Abstract
Objective
To explore the correlation between the marital status and prognosis of patients with laryngeal squamous cell carcinoma (LSCC).
Study design
MPSM was adopted to minimize the maximum standardized average difference of the covariates among the four groups with different marital status.
Setting
Multinomial propensity scores matching (MPSM) based on data from the surveillance, epidemiology, and end results (SEER) database.
Methods
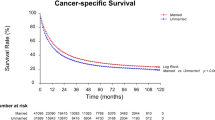
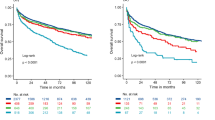
The Kaplan–Meier method and log-rank test were used to compare the survival outcomes of these groups with different marital status.
Results
Totally, 16,981 LSCC patients (median [IQR] age 62 [55–69] years; 829 [76.41%] males) from 2004 to 2016 were included in this study. Among them, 9112 (53.66%) were married, 2708 (15.95%) divorced or separated, 1709 (10.06%) widowed, and 3452 (20.33%) single. After MPSM, the weights make the characteristics of four groups with different marital status sufficient balance. The Kaplan–Meier method and log-rank test showed widowed patients may lead to the highest mortality rate while married patients have a higher survival rate than the other three groups. Single and divorced or separated patients had no significant difference in the survival rate. In addition, multivariate analysis by controlling for confounding factors showed that in male, well-differentiated, and early stage patients, compared with married, unmarried was an independent risk factor for CSS (P < 0.05).
Conclusion
Marital status showed a significant association with the survival status of LSCC patients. Importantly, the outcome of married patients was better, while widowed patients tended to have worse prognosis.



Similar content being viewed by others
References
Leoncini E, Vukovic V, Cadoni G et al (2018) Tumour stage and gender predict recurrence and second primary malignancies in head and neck cancer: a multicentre study within the INHANCE consortium. Eur J Epidemiol 33:1205–1218
Tamaki A, Miles BA, Lango M et al (2018) AHNS series: do you know your guidelines? Review of current knowledge on laryngeal cancer. Head Neck 40:170–181
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Gupta B, Johnson NW, Kumar N (2016) Global epidemiology of head and neck cancers: a continuing challenge. Oncology 91:13–23
Satoshi H, Tomoya Y, Yusuke O et al (2020) Chemoradiotherapy for high-risk stage II laryngeal cancer. Int J Clin Oncol 25:1596–1603
Fletcher KT, Gal TJ, Ebelhar AJ et al (2017) Prognostic indicators and survival in salvage surgery for laryngeal cancer. Head Neck 39:2021–2026
Zhu X, Heng Y, Zhou L et al (2019) A prognostic nomogram for predicting risk of recurrence in laryngeal squamous cell carcinoma patients after tumor resection to assist decision making for postoperative adjuvant treatment. J Surg Oncol 120:698–706
Boen CE, Barrow DA, Bensen JT et al (2018) Social relationships, inflammation, and cancer survival. Cancer Epidemiol Biomarkers Prev 27:541–549
McDonough MH, Jayne Beselt L, Daun JT et al (2019) The role of social support in physical activity for cancer survivors: a systematic review. Psychooncology 28:1945–1958
Uchino BN, Trettevik R, Kent de Grey RG et al (2018) Social support, social integration, and inflammatory cytokines: a meta-analysis. Health Psychol 37:462
Wang X, Cao W, Zheng C et al (2018) Marital status and survival in patients with rectal cancer: an analysis of the surveillance, epidemiology and end results (SEER) database. Cancer Epidemiol 54:119–124
Chen Z, Yin K, Zheng D et al (2020) Marital status independently predicts non-small cell lung cancer survival: a propensity-adjusted SEER database analysis. J Cancer Res Clin Oncol 146:67–74
Parise C, Caggiano V (2018) The influence of marital status and race/ethnicity on risk of mortality for triple negative breast cancer. PLoS ONE 13:e0196134
Qiu M, Yang D, Xu R (2016) Impact of marital status on survival of gastric adenocarcinoma patients: results from the surveillance epidemiology and end results (SEER) database. Sci Rep 6:1–10
Osazuwa-Peters N, Christopher KM, Cass LM et al (2019) What’s Love Got to do with it? Marital status and survival of head and neck cancer. Eur J Cancer Care 28:e13022
de Jonge P, Wardenaar KJ, Lim CCW et al (2018) The cross-national structure of mental disorders: results from the world mental health surveys. Psychol Med 48:2073
Joana P-T, Ainitze L, Eider P-S et al (2019) Predictors of psychological distress in breast cancer survivors: a biopsychosocial approach. Eur J Cancer Care (Engl) 28:e13166
Pike JL, Irwin MR (2006) Dissociation of inflammatory markers and natural killer cell activity in major depressive disorder. Brain Behav Immun 20:169–174
Antoni MH, Lutgendorf SK, Cole SW et al (2006) The influence of bio-behavioural factors on tumour biology: pathways and mechanisms. Nat Rev Cancer 6:240–248
Jaremka LM, Peng J, Bornstein R et al (2014) Cognitive problems among breast cancer survivors: loneliness enhances risk. Psychooncology 23:1356–1364
Kissane DW (2014) Unrecognised and untreated depression in cancer care. Lancet Psychiatry 1:320
Gonzales FA, Hurtado-de-Mendoza A, Santoyo-Olsson J et al (2016) Do coping strategies mediate the effects of emotional support on emotional well-being among Spanish-speaking Latina breast cancer survivors? Psychooncology 25:1286–1292
Ehrlich KB, Miller GE, Scheide T et al (2016) Pre-transplant emotional support is associated with longer survival after allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 51:1594–1598
Peterson EB, Ostroff JS, DuHamel KN et al (2016) Impact of provider-patient communication on cancer screening adherence: a systematic review. Prev Med 93:96–105
Shroff RT, Kennedy EB, Bachini M et al (2019) Adjuvant therapy for resected biliary tract cancer: ASCO clinical practice guideline. J Clin Oncol 37:1015–1027
Reyngold M, Winter KA, Regine WF et al (2020) Marital status and overall survival in patients with resectable pancreatic cancer: results of an ancillary analysis of NRG oncology/RTOG 9704. Oncologist 25:e477–e483
Samawi HH, Yin Y, Speers CH et al (2018) Sex disparities in outcomes of early stage colorectal cancer: a population-based study. Clin Colorectal Cancer 17:e711–e717
McLaughlin John M, Fisher James L, Paskett Electra D (2011) Marital status and stage at diagnosis of cutaneous melanoma: results from the surveillance epidemiology and end results (SEER) program, 1973–2006. Cancer 117:1984–1993
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
XD: interpretation, drafting, critical revision, and data interpretation; WZ: interpretation and acquisition of data, approval, and accountable; XL: analysis and interpretation of data; SY: data interpretation and critical revision; QC: data interpretation and critical revision; JH: data interpretation; YC: review and revision of the manuscript; JL: conception and design, approval, and accountable; all the authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Patient consent for publication
Not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Du, X., Zhan, W., Li, X. et al. Marital status and survival in laryngeal squamous cell carcinoma patients: a multinomial propensity scores matched study. Eur Arch Otorhinolaryngol 279, 3005–3011 (2022). https://doi.org/10.1007/s00405-022-07252-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07252-7