Abstract
Purpose
The aim of this meta-analysis is to assess the correlation between blood transfusions and the medical/surgical complications after head and neck reconstructive surgery.
Methods
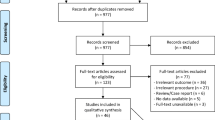
The PRISMA protocol was used and the literature search was performed on Pubmed, Scopus, Cochrane Library and Web of Science up to March 13, 2020. The risk of bias in individual studies was assessed through the Newcastle Ottawa Scale.
Results
A total of 1219 records were screened after the electronic search, 22 of which were included in the qualitative analysis. Of there 22 scores, 18 articles were included in the meta-analysis. The OR for medical and surgical complications of transfused patients was 1,64 (95% CI 1.23–2.21); while, the OR for hospital readmission was 1.53 (95% CI 1.29–1.81).
Conclusions
The results of this meta-analysis suggested that blood transfusions are associated with both an increased risk of surgical and medical complications of head and neck flaps and with the hospital readmission.


Similar content being viewed by others
References
Rosenthal E, Carroll W, Dobbs M, Magnoson S, Wax M, Peters G (2004) Simplifying head and neck microvascular reconstruction. Head Neck 26(11):930–936
Jones NF, Jarrahy R, Song JI, Kaufman MR, Markowitz B (2007) Postoperative medical complications—not microsurgical complications—negatively influence the morbidity, mortality, and true costs after microsurgical reconstruction for head and neck cancer. Plast Reconstruct Surg 119:2053–2060
Abouyared M, Katz AP, Ein L, Ketner J, Sargi Z, Nicolli E, Leibowitz JM (2019) Controversies in free tissue transfer for head and neck cancer: a review of the literature. Head Neck 41(9):3457–3463. https://doi.org/10.1002/hed.25853
Hill GE, Frawley WH, Griffith KE, Forestner JE, Minei JP (2003) Allogenic blood transfusion increases the risk of postoperative bacterial infection: a meta-analysis. J Trauma 54:908–914
Puram SV, Yarlagadda BB, Sethi R, Muralidhar V, Chambers KJ, Emerick KS, Rocco JW, Lin DT, Deschler DG (2015) Transfusion in head and neck free flap patients: practice patterns and a comparative analysis by flap type. Otolaryngol Head Neck Surg 152(3):449–457. https://doi.org/10.1177/0194599814567107
Liumbruno G, Bennardello F, Lattanzio A, Piccoli P, Rossetti G (2009) Reccomendations or the transfusion of red blood cells. Blood Transfus 7:49–64
Messmer K, Lewis DH, Sunder-Plassmann L, Klovekorn WP, Mendler N, Holper K (1972) Acute normovolemic hemodiluition. Changes of central hemodynamics and microcirculatory flow in skeletal muscle. Eur Surg Res 4(1):55–70
Rossmiller SR, Cannady SB, Ghanem TA, Wax MK (2010) Transfusion criteria in free flap surgery. Otolaryngol Head Neck Surg 142(3):359–364. https://doi.org/10.1016/j.otohns.2009.11.024
Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, Elbourne D, Egger M, Altman DG (2012) CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. Int J Surg 10(1):28–55
Cloke DJ, Green JE, Khan AL, Hodgkinson PD, McLean NR (2004) Factors influencing the development of wound infection following free-flap reconstruction for intra-oral cancer. Br J Plast Surg 57(6):556–560. https://doi.org/10.1016/j.bjps.2004.04.006
Karakida K, Aoki T, Ota Y, Yamazaki H, Otsuru M, Takahashi M, Sakamoto H, Miyasaka M (2010) Analysis of risk factors for surgical-site infections in 276 oral cancer surgeries with microvascular free-flap reconstructions at a single university hospital. J Infect Chemother 16(5):334–339. https://doi.org/10.1007/s10156-010-0108-y
Pinto FR, Malena CR, Vanni CM, Capelli Fde A, Matos LL, Kanda JL (2010) Pectoralis major myocutaneous flaps for head and neck reconstruction: factors influencing occurrences of complications and the final outcome. Sao Paulo Med J 128(6):336–341. https://doi.org/10.1590/s1516-31802010000600005
Lee DH, Kim SY, Nam SY, Choi SH, Choi JW, Roh JL (2011) Risk factors of surgical site infection in patients undergoing major oncological surgery for head and neck cancer. Oral Oncol 47(6):528–531. https://doi.org/10.1016/j.oraloncology.2011.04.002
Lin WJ, Wang CP, Wang CC, Jiang RS, Wong YK, Chen FJ, Liu SA (2012) The association between surgical site infection and previous operation in oral cavity cancer patients. Eur Arch Otorhinolaryngol 269(3):989–997. https://doi.org/10.1007/s00405-011-1709-5
McMahon JD, MacIver C, Smith M, Stathopoulos P, Wales C, McNulty R, Handley TP, Devine JC (2013) Postoperative complications after major head and neck surgery with free flap repair—prevalence, patterns, and determinants: a prospective cohort study. BrJ Oral Maxillofac Surg 51(8):689–695. https://doi.org/10.1016/j.bjoms.2013.04.015
Danan D, Smolkin ME, Varhegyi NE, Bakos SR, Jameson MJ, Shonka DC Jr (2015) Impact of blood transfusions on patients with head and neck cancer undergoing free tissue transfer. Laryngoscope 125(1):86–91. https://doi.org/10.1002/lary.24847
Hand WR, McSwain JR, McEvoy MD, Wolf B, Algendy AA, Parks MD, Murray JL, Reeves ST (2015) Characteristics and intraoperative treatments associated with head and neck free tissue transfer complications and failures. Otolaryngol Head Neck Surg 152(3):480–487. https://doi.org/10.1177/0194599814564366
Wang CH, Wong YK, Wang CP, Wang CC, Jiang RS, Lai CS, Liu SA (2015) Risk factors of recipient site infection in head and neck cancer patients undergoing pectoralis major myocutaneous flap reconstruction. Eur Arch Otorhinolaryngol 272(11):3475–3482. https://doi.org/10.1007/s00405-014-3372-0
Wong AK, Nguyen TJ, Peric M, Shahabi A, Vidar EN, Hwang BH, Leilabadi SN, Chan LS, Urata MM (2015) Analysis of risk factors associated with microvascular free flap failure using a multi-institutional database. Microsurgery 35(1):6–12. https://doi.org/10.1002/micr.22223
Ishimaru M, Ono S, Suzuki S, Matsui H, Fushimi K, Yasunaga H (2016) Risk factors for free flap failure in 2846 patients with head and neck cancer: a national database study in Japan. J Oral Maxillofac Surg 74(6):1265–1270. https://doi.org/10.1016/j.joms.2016.01.009
Sanati-Mehrizy P, Massenburg BB, Rozehnal JM, Ingargiola MJ, Hernandez Rosa J, Taub PJ (2016) Risk factors leading to free flap failure: analysis from the national surgical quality improvement program database. J Craniofac Surg 27(8):1956–1964. https://doi.org/10.1097/scs.0000000000003026
Carniol ET, Marchiano E, Brady JS, Merchant AM, Eloy JA, Baredes S, Park RC (2017) Head and neck microvascular free flap reconstruction: an analysis of unplanned readmissions. Laryngoscope 127(2):325–330. https://doi.org/10.1002/lary.26039
Garg RK, Wieland AM, Hartig GK, Poore SO (2017) Risk factors for unplanned readmission following head and neck microvascular reconstruction: results from the national surgical quality improvement program, 2011–2014. Microsurgery 37(6):502–508. https://doi.org/10.1002/micr.30116
Abt NB, Puram SV, Sinha S, Sethi RKV, Goyal N, Emerick KS, Lin DT, Deschler DG (2018) Transfusion in head and neck cancer patients undergoing pedicled flap reconstruction. Laryngoscope 128(12):E409–e415. https://doi.org/10.1002/lary.27393
Farquhar DR, Masood MM, Pappa AK, Patel SN, Hackman TG (2018) Predictors of adverse outcomes in free flap reconstruction: a single-institution experience. Otolaryngol Head Neck Surg 159(6):973–980. https://doi.org/10.1177/0194599818787801
Nguyen A, Shin H, Saint-Cyr M, Verheyden C (2018) Blood loss and transfusion rates in microsurgical head and neck reconstruction. Plast Reconstruct Surg 6(11):e1988. https://doi.org/10.1097/gox.0000000000001988
Wu H, Liu F, Ji F, Guo M, Wang Y, Cao M (2018) Identification of independent risk factors for complications: a retrospective analysis of 163 fibular free flaps for Mandibulofacial reconstruction. J Oral Maxillofac Surg 76(7):1571–1577. https://doi.org/10.1016/j.joms.2017.12.026
Goel AN, Raghavan G, St John MA, Long JL (2019) Risk factors, causes, and costs of hospital readmission after head and neck cancer surgery reconstruction. JAMA Facial Plast Surg 21(2):137–145. https://doi.org/10.1001/jamafacial.2018.1197
Grill FD, Wasmaier M, Mucke T, Ritschl LM, Wolff KD, Schneider G, Loeffelbein DJ, Kadera V (2020) Identifying perioperative volume-related risk factors in head and neck surgeries with free flap reconstructions—an investigation with focus on the influence of red blood cell concentrates and noradrenaline use. J Cranio Maxillofac Surg 48(1):67–74. https://doi.org/10.1016/j.jcms.2019.12.001
Wang C, Fu G, Ji F, Cheng S, Liu Z, Cao M (2020) Perioperative risk factors for radial forearm-free flap complications. J Craniofac Surg 31(2):381–384. https://doi.org/10.1097/scs.0000000000006035
Wang C, Fu G, Liu F, Liu L, Cao M (2018) Perioperative risk factors that predict complications of radial forearm free flaps in oral and maxillofacial reconstruction. Br J Oral Maxillofac Surg 56(6):514–519. https://doi.org/10.1016/j.bjoms.2018.04.015
Hanasono MM, Friel MT, Klem C, Hsu PW, Robb GL, Weber RS, Roberts DB, Chang DW (2009) Impact of reconstrustive microsurgery in patients with advanced oral cavity cancers. Head Neck 31:1289–1296
Perisanidis C, Herberger B, Papadogeorgakis N, Seemann R, Eder-Czembirek C, Tamandl D, Heinze G, Kyzas PA, Kanatas A, Mitchell D, Wolff KD, Ewers R (2012) Complications after free flap surgery: do we need a standardized classification of surgical complications? British J Oral Maxillofac Surg 50(2):113–118. https://doi.org/10.1016/j.bjoms.2011.01.013
Opelz G, Sengar DP, Mickey MR, RTerasaki PI, (1973) Effect of blood transfusions on subsequent kidney transplants. Transplant Proc 5:253–259
Girod A, Brancati A, Mosseri V, Kriegel I, Jouffroy T, Rodriguez J (2010) Study of the length of hospital stay for free flap reconstruction of oral and pharyngeal cancer in the context of the new French casemix-based funding. Oral Oncol 46(3):190–194. https://doi.org/10.1016/j.oraloncology.2009.12.002
Offodile AC 2nd, Aherrera A, Guo L (2014) Risk factors associated with prolonged postoperative stay following free tissue transfer: an analysis of 2425 patients from the American College of Surgeons National Surgical Quality Improvement Program database. Plast Reconstruct Surg 134(6):1323–1332. https://doi.org/10.1097/prs.0000000000000735
Eskander A, Kang SY, Tweel B, Sitapara J, Old M, Ozer E, Agrawal A, Carrau R, Rocco J, Teknos TN (2018) Quality indicators: measurement and predictors in head and neck cancer free flap patients. Otolaryngol Head Neck Surg 158(2):265–272. https://doi.org/10.1177/0194599817742373
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest.
Research involving human participants and/or animals
This research didn’t include any human participants and/or animals.
Informed consent
Not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Giovacchini, F., Bensi, C., Paradiso, D. et al. Association between blood transfusions and complications in head and neck reconstruction: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol 278, 2171–2185 (2021). https://doi.org/10.1007/s00405-020-06286-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06286-z