Abstract
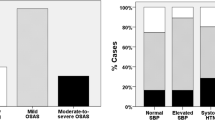
The grading system of the severity of obstructive sleep apnea hypopnea syndrome (OSAHS) used presently showed that the severe OSAHS had an extensive range of apnea hypopnea index (AHI) (≥30, even over 100). So this grading system is not rational. From Jan 1999 to June 2011, there were 2,618 patients complaining of snoring took the polysomnography. The patients were divided into 11 groups according to their AHI. Frequencies of OSAHS with hypertension in each group were tested using crosstabs. The incidence of hypertension was increased as the increasing of AHI. Crosstab analysis showed that there were four cutoff points of AHI (5, 30, 50, 100). There was a significant difference in the incidence of hypertension between the groups of AHI more than the cutoff point and AHI less than the cutoff point. So from the view of hypertension in each group, we recommend that the AHI <5 should be considered as normal or simple snorer, AHI = 5–30 as mild degree of OSAHS, AHI = 30–50 as moderate degree of OSAHS, AHI = 50–100 as severe degree of OSAHS, and AHI ≥100 as profound degree of OSAHS.

Similar content being viewed by others
References
Anonymous (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep 22:667–689
Nieto FJ, Young TB, Lind BK et al (2000) Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA 283(14):1829–1836
Young T, Finn L, Peppard PE, Szklo-Coxe M et al (2008) Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep 31(8):1071–1078
Kulkas A, Tiihonen P, Julkunen P et al (2013) Novel parameters indicate significant differences in severity of obstructive sleep apnea with patients having similar apnea-hypopnea index. Med Biol Eng Comput 51(6):697–708
Lavie P, Silverberg D, Oksenberg A et al (2001) Obstructive sleep apnea and hypertension: from correlative to causative relationship. J Clin Hypertens 3(5):296–301
Fusetti M, Fioretti AB, Valenti M et al (2012) Cardiovascular and metabolic comorbidities in patients with obstructive sleep apnoea syndrome. Acta Otorhinolaryngol Ital 32(5):320–325
Marin JM, Agusti A, Villar I et al (2012) Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA 307(20):2169–2176
Konecny T, Kara T, Somers VK (2014) Obstructive sleep apnea and hypertension: an update. Hypertension 63(2):203–209
Writing Group of 2010 Chinese Guidelines for the Management of Hypertension (2011) 2010 Chinese guidelines for the management of hypertension. Zhonghua Xin Xue Guan Bing Za Zhi 39(7):579–615
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, J., Chen, X. & Sun, J. Is the grading system of the severity of the OSAHS used presently rational or not?: from the view of incidence of hypertension in different severity groups. Eur Arch Otorhinolaryngol 271, 2561–2564 (2014). https://doi.org/10.1007/s00405-014-3036-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-014-3036-0