Abstract
Objectives
To determine the usefulness of the smoothed cepstral peak prominence (CPPS) in sustained vowel as objective measure of dysphonia.
Study design
This is a retrospective cohort study. 49 patients presenting a vocal cord motility impairment between 2012 and 2018 were included.
Methods
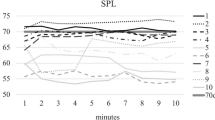
Classical acoustic parameters, including jitter, shimmer and NHR, as well as the CPPS were obtained for each patient with a vocal cord motility impairment confirmed by means of a fiberoptic laryngoscopy. We calculated the S/E ratio of each patient to establish the glottal efficiency. An independent sample t test and a Pearson correlation test were used to compare data.
Results
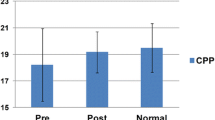
Patients presenting a vocal cord motility impairment present abnormal values of the CPPS. Those patients presenting a vocal cord paralysis present lower values of those presenting a vocal cord paresis, with statistically significant difference (P < 0.005). CPPS and the S/E ratio present a moderate negative correlation (− 0.29).
Conclusions
Subjects with a vocal cord motility impairment present abnormal values for CPPS and those values are lower, the greater the motility impairment is. Therefore, CPPS presents as an objective, measurable and reproducible acoustic parameter of dysphonia that will improve the evaluation of patients presenting vocal pathologies.


Similar content being viewed by others
References
Maryn Y, Roy N, De Bodt M, Van Cauwenberge P, Corthals P (2009) Acoustic measurement of overall voice quality: a meta-analysis. J Acoust Soc Am 126:2619–2634
Yumoto E, Gould WJ, Baer T (1982) Harmonics-to-noise ratio as an index of the degree of hoarseness. J Acoust Soc Am 71(6):1544–1549
Kreiman J, Gerratt BR (2000) Measuring vocal quality. In: Kent RD, Ball MJ (eds) Voice quality measurement. Singular Publishing Group, San Diego, pp 73–101
Maryn Y, Roy N, De Bodt M, Van Cauwenberge P, Corthals P (2009) Acoustic measurement of overall voice quality: a meta-analysis. J Acoust Soc Am 126(5):2619–2634. https://doi.org/10.1121/1.3224706
Maryn Y, Weenink D (2015) Objective dysphonia measures in the program Praat: smoothed cepstral peak prominence and acoustic voice quality index. J Voice 29(1):35–43. https://doi.org/10.1016/j.jvoice.2014.06.015
Núñez-Batalla F, Cartón-Corona N, Vasile G, García-Cabo P, Fernández-Vañes L, Llorente-Pendás JL (2019) Validation of the measures of cepstral peak prominence as a measure of dysphonia severity in Spanish-speaking subjects. Acta Otorrinolaringol Esp 70(4):222–228. https://doi.org/10.1016/j.otorri.2018.04.008
Sauder C, Bretl M, Eadie T (2017) Predicting voice disorder status from smoothed measures of cepstral peak prominence using Praat and analysis of dysphonia in speech and voice (ADSV). J Voice 31(5):557–566. https://doi.org/10.1016/j.jvoice.2017.01.006
Desuter G, Dedry M, Schaar B, van Lith-Bijl J, van Benthem PP, Sjögren EV (2018) Voice outcome indicators for unilateral vocal fold paralysis surgery: a review of the literature. Eur Arch Otorhinolaryngol 275(2):459–468. https://doi.org/10.1007/s00405-017-4844-9
Balasubramanium RK, Bhat JS, Fahim S, Raju R (2011) Cepstral analysis of voice in unilateral adductor vocal fold palsy. J Voice 25(3):326–329. https://doi.org/10.1016/j.jvoice.2009.12.010
Sprecher A, Olszewski A, Jiang JJ, Zhang Y (2010) Updating signal typing in voice: addition of type 4 signals. J Acoust Soc Am 127(6):3710–3716. https://doi.org/10.1121/1.3397477
http://www.fon.hum.uva.nl/praat/manual/Voice_3__Shimmer.html
Delgado-Hernández J, León-Gómez NM, Izquierdo-Arteaga LM, Llanos-Fumero Y (2018) Cepstral analysis of normal and pathological voice in Spanish adults. Smoothed cepstral peak prominence in sustained vowels versus connected speech. Acta Otorrinolaringol Esp. 69(3):134–140. https://doi.org/10.1016/j.otorri.2017.05.006
Brinca LF, Batista APF, Tavares AI, Goncalves IC, Moreno ML (2014) Useof cepstral analyses for differentiating normal from dysphonicvoices: a comparative study of connected speech versus sus-tained vowel in European Portuguese female speakers. J Voice 28:282–286
Dejonckere PH, Bradley P, Clemente P, Cornut G, Crevier-Buchman L, Friedrich G et al (2001) A basic protocol for functional assessment of voice pathology, especially for investigating the efficacy of (phonosurgical) treatments and evaluating new assessment techniques, Guideline elaborated by the Committee on Phoniatrics of the European Laryngological Society (ELS). Eur Arch Otorhinolaryngol. 258(2):77–82
Dejonckere PH (2000) Assessing efficacy of voice treatments: a guideline. Rev Laryngol Otol Rhinol (Bord) 121(5):307–310
Lopes LW, Sousa ESDS, Silva ACFD, Silva IMD, Paiva MAA, Vieira VJD et al (2019) Cepstral measures in the assessment of severity of voice disorders. Codas 31(4):e20180175. https://doi.org/10.1590/2317-1782/20182018175
Esen Aydinli F, Özcebe E, İncebay Ö (2019) Use of cepstral analysis for differentiating dysphonic from normal voices in children. Int J Pediatr Otorhinolaryngol 116:107–113. https://doi.org/10.1016/j.ijporl.2018.10.029
Brinca LF, Batista AP, Tavares AI, Gonçalves IC, Moreno ML (2014) Use of cepstral analyses for differentiating normal from dysphonic voices: a comparative study of connected speech versus sustained vowel in European Portuguese female speakers. J Voice 28(3):282–286. https://doi.org/10.1016/j.jvoice.2013.10.001
Lowell SY, Colton RH, Kelley RT, Mizia SA (2013) Predictive value and discriminant capacity of cepstral- and spectral-based measures during continuous speech. J Voice 27(4):393–400. https://doi.org/10.1016/j.jvoice.2013.02.005
Patel RR, Awan SN, Barkmeier-Kraemer J, Courey M, Deliyski D, Eadie T et al (2018) Recommended protocols for instrumental assessment of voice: American speech-language-hearing association expert panel to develop a protocol for instrumental assessment of vocal function. Am J Speech Lang Pathol 27(3):887–905. https://doi.org/10.1044/2018_AJSLP-17-0009
Acknowledgements
The authors present no conflict of interest and they do not have to disclosure any financial supporting.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Delgado-Vargas, B., Acle-Cervera, L., Sánz-López, L. et al. Cepstral analysis in patients with a vocal fold motility impairment: advantages of the cepstrum over time-based acoustic analysis. Eur Arch Otorhinolaryngol 278, 173–179 (2021). https://doi.org/10.1007/s00405-020-06291-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06291-2