Abstract
Background
Fungal laryngitis is a fungal infection of the larynx which is an extremely rare clinical entity, especially in immunocompetent patients. The diagnosis is often overlooked and delayed among patients, and it is usually evident among immunocompromised patients.
Case presentation
We herein present a case of a 60-year-old gentleman presented with dysphagia for 6 months associated with hoarseness. Endoscopic examination shows a fungating mass over the larynx that mimics cancer. However, a biopsy of the mass showed the presence of fungal spores.
Conclusion
This case report emphasizes the importance of clinical suspicion of fungal laryngitis and its early intervention.
Similar content being viewed by others
Background
An isolated fungal infection of the larynx is less common than a fungal infection of the respiratory tract. Primary fungal laryngitis is also a very rare clinical entity.1 It often presents with nonspecific clinical symptoms and often gets confused with certain laryngeal diseases such as leukoplakia, gastroesophageal reflux disease, and other granulomatous lesions of the larynx not forgetting carcinoma [1]. The common presentation of fungal laryngitis varies and can present as hoarseness, dysphagia, dysphonia, odynophagia, stridor, and respiratory distress [2].
These nonspecific clinical presentations mimicking other laryngeal lesions may cause misdiagnosis which will lead to inappropriate treatment. Therefore, clinicians and otolaryngologists should take count of the presentation and diagnosis as treatment differs for fungal infections at uncommon sites like the larynx [3].
Case presentation
A 60-year-old man with underlying diabetes mellitus and bronchial asthma was referred for dysphagia and globus sensation over the throat for the past 5 months associated with hoarseness. Esophagogastroduodenoscopy (OGDS) performed primarily by the surgical team showed a fungating mass over the supraglottic region, partially obstructing the upper airway, and was referred to the ORL clinic for further management.
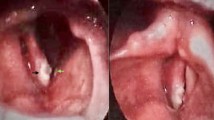
Upon review, the patient was not in respiratory distress, and no stridor was heard. There were no cervical lymph nodes palpable. Endoscopic examination of the pharynx and larynx showed a fungating mass at the right arytenoid extending anteriorly to posterior 1/3 of the right false cord with normal mobility of the vocal cords (Fig. 1). Other laryngeal subsites were normal. A biopsy of the mass was reported as a fungal spore with no malignant cells seen (Fig. 2). After discussing with our pathologist and multiple testings, it was concluded that the patient was suffering from fungal laryngitis rather than laryngeal cancer. The patient was then treated with oral antifungal (Fluconazole) for 3 months duration. He responded well to treatment and subsequent follow-up showed a resolved lesion (Fig. 3). Subsequently, the patient was called for a monthly follow-up to perform a surveillance endoscope, the scope findings were unremarkable.
Discussion
Fungal laryngitis is an infection which is commonly seen in immunocompromised individuals masquerading other laryngeal diseases with endoscopy and radiological appearance mimicking the features of laryngeal malignancy [2]. Early detection and treatment are crucial as misdiagnosis or delay in treatment may result in further impairment of the anatomical and functional properties of the larynx [3]. Even so, recent reports state that fungal laryngitis can happen in both immunocompromised patients and healthy patients with predisposing factors such as the use of corticosteroids especially inhaled steroids in asthmatics, broad-spectrum antibiotics usage, diabetes, alcoholism, burns, endotracheal intubations, and recent laryngitis [5]. A history of steroid usage regardless of inhaled or via oral are helpful diagnostic pointer [5]. Our patient had two risk factors namely diabetes and chronic usage of corticosteroid inhaler due to his uncontrolled bronchial asthma. It is known that a considerable proportion of inhaled corticosteroid is deposited in the larynx, especially on the superior surface of the vocal cord, easing fungal colonization on the epithelial surfaces [6].
Clinical presentation of fungal laryngitis is nonspecific and varies such as sore throat, hoarseness, dysphagia, even so respiratory distress, fever, cough, and/or Gerd-like symptoms are reported too [2, 7]. Clinician should keep in mind the risk factors that might be involved aided by a high-definition laryngoscopy that could change the diagnosis that he/she is looking for [4]. Nonetheless in our case, it is known that the scope finding results in a huge well-circumscribed tumor in the supraglottic region partially obstructing the airway, mimicking carcinoma as our primary diagnosis.
Histological evaluation of tissues is a quick and easy way to identify fungal organisms and as an adjunct to microbiologic culture for diagnosis of fungal infections. Histologic evaluation of granulomatous inflammation and granulomas must include special stains such as Gomori Methenamine Silver (GMS) and periodic acid-Schiff (PAS) to exclude or include the presence of fungi and acid-fast bacteria. The most common fungi causing laryngitis is Candida followed by Aspergillosis, Cryptococcal, Blastomycosis, and Histoplasmosis is also implicated. Infection is usually precipitated by pulmonary or oropharyngeal infection [3].
Therapy of fungal laryngitis consists of prolonged treatment by systemic antifungals. According to literature, a daily usage of fluconazole at a dose of 100 to 400 mg should be given as the main choice. It is the fundamental drug of choice for patients with candida infections, as this oral agent has a higher rate of absorption [7]. Duration of treatment can vary from 10 to 30 days with noticeable clinical changes [1, 7]. Our patient was started with 200 mg oral fluconazole daily for 30 days and showed dramatic improvement in 2 weeks. At the same time, patient was satisfied as his symptoms improved tremendously post-completion of treatment.
Conclusion
Fungal laryngitis should be considered in the differential diagnosis in any immunocompromised or immunocompetent patient with risk factors as stated above. Failure to do so may result in impairment of anatomical and functional properties of the larynx. Our case has demonstrated fungal laryngitis mimicking laryngeal malignancy. Therefore, performing a biopsy with histological examination using special stains is crucial and allows the exclusion of malignancy and prevents misdiagnosis along with mistreatment which will potentially harm the patient.
Patient perspective
The patient felt better after the completion of his treatment. He was thankful for choosing our center rather than any other medical center due to the wonderful hospitality and treatment choices offered to him. His family and himself were very satisfied with our mode of treatment as we did not cause any potential harm even though we had a diagnostic dilemma in the beginning.
Availability of data and materials
Not applicable.
References
Swain SK, Sahu MC, Debdta P, Baisakh MR (2019) Primary fungal laryngitis: an overlooked clinical entity. Apollo Med 16:11–15
Singh K, Chong AW, Mun KS (2016) Fungal laryngitis causing airway compromise in post irradiated patient. Acta Oto-Laryngologica Case Reports 1(1):123–125
Ravikumar A et al (2014) Fungal laryngitis in immunocompetent patients. Indian journal of otolaryngology and head and neck surgery: official publication of the Association of Otolaryngologists of India, vol. 66. Suppl 1:375–378. https://doi.org/10.1007/s12070-011-0322-7
Issa IJ (2018) Fungal Laryngitis in Immunocompetent Patients; Risk Factors, Presentation and Treatment. Sch J Otolaryngol 1(3). https://doi.org/10.32474/sjo.2018.01.000114
Sapre AP, Gosavi RS (2017) Fungal Laryngitis in Immunocompetent Individuals: Not so Uncommon. Int J Phonosurgery Laryngol 7(2):66–71. https://doi.org/10.5005/jp-journals-10023-1147
Saha A, Saha K, Chatterjee U (2015) Primary aspergillosis of vocal cord: Long-term inhalational steroid use can be the miscreant. Biomed J 38(6):550–553. https://doi.org/10.1016/j.bj.2015.09.001
Mesolella M, Maione N, Salerno G, Motta G (2021) Laryngeal candidiasis mimicking supraglottic carcinoma by prolonged inhaled steroid therapy: a case report and review of the literature. Ear, Nose and Throat Journal. 100(5):761S–765S
Acknowledgements
We would like to sincerely thank the patient for his full cooperation throughout the process of writing this case report.
Funding
None.
Author information
Authors and Affiliations
Contributions
KS: major contributor in writing the manuscript. VK: major contributor in writing the manuscript. FWAM: major contributor in editing. AMD: major contributor in editing. ASR: major contributor in editing. IM: major contributor in consultation. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethics approval from the National Medical Research Registry Board. Informed written consent to participate in the study was provided by all participants.
Consent for publication
Written consent has been taken from the individual involved in my study. The patient has consented to publish the case report and images via written consent. Written informed consent for publication of their clinical details and/or clinical images was obtained from the patient. A copy of the consent form is available for review by the Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Srinivasagam, K., Kumarasamy, V., Manab, F.W.A. et al. Fungal laryngitis: a forgotten disease mimicking laryngeal cancer—a case report. Egypt J Otolaryngol 39, 188 (2023). https://doi.org/10.1186/s43163-023-00537-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-023-00537-6