Abstract
Purpose
The authors aim to review available reports regarding laryngeal candidiasis and describe the existing evidence on the demographics, clinical manifestations, diagnosis, therapeutic options, and outcomes of this infection.
Methods
A review of articles on laryngeal candidiasis was conducted using PubMed® database from its inception through July 2019.
Results
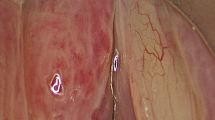
Patients were mainly females presenting with complaints of dysphonia and associated gastroesophageal reflux history or inhaled corticosteroids use; although local predisposing factors were common, most patients were immunocompetent. The main anatomical affected subsite was the glottis with the presence of leukoplastic lesions. The diagnostic approach remains controversial, since some authors recommend prompt lesion biopsy and others rely on empirical antifungal treatment that showed effective results regarding symptoms and lesions resolution.
Conclusion
Laryngeal Candida infection is thought to be a rare condition, with limited available literature. The correct diagnosis is difficult for the otolaryngologist and a high level of suspicion is required. The authors emphasize the need to include this condition into the differential diagnosis in patients with predisposing factors presenting with suspected lesions. In addition, the conservative diagnostic approach with antifungal treatment seems to provide effective outcomes, although comparative clinical studies between diagnostic options are lacking.
Similar content being viewed by others
References
Mehanna HM, Kuo T, Chaplin J, Taylor G, Morton RP (2004) Fungal laryngitis in immunocompetent patients. J Laryngol Otol 118(5):379–381. https://doi.org/10.1258/002221504323086615
Nunes FP, Bishop T, Prasad ML, Madison JM, Kim DY (2008) Laryngeal candidiasis mimicking malignancy. Laryngoscope 118(11):1957–1959. https://doi.org/10.1097/MLG.0b013e3181802122
Nair AB, Chaturvedi J, Venkatasubbareddy MB, Correa M, Rajan N, Sawkar A (2011) A case of isolated laryngeal candidiasis mimicking laryngeal carcinoma in an immunocompetent individual. Malays J Med Sci 18(3):75–78
Ravikumar A, Prasanna Kumar S, Somu L, Sudhir B (2014) Fungal laryngitis in immunocompetent patients. Indian J Otolaryngol Head Neck Surg 66(Suppl 1):375–378. https://doi.org/10.1007/s12070-011-0322-7
Balsam D, Sorrano D, Barax C (1992) Candida epiglottitis presenting as stridor in a child with HIV infection. Pediatr Radiol 22(3):235–236
Andrade DT, Correa D, León MN, Napolitano VC, Badia P (2016) Laringitis fúngica en pacientes inmunocompetentes. Revista de otorrinolaringología y cirugía de cabeza y cuello 76:7–14. https://doi.org/10.4067/S0718-48162016000100002
Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA, Ostrosky-Zeichner L, Reboli AC, Schuster MG, Vazquez JA, Walsh TJ, Zaoutis TE, Sobel JD (2016) Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis 62(4):e1–50. https://doi.org/10.1093/cid/civ933
Zhang S, Farmer TL, Frable MA, Powers CN (2000) Adult herpetic laryngitis with concurrent candidal infection: a case report and literature review. Arch Otolaryngol Head Neck Surg 126(5):672–674
Henry LR, Packer MD, Brennan J (2005) Airway-obstructing laryngeal candidiasis in an immunocompetent host. Otolaryngol Head Neck Surg 133(5):808–810. https://doi.org/10.1016/j.otohns.2004.10.017
Haberman RS 2nd, Becker ME, Ford CN (1983) Candida epiglottitis. Arch Otolaryngol 109(11):770–771. https://doi.org/10.1001/archotol.1983.00800250064015
Cole S, Zawin M, Lundberg B, Hoffman J, Bailey L, Ernstoff MS (1987) Candida epiglottitis in an adult with acute nonlymphocytic leukemia. Am J Med 82(3 Spec No):662–664. https://doi.org/10.1016/0002-9343(87),90119-7
Walsh TJ, Gray WC (1987) Candida epiglottitis in immunocompromised patients. Chest 91(4):482–485. https://doi.org/10.1378/chest.91.4.482
Hirshoren N, Eliashar R, Weinberger JM (2008) Candida epiglottitis: a rare emergent condition—appearance, treatment and pitfalls. Eur J Intern Med 19(8):e84–85. https://doi.org/10.1016/j.ejim.2008.04.010
Kobayashi RH, Rosenblatt HM, Carney JM, Byrne WJ, Ament ME, Mendoza GR, Dudley JP, Stiehm ER (1980) Candida esophagitis and laryngitis in chronic mucocutaneous candidiasis. Pediatrics 66(3):380–384
Guclu O, Ulkumen B, Bulbul T (2006) Candida laryngitis. Otolaryngol Head Neck Surg 135(3):483–484. https://doi.org/10.1016/j.otohns.2006.02.023
Forrest LA, Weed H (1998) Candida laryngitis appearing as leukoplakia and GERD. J Voice 12(1):91–95
Yonkers AJ (1973) Candidiasis of the larynx. Ann Otol Rhinol Laryngol 82(6):812–815. https://doi.org/10.1177/000348947308200611
Lawson R, Bodey G, Luna M (1980) Case report: candida infection presenting as laryngitis. Am J Med Sci 280(3):173–177
Williams AJ, Baghat MS, Stableforth DE, Cayton RM, Shenoi PM, Skinner C (1983) Dysphonia caused by inhaled steroids: recognition of a characteristic laryngeal abnormality. Thorax 38(11):813–821
Makitie AA, Back L, Aaltonen LM, Leivo I, Valtonen M (2003) Fungal infection of the epiglottis simulating a clinical malignancy. Arch Otolaryngol Head Neck Surg 129(1):124–126
Hass A, Hyatt AC, Kattan M, Weiner MA, Hodes DS (1987) Hoarseness in immunocompromised children: association with invasive fungal infection. J Pediatr 111(5):731–733. https://doi.org/10.1016/s0022-3476(87)80254-8
Al-Kindi H, Abdoon H, Alkhabori M, Daar S, Beshlawi I, Wali YA (2008) Invasive candidal laryngitis as a manifestation of cyclic neutropenia in an Omani infant. Pediatr Hematol Oncol 25(4):339–344. https://doi.org/10.1080/08880010802016144
Hollis LJ, Montgomery PQ, Hern JD, Mahadeva U, Tolley NS (1996) Invasive candidiasis of a late presentation laryngeal chondroradionecrosis. J Laryngol Otol 110(8):789–792
Ganesan S, Harar RP, Dawkins RS, Prior AJ (1998) Invasive laryngeal candidiasis: a cause of stridor in the previously irradiated patient. J Laryngol Otol 112(6):575–578
Selkin SG (1985) Laryngeal candidiasis and ketoconazole. Otolaryngol Head Neck Surg 93(5):661–663. https://doi.org/10.1177/019459988509300516
Wong KK, Pace-Asciak P, Wu B, Morrison MD (2009) Laryngeal candidiasis in the outpatient setting. J Otolaryngol Head Neck Surg 38(6):624–627
Jacobs RF, Yasuda K, Smith AL, Benjamin DR (1982) Laryngeal candidiasis presenting as inspiratory stridor. Pediatrics 69(2):234–236
Tashjian LS, Peacock JE Jr (1984) Laryngeal candidiasis. Report of seven cases and review of the literature. Arch Otolaryngol 110(12):806–809
Fisher EW, Richards A, Anderson G, Albert DM (1992) Laryngeal candidiasis: a cause of airway obstruction in the immunocompromised child. J Laryngol Otol 106(2):168–170
Tedeschi LG, Cheren RV (1968) Laryngeal hyperkeratosis due to primary monilial infection. Arch Otolaryngol 87(1):82–84. https://doi.org/10.1001/archotol.1968.00760060084016
Perrone JA (1970) Laryngeal obstruction due to monilia albicans in a newborn. Laryngoscope 80(2):288–291. https://doi.org/10.1288/00005537-197002000-00013
Sulica L (2005) Laryngeal thrush. Ann Otol Rhinol Laryngol 114(5):369–375. https://doi.org/10.1177/000348940511400506
Lees JJ (1959) Moniliasis of the larynx and hypopharynx. J Laryngol Otol 73:619–620. https://doi.org/10.1017/s0022215100055791
Medoff G, Dismukes WE, Meade RH 3rd, Moses JM (1972) A new therapeutic approach to candida infections. A preliminary report. Arch Intern Med 130(2):241–245
Lee DH, Cho HH (2013) Primary candidiasis and squamous cell carcinoma of the larynx: report of a case. Surg Today 43(2):203–205. https://doi.org/10.1007/s00595-012-0231-8
Hicks JN, Peters GE (1982) Pseudocarcinomatous hyperplasia of the larynx due to candida albicans. Laryngoscope 92(6 Pt 1):644–647
DelGaudio JM (2002) Steroid inhaler laryngitis: dysphonia caused by inhaled fluticasone therapy. Arch Otolaryngol Head Neck Surg 128(6):677–681
Laing RB, Wardrop PJ, Welsby PD, Brettle RP (1995) Stridor in patients with HIV infection. J Laryngol Otol 109(12):1197–1199
Lepak A, Andes D (2011) Fungal sepsis: optimizing antifungal therapy in the critical care setting. Crit Care Clin 27(1):123–147. https://doi.org/10.1016/j.ccc.2010.11.001
Baum GL (1960) The significance of candida albicans in human sputum. N Engl J Med 263:70–73. https://doi.org/10.1056/nejm196007142630204
Stachler RJ, Francis DO, Schwartz SR, Damask CC, Digoy GP, Krouse HJ, Mccoy SJ, Ouellette DR, Patel RR, Reavis CCW, Smith LJ, Smith M, Strode SW, Woo P, Nnacheta LC (2018) Clinical practice guideline: hoarseness (Dysphonia) (Update). Otolaryngol Head Neck Surg 158(1):S1–S42. https://doi.org/10.1177/0194599817751030
Vrabec DP (1993) Fungal infections of the larynx. Otolaryngol Clin North Am 26(6):1091–1114
Pabuccuoglu U, Tuncer C, Sengiz S (2002) Histopathology of candidal hyperplastic lesions of the larynx. Pathol Res Pract 198(10):675–678. https://doi.org/10.1078/0344-0338-00319
Takahashi Y, Nagata N, Shimbo T, Nishijima T, Watanabe K, Aoki T, Sekine K, Okubo H, Watanabe K, Sakurai T, Yokoi C, Kobayakawa M, Yazaki H, Teruya K, Gatanaga H, Kikuchi Y, Mine S, Igari T, Takahashi Y, Mimori A, Oka S, Akiyama J, Uemura N (2015) Long-term trends in esophageal candidiasis prevalence and associated risk factors with or without HIV infection: lessons from an endoscopic study of 80,219 patients. PLoS ONE 10(7):e0133589. https://doi.org/10.1371/journal.pone.0133589
Lipan MJ, Reidenberg JS, Laitman JT (2006) Anatomy of reflux: a growing health problem affecting structures of the head and neck. Anat Rec B New Anat 289(6):261–270. https://doi.org/10.1002/ar.b.20120
Yao A, Bates TJ, Pearson J, Robinson M, Ward C, Powell J (2018) Laryngeal candidiasis: our experience from sixty biopsy specimens. Clin Otolaryngol 43(2):729–732. https://doi.org/10.1111/coa.13034
Funding
None declared.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no competing interest.
Research involving human participants and/or animals
All the procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This is a review on retrospective studies which were conducted on already available data for which formal consent was obtained. Therefore, institutional ethical approval is not required according to the law and the national ethical guidelines.
Informed consent
Informed consent was not obtained from individual participants due the fact that this review included retrospective studies for which formal consent was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Valente, P., Ferreira, J., Pinto, I. et al. Management of laryngeal candidiasis: an evidence-based approach for the otolaryngologist. Eur Arch Otorhinolaryngol 277, 1267–1272 (2020). https://doi.org/10.1007/s00405-020-05865-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-05865-4