory response [20], which could decrease the risk of sudden upper airway obstruction in supraglottitis.
We developed predicted probability curves showing the likelihood, in our cohort of patients, that a patient would require airway intervention. Previous investigations [2, 11] demonstrated that a shorter duration of symptoms was associated with a higher risk of airway intervention, probably in relation to a more aggressive course of the disease; but in our study it was only a tendency, without being able to have statistical significance. However, predicted probabilities of airway intervention shown in Figs. 3 and 4, demonstrate that patients with symptoms that started less than 24 h before hospital admission have higher probabilities of airway intervention requirements. The presence of epiglottic abscess and lower age also plays an important role in the risk of airway intervention (Figs. 3 and 4). Taking into account their important limitations, these figures could be used as a tool to estimate the risk of airway intervention according to the three parameters mentioned above.
The vast majority of our patients had a good clinical outcome, although three of them presented clinical worsening requiring drainage of an abscess (3%) without subsequent complications. One patient of the study had a post-anoxic encephalopathy (1%) after a failed intubation attempt that required emergency tracheostomy, and another patient died (1%) after a cardiorespiratory arrest during emergency tracheostomy procedure. The meta-analysis of Sideris et al. [5] describes an overall 1.5% mortality rate, which is consistent with our results. Some papers also described post-anoxic encephalopathy in relation to airway collapse [15, 21], like in our study. A previous study [4] showed that BMI > 25 kg/m2 is an independent risk factor for developing severe epiglottitis and is associated with relatively higher 2-day mortality. Furthermore, another study [22] demonstrated a linear association between upper airway caliber and BMI after adjustment for lung volume, which suggests that the airways become narrower with increasing BMI, and that could explain the extreme airway emergency in the abovementioned patients [4].
The findings of this study must be seen in light of some limitations. The main limitation is the retrospective design of the study, similar to the current literature available about this disease. Due to its low prevalence and high severity, it is difficult to perform prospective and randomized studies. Furthermore, description of symptoms and extension of the disease, management decisions and the assessment of airway intervention were subject to individual clinician bias. Additionally, although this study is one of the largest reported, its small sample makes it difficult to obtain statistically significant results in some cases.
Conclusion
There has been an increase in the incidence of supraglottitis in the recent years in our center. In the present study, we found an upward trend of 9% in the annual incidence rate of supraglottitis, with an important increase in cases and its severity in 2019. However, public health measures due to COVID-19 pandemic interfered with the results in 2020, requiring further studies in the following years.
Defining patients who may present a severe supraglottitis and require airway intervention remains the key point in the management of this disease nowadays. Our results showed that patients with an epiglottic abscess, smokers and patients with hypersalivation might have an increased risk of requiring airway intervention. Younger age and shorter duration of symptoms before hospital admission also seem to have a tendency for a greater risk of airway intervention, but without statistical significance. We defined predicted probability curves that, considering their limitations, could be used as a tool to estimate the risk of airway intervention in relation to disease extension, age and days with symptoms before hospital admission. This information can help physicians predict which patients are most likely to require airway intervention and act with caution.
Further prospective multicenter studies are required to support the results of the current research: establish the risk factors for airway intervention, confirm the apparent increase in cases in recent years and set up new management and treatment strategies.
Availability of data and material
Not applicable.
Code availability
R-free software 3.6.3 version.
References
Ringel B, Shilo S, Carmel-Neiderman NN et al (2020) Low rates of airway intervention in adult supraglottitis: a case series and meta-analysis. Am J Otolaryngol 41(4):102482. https://doi.org/10.1016/j.amjoto.2020.102482
Guardiani E, Bliss M, Harley E (2010) Supraglottitis in the era following widespread immunization against Haemophilus influenzae type B: evolving principles in diagnosis and management. Laryngoscope 120(11):2183–2188. https://doi.org/10.1002/lary.21083
Berger G, Landau T, Berger S, Finkelstein Y, Bernheim J, Ophir D (2003) The rising incidence of adult acute epiglottitis and epiglottic abscess. Am J Otolaryngol 24(6):374–383. https://doi.org/10.1016/S0196-0709(03)00083-8
Suzuki S, Yasunaga H, Matsui H et al (2015) Factors associated with severe epiglottitis in adults: analysis of a Japanese inpatient database. Laryngoscope 125:2072–2078. https://doi.org/10.1002/lary.25114
Sideris A, Holmes TR, Cumming B, Havas T (2020) A systematic review and meta- analysis of predictors of airway intervention in adult epiglottitis. Laryngoscope 130(2):465–473. https://doi.org/10.1002/lary.28076
Guldfred LA, Lyhne D, Becker BC (2008) Acute epiglottitis: epidemiology, clinical presentation, management and outcome. J Laryngol Otol 122(8):818–823. https://doi.org/10.1017/S0022215107000473
Shaikh N, Nawaz S, Ahmad K, Al Maslamani M (2020) Acute adult supraglottitis: an impending threat to patency of airway and life. Cureus 12(8):e9976. https://doi.org/10.7759/cureus.9976
ShapiraGalitz Y, Shoffel-Havakuk H, Cohen O, Halperin D, Lahav Y (2017) Adult acute supraglottitis: analysis of 358 patients for predictors of airway intervention. Laryngoscope 127(9):2106–2112. https://doi.org/10.1002/lary.26609
Tapiovaara LK, Aro KLS, Bäck LJJ, Koskinen AIM (2019) Comparison of intubation and tracheotomy in adult patients with acute epiglottitis or supraglottitis. Eur Arch Otorhinolaryngol 276(11):3173–3177. https://doi.org/10.1007/s00405-019-05624-0
Hanna J, Brauer PR, Berson E, Mehra S (2019) Adult epiglottitis: trends and predictors of mortality in over 30 thousand cases from 2007 to 2014. Laryngoscope 129(5):1107–1112. https://doi.org/10.1002/lary.27741
Mayo Smith MF, Spinale JW, Donskey CJ, Yukawa M, Lifjhfk RH, Schiffman FJ (1995) Acute epiglottitis. An 18-year experience in Rhode Island. Chest 108(6):1640–1647. https://doi.org/10.1378/chest.108.6.1640
Vaid P, Farrell E, Donnelly M (2021) Predictors of airway intervention in acute supraglottitis (AS), a recent 7- year experience. Am J Otolaryngol 42(6):103084. https://doi.org/10.1016/j.amjoto.2021.103084
Shah RK, Roberson DW, Jones DT (2004) Epiglottitis in the Hemophilus influenzae Type B vaccine era: changing trends. Laryngoscope 114(3):557–560. https://doi.org/10.1097/00005537-200403000-00031
Baird SM, Marsh PA, Padiglione A et al (2018) Review of epiglotitis in the post Haemophilus influenzae type-b vaccine era. ANZ J Surg 88(11):1135–1140. https://doi.org/10.1111/ans.14787
Nonomura M, Yoshizawa A, Mizuta M, Sat S (2021) Comparison of scope classifications for predicting the need for airway intervention in acute supraglottitis. Int J Pract Otolaryngol 04(01):e6–e10. https://doi.org/10.1055/s-0041-1722883
Cheung CS, Man SY, Graham CA et al (2009) Adult epiglotitis : 6 year experience in a university teaching hospital in Hong Kong. Eur J Emerg Med 16:221–226. https://doi.org/10.1097/MEJ.0b013e328320ad2f
Piersiala K, Kakabas L, Bruckova A, Starkhammar M, Cardell LO (2022) Acute odynophagia: a new symptom of COVID-19 during the SARS-CoV-2 Omicron variant wave in Sweden. J Intern Med. https://doi.org/10.1111/joim.13470
Sideris G, Delides A, Maragkoudakis P, Papadimitriou N (2021) Analysis of prognostic factors for airway intervention in 140 patients with acute supraglottitis. Eur Ann Otorhinolaryngol Head Neck Dis. https://doi.org/10.1016/j.anorl.2021.02.012
Shah RK, Stocks C (2010) Epiglotitis in the United States: national trends, variances, prognosis and management. Laryngoscope 120:1256–1262. https://doi.org/10.1002/lary.20921
Laflamme C, Mailhot GB, Pouliot M (2017) Age-related decline of the acute local inflammation response: a mitigating role for the adenosine A2A receptor. Aging 9(10):2083–2097. https://doi.org/10.18632/aging.101303
Mathoera RB, Wever PC, van Dorsten FRC, Balter SGT, de Jager CPC (2008) Epiglotitis in the adult patient. Neth J Med 66(9):373–377
King GG, Brown NJ, Diba C et al (2005) The effects of body weight on airway calibre. Eur Respir J 25:896–901. https://doi.org/10.1183/09031936.05.00104504
Acknowledgements
The authors would like to gratefully acknowledge the priceless work in the clinical and surgical management of the patients in the study, as well as the excellent support received from the study collaborators: Enric Cisa, Henry Rafael Lares, Francesc Cruellas, Anna Farré, Ricardo Bartel, Jose Maria Caballero, Marta Fulla, Mireia Golet, Miriam Hamdan, Javier Skufca and Jordi Tornero.
Funding
This study has not been funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethics approval
This single-centre retrospective study was conducted in accordance with ethical guidelines of the Declaration of Helsinki and was approved by the Institutional Ethics Committee (PR001/21). Due to the retrospective nature of the study and the fact that it did not present any changes in the evolution and management of the patients, it was not considered necessary to obtain informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Penella, A., Mesalles-Ruiz, M., Portillo, A. et al. Acute infectious supraglottitis in adult population: epidemiology, management, outcomes and predictors of airway intervention. Eur Arch Otorhinolaryngol 279, 4033–4041 (2022). https://doi.org/10.1007/s00405-022-07365-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07365-z