Abstract
Purpose
This study aims to reveal changes in the incidence and prognosis of patients with tonsillar lymphoma on a population level.
Methods
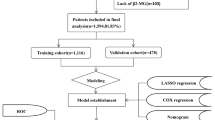
The incidence, clinicopathological, and prognostic data of tonsillar lymphoma patients were extracted from the Surveillance, Epidemiology, and End Results (SEER) database. The Join-point software and R packages were utilized to analyze the annual percentage changes (APCs) and survival outcomes.
Results
The incidence of primary tonsillar lymphoma increased from 0.1204 per 100,000 person-years (95% CI, 0.0680–0.1962) in 1983 to 0.2158 (95% CI, 0.1675–0.2740) in 2015 with an APC of 1.20. When classified by decades, both cancer-specific survival (CSS) and overall survival (OS) improved with time. The 2006–2015 decade showed the highest rate of CSS and OS. Nevertheless, for disease-specific survival (DSS), the difference was not significant between 1996–2005 and 2006–2015 decades. The main cause of mortality among this cohort was heart diseases. Three nomograms were constructed to predict OS, CSS, and DSS for patients with primary tonsillar lymphoma, respectively. Histological subtype made the most contribution to poor prognosis in OS-predicting and CSS-predicting nomograms. While, for DSS, age at diagnosis made the most contribution to poor outcomes.
Conclusions
The incidence of primary tonsillar lymphoma has increased in the past decades. The OS and CSS rates of tonsillar lymphoma improved continuously, while there was no significant improvement in DSS in the past decades. These changes indicated an improved management of tonsillar lymphoma with newer therapeutic agents and the need of multi-disciplinary treatments to offset the future burden of noncancer diseases.




Similar content being viewed by others
Data availability
Data were publicly accessible which can be obtained in the SEER database.
Abbreviations
- SEER:
-
The Surveillance, Epidemiology, and End Results (SEER) database
- APC:
-
Annual percentage changes
- CSS:
-
Cancer-specific survival
- OS:
-
Overall survival
- DSS:
-
Disease-specific survival
- NHL:
-
Non-Hodgkin’s lymphoma
- HL:
-
Hodgkin’s lymphoma
- CI:
-
Confidence interval
- DLBCL:
-
Diffuse large B cell lymphoma
References
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics, 2020. CA Cancer J Clin 70(1):7–30. https://doi.org/10.3322/caac.21590
Yuen A, Jacobs C (1999) Lymphomas of the head and neck. Semin Oncol 26(3):338–345
Kirsch JP, Miller RH, Blair PA (1991) Histiocytic non-Hodgkin’s lymphoma of Waldeyer’s ring. Otolaryngol Head Neck Surg 105:777–780. https://doi.org/10.1177/019459989110500602
Rosenberg SA, Diamond HD, Jaslowitz B, Craver LF (1961) Lymphosarcoma: a review of 1269 cases. Medicine 40:31–84. https://doi.org/10.1097/00005792-196102000-00002
López-Guillermo A, Colomo L, Jiménez M, Bosch F, Villamor N, Arenillas L, Muntañola A, Montoto S, Giné E, Colomer D, Beà S, Campo E, Montserrat E (2005) Diffuse large B-cell lymphoma: clinical and biological characterization and outcome according to the nodal or extranodal primary origin. J Clin Oncol 23:2797–2804. https://doi.org/10.1200/JCO.2005.07.155
Lee YH, Cho SG, Jung SE, Kim SH, Hyun OJ, Park GS, Yang SW, Lee IS, Rhee CK, Choi BO (2016) Analysis of treatment outcomes for primary tonsillar lymphoma. Radiat Oncol J 34:273–279. https://doi.org/10.3857/roj.2016.01781
Yahalom J, Illidge T, Specht L, Hoppe RT, Li YX, Tsang R, Wirth A (2015) Modern radiation therapy for extranodal lymphomas: field and dose guidelines from the International Lymphoma Radiation Oncology Group. Int J Radiat Oncol Biol Phys 92:11–31. https://doi.org/10.1016/j.ijrobp.2015.01.009
Tan LH (2004) Lymphomas involving Waldeyer’s ring: placement, paradigms, peculiarities, pitfalls, patterns and postulates. Ann Acad Med Singap 33(4 Suppl):15–26
Gurkaynak M, Cengiz M, Akyurek S, Ozyar E, Atahan IL, Tekuzman G (2003) Waldeyer’s ring lymphomas: treatment results and prognostic factors. Am J Clin Oncol 26:437–440. https://doi.org/10.1097/01.coc.0000027588.56104.15
White MC, Babcock F, Hayes NS, Mariotto AB, Wong FL, Kohler BA, Weir HK (2017) The history and use of cancer registry data by public health cancer control programs in the United States. Cancer 123(Suppl 24):4969–4976. https://doi.org/10.1002/cncr.30905
Thomas A, Link BK, Altekruse S, Romitti PA, Schroeder MC (2017) Primary breast lymphoma in the United States: 1975–2013. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djw294
Kim HJ, Fay MP, Yu B, Barrett MJ, Feuer EJ (2004) Comparability of segmented line regression models. Biometrics 60:1005–1014. https://doi.org/10.1111/j.0006-341X.2004.00256.x
Dohar JE, Bonilla JA (1996) Processing of adenoid and tonsil specimens in children: a national survey of standard practices and a five-year review of the experience at the Children’s Hospital of Pittsburgh. Otolaryngol Head Neck Surg 115(1):94–97. https://doi.org/10.1016/S0194-5998(96)70143-2
Dolev Y, Daniel SJ (2008) The presence of unilateral tonsillar enlargement in patients diagnosed with palatine tonsil lymphoma: experience at a tertiary care pediatric hospital. Int J Pediatr Otorhinolaryngol 72:9–12. https://doi.org/10.1016/j.ijporl.2007.09.001
Toader C, Toader M, Stoica A, Pop G, Oprea A, Constantin AS, Niculescu L, Vivisenco IC, Drăghici MS, Osman A, Mogoantă CA (2016) Tonsillar lymphoma masquerading as obstructive sleep apnea - pediatric case report. Rom J Morphol Embryol 57(2 Suppl):885–891
Strongman H, Brown A, Smeeth L, Bhaskaran K (2019) Body mass index and Hodgkin’s lymphoma: UK population-based cohort study of 5.8 million individuals. Br J Cancer 120(7):768–770. https://doi.org/10.1038/s41416-019-0401-1
Coiffier B, Lepage E, Briere J, Herbrecht R, Tilly H, Bouabdallah R, Morel P, Van Den Neste E, Salles G, Gaulard P, Reyes F, Lederlin P, Gisselbrecht C (2002) CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med 346:235–242. https://doi.org/10.1056/NEJMoa011795
Li S, Young KH, Medeiros LJ (2018) Diffuse large B-cell lymphoma. Pathology 50:74–87. https://doi.org/10.1016/j.pathol.2017.09.006
Wang ML, Rule S, Martin P, Goy A, Auer R, Kahl BS, Jurczak W, Advani RH, Romaguera JE, Williams ME, Barrientos JC, Chmielowska E, Radford J, Stilgenbauer S, Dreyling M, Jedrzejczak WW, Johnson P, Spurgeon SE, Li L, Zhang L, Newberry K, Ou Z, Cheng N, Fang B, McGreivy J, Clow F, Buggy JJ, Chang BY, Beaupre DM, Kunkel LA, Blum KA (2013) Targeting BTK with ibrutinib in relapsed or refractory mantle-cell lymphoma. N Engl J Med 369:507–516. https://doi.org/10.1056/NEJMoa1306220
Stone CR, Mickle AT, Boyne DJ, Mohamed A, Rabi DM, Brenner DR, Friedenreich CM (2019) Treatment for lymphoma and late cardiovascular disease risk: a systematic review and meta-analysis. Health Sci Rep 2:e135. https://doi.org/10.1002/hsr2.135
Cui X, Zhu H, Huang J (2020) Nomogram for predicting lymph node involvement in triple-negative breast cancer. Front Oncol 10:608334. https://doi.org/10.3389/fonc.2020.608334
Song Z, Wang Y, Zhang D, Zhou Y (2020) A Novel tool to predict early death in uterine sarcoma patients: a surveillance, epidemiology, and end results-based study. Front Oncol 10:608548. https://doi.org/10.3389/fonc.2020.608548
Metzger ML, Mauz-Korholz C (2019) Epidemiology, outcome, targeted agents and immunotherapy in adolescent and young adult non-Hodgkin and Hodgkin lymphoma. Br J Haematol 185:1142–1157. https://doi.org/10.1111/bjh.15789
Thamm DH (2019) Novel treatments for lymphoma. Vet Clin North Am Small Anim Pract 49:903–915. https://doi.org/10.1016/j.cvsm.2019.04.004
Xu ML, Fedoriw Y (2016) Lymphoma microenvironment and immunotherapy. Surg Pathol Clin 9:93–100. https://doi.org/10.1016/j.path.2015.10.001
Acknowledgements
Thanks to all patients and authors who have con- tributed to the study.
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
YL: participated in the conception and design of this project, interpretation of data, and drafting. HZ: collected data and analysis. YW and ML: gave critical revision of the article and final approval of the manuscript to be submitted.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest. There are no financial conflicts of interest to disclose.
Ethical approval
All data from the SEER database are de-identified prior to publication to the public, so the cases extracted from the SEER database do not contain any personal identifying information and, therefore, no ethical approval is required for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liang, Y., Zhang, H., Wu, Y. et al. Incidence and survival trends in patients with primary tonsillar lymphoma: a large population-based study. Eur Arch Otorhinolaryngol 279, 4023–4032 (2022). https://doi.org/10.1007/s00405-022-07363-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07363-1