Abstract
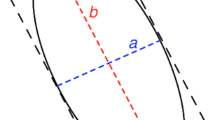
The use of trans-oral laser techniques for the resection of head and neck carcinomas has increased exponentially over the last four decades. Inadvertent laser damage to the patient or operating theatre staff is an acknowledged risk. However, no data exist to verify the safety margin of commonly employed precautions. The aims of this study was to assess the safety margins of protective strategies commonly adopted when using CO2 lasers to resect tumours of the head and neck. A Sigmacon Acupulse Lumenis™ CO2 laser was evaluated. The beam was focused to 2 mm diameter at 402 mm focal length. Gauze swabs, neurosurgical patties, surgical gloves, paper drapes and conventional endotracheal (ET) tubes were tested against the following laser variables: power, beam characteristics and angle of beam incidence (90 & 45°). Laser penetration time through the material under test was recorded in seconds (s). All the materials where tested dry and some, when appropriate, were tested wet. The mean of three recordings was calculated. The results demonstrated dry gauze swabs, neurosurgical patties and paper drapes provided 0 s protection at 2 W (lowest power). However, when wet, the laser failed to penetrate the swabs and neurosurgical patties, even after 180 s of continuous application. Gloves (single or double layer), and ET cuffs were penetrated in less than 1 s at 2 W. Time to penetrate a size 6.0 ET tube at 2 W continuous setting increased from <1 s at 90° to 42 s at 45°. These data are essential for anyone using CO2 lasers for the resection of head and neck tumours. The importance of keeping laser consumables wet throughout the procedure is highlighted. The angle at which the laser hits the ET tube may impart some protection against airway fire but the data support the need to cover the ET tube with damp swabs or neuropatties when possible.




Similar content being viewed by others
References
Ferguson J, Carr R, Chang E, Farrior E (2002) Evaluation of endotracheal tube safety for CO2 laser resurfacing. Laryngoscope 112:1239–1242
Strong MS, Jako GJ (1972) Laser surgery in the larynx. Ann Otol Rhinol Laryngol 81:791–798
Vaughan CW, Strong MS, Jako GJ et al (1978) Laryngeal carcinoma: transoral treatment utilizing the CO2 laser. Am J Surg 136(4):490–493
Strong MS, Vaughan CW, Healy GB et al (1979) Transoral management of localized carcinoma of the oral cavity using the CO2 laser. Laryngoscope 89(6):897–905
Burian K, Höfler H (1979) On micirosurgical treatment of vocal cord carcinomas with CO2 laser. Laryngol Rhinol Otol (Stuttg) 58:551–556
Davis RK, Shapshay SM, Strong MS, Hyams VJ (1983) Transoral partial supraglottic resection using the CO2 laser. Laryngoscope 93(4):429–432
Davis RK, Kelly SM, Hayes J (1991) Endoscopic CO2 laser excisional biopsy of early supraglottic cancer. Laryngoscope 101(6, pt 1):680–683
Motta G, Villari G, Motta GJ, Ripa G, Salerno G (1986) The CO2 laser in the laryngeal microsurgery. Acta Otolaryngol Suppl (Stockh) 433:1–30
Motta G, Esposito E, Cassiano B, Motta S (1997) T1-T2-T3 glottic tumors: fifteen years experience with CO2 laser. Acta Otolaryngol Suppl (Stockh) 527:155–159
Myers EN, Wagner RL, Johnson JT (1994) Microlaryngoscopic surgery for T1 glottic lesions: a cost-effective option. Ann Otol Rhinol Laryngol 103:28–30
Thumfart WF, Eckel HE (1990) Endolaryngeal laser surgery in the treatment of laryngeal cancers. The current cologne concept. HNO 38:174–178
Ambrosch P (2007) The role of laser microsurgery in the treatment of laryngeal cancer. Curr Opin Otolaryngol Head Neck Surg 15(2):82–88
Ossoff RH, Hotaling AJ, Karlan MS, Sisson GA (1983) CO2 laser in otolaryngology-head and neck surgery: a retrospective analysis of complications. Laryngoscope 93(10):1287–1289
Fader DJ, Ratner D (2000) Principles of CO2/erbium laser safety. Dermatol Surg 26(3):235–239
Kuo CH, Tan PH, Chen JJ et al (2001) Endotracheal tube fires during carbon dioxide laser surgery on the larynx—a case report. Acta Anaesthesiol Sin 39:53–56
Lai HC, Juang SE, Liu TJ et al (2002) Fires of endotracheal tubes of three different materials during carbon dioxide laser surgery. Acta Anaesthesiol Sin 40:47–51
Dhar V, Young K, Nouraei SA et al (2008) Impact of oxygen concentration and laser power on occurrence of intraluminal fires during shared-airway surgery: an investigation. J Laryngol Otol 122(12):1335–1338
Jaquet Y, Monnier P, Melle GV et al (2006) Complications of different ventilation strategies in endoscopic laryngeal surgery: a 10-year review. Anesthesiology 104:52–59
Rubiano R, Chang JL, Larson CE, Lawler RA, Rehkopf R (1985) Precautions in use of a new endotracheal tube for laser surgery. Anesth Analg 64:1037–1038
Schramm VL Jr, Mattox DE, Stool SE (1981) Acute management of laser-ignited intratracheal explosion. Laryngoscope 91:1417–1426
Yarington ET, Thomosone GE (1982) Incendiary characteristics of endotracheal tubes with the carbon dioxide laser. Ann Otol Rhinol Laryngol 91:605
Strong MS, Jacko GJ, Polanyi T et al (1973) Laser Surgery in the aerodigestive tract. Am J Surg 126:533
Ossoff RH (1989) Laser safety in otolaryngology-head and neck surgery: anaesthetic and educational considerations for laryngeal surgery. Laryngoscope 99(Suppl):1–26
Snow JC, Norton ML, Saluja TS, Estanislao AF (1976) Fire hazard during CO2 laser microsurgery on the larynx and trachea. Anesth Analg 55:146–147
Cozine K, Rosenbaum LM, Ashkanazi J, Rosenbaum SH (1981) Laser induced endotracheal fire. Anesthesiology 55:583–585
Sesterhenn AM, Dunne AA, Braulke D, Lippert BM, Benedikt JF, Werner JA (2003) Lasers in surgery and medicine 32:384–390
LeJeune FE, LeTard F, Guice C, Marice H (1982) Heat sink protection against lasering endotracheal cuffs. Ann Otol Rhinol Laryngol 91:606–607
Sosis MB, Dillon FX (1991) Saline-filled cuffs help prevent laser-induced polyvinylchloride endotracheal tube fires. Anaesth Analg 72:187–189
Sosis MB, Braverman B (1996) Advantage of rubber over plastic endotracheal tubes for rapid extubation in a laser fire. J Clin Laser Med Surg 14(2):93–95
Acknowledgements
The authors would like to thank Storz, Sigmacon and Carl Zeiss for their financial contributions, which allowed this study to be undertaken.
Author information
Authors and Affiliations
Corresponding author
Appendix 1: Time in seconds for laser penetration through various materials at varied laser settings
Appendix 1: Time in seconds for laser penetration through various materials at varied laser settings
See Table 1.
Rights and permissions
About this article
Cite this article
Ahmed, F., Kinshuck, A.J., Harrison, M. et al. Laser safety in head and neck cancer surgery. Eur Arch Otorhinolaryngol 267, 1779–1784 (2010). https://doi.org/10.1007/s00405-010-1312-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-010-1312-1