Abstract
Radiotherapy of the laryngopharynx sometimes leads to functional disabilities including swallowing dysfunction. One of the reasons for these disabilities is a deterioration of laryngeal sensation. Laryngeal sensation is an important factor in swallowing, but quantitative evaluation of laryngeal sensation has been difficult. In this study, we evaluated changes in laryngeal sensation before and after radiotherapy for laryngeal and hypopharyngeal cancer, using a flexible laryngoscope and probes. This study was conducted in 12 patients, 8 with laryngeal cancer and 4 with hypopharyngeal cancer, who received radiotherapy alone or chemoradiotherapy at our medical centre. Measurements were performed using a 3.3-mm-diameter flexible laryngoscope with a probe port and four types of probes with 0.06-, 0.13-, 0.20-, and 0.30-mm nylon filaments attached to a wire tip. Sensation was evaluated at the tip of the epiglottis and the arytenoid region. Measurements were performed before radiotherapy, 1, 3 months, and 1 year after completion of radiotherapy. Sensation of the epiglottis and arytenoid deteriorated significantly 1 and 3 months after radiotherapy compared with before radiotherapy. Laryngeal sensation recovered in most cases within 1 year after radiotherapy. The present study clearly demonstrates the deterioration of laryngeal sensation with radiotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radiotherapy for laryngopharyngeal cancer plays an important role for organ preservation [1–3]. However, it sometimes leads to functional disabilities including swallowing dysfunction [2–5]. One of the reasons for these disabilities is a deterioration of laryngeal sensation. Laryngeal sensation is an important factor in swallowing [6–9], but quantitative evaluation of laryngeal sensation has been difficult. Aviv et al. described the use of an air-puff stimulator for quantitative evaluation of laryngeal sensation [7, 10], but such testing has been limited because of the special equipment required. In the present study, a novel method to measure laryngeal sensation using a flexible laryngoscope and probes previously developed by Yaguchi et al. was used [11, 12]. Yaguchi et al. evaluated and compared laryngeal sensation in young adults and elderly individuals using this method. In the present study, the same method was used to evaluate changes in laryngeal sensation before and after radiotherapy for laryngeal and hypopharyngeal cancer.
Materials and methods
This study was approved by the ethics committee and institutional review board of our hospital (No. 534, 534-2). All patients provided their written informed consent.
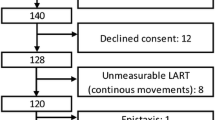
The study involved 12 patients with laryngeal (n = 8) or hypopharyngeal cancer (n = 4) who did not undergo surgery for the primary lesion, and underwent either radiotherapy alone or chemoradiotherapy. The patients’ mean age was 66.2 years (range 53–78 years). Four patients underwent radiotherapy alone, and eight underwent chemoradiotherapy. All patients achieved a complete response of the primary lesion. In two patients, neck dissection on the side of the lesion was performed within 1 month after completing radiotherapy for residual cervical lymph nodes. Table 1 shows the patients’ characteristics.
The test procedure was as follows. A novel flexible laryngoscope (ENF-Y0005), with a maximum diameter of 3.3 mm and a 1.2-mm probe port was co-developed with Olympus (Tokyo, Japan) in previous research [11, 12]. When compared with a conventional flexible laryngoscope with a forceps port, this flexible laryngoscope is narrower, has a curvature angle of 130°, and has excellent manoeuvrability (Fig. 1). The probes, also co-developed with Olympus, have a nylon filament attached to a wire tip and are protected by a sheath to prevent entanglement with the flexible laryngoscope. Four types of probes with nylon filament diameters of 0.06, 0.13, 0.20, and 0.30 mm were used (Fig. 1). These were prepared based on Semmes–Weinstein monofilaments, which are used to test sensation, for example, in diabetic peripheral neuropathy [12]. At the time of the study, the flexible laryngoscope and probes had not yet become commercially available, and they were provided by Olympus.
Flexible laryngoscopes and probes. The upper left photo shows all of the flexible laryngoscopes. The lower left photo compares the tips of the laryngoscopes. The top is a conventional flexible laryngoscope, and the bottom is the novel, thinner, and flexible laryngoscope. The right photo is a magnified view of the probe tips. The nylon filament diameters are a 0.06, b 0.13, c 0.2, and d 0.3 mm
To insert the flexible laryngoscope without using intranasal anaesthesia, 1:2,000 epinephrine was gently applied to widen the nasal cavity. The flexible laryngoscope was inserted to the oropharynx, and the probes were placed in contact with the tip of the epiglottis and the arytenoid region mucosa (at a non-tumour site in cases of hypopharyngeal cancer). Sufficient contact was made so that there was a slight bending of the probe (Fig. 2). The flexible laryngoscope and probes were manipulated, whenever possible, by the same person. Patients were asked to ring a buzzer or tap their hand when they felt the probe. For objective evaluation, the laryngeal adductor reflex was observed. Agreement between the subjective and objective findings was considered “positive.” Testing started with the thinnest probe, and the sensation level was based on the probe giving two of three positive responses.
Testing was performed four times; before radiotherapy, 1, 3 months, and 1 year after completing radiotherapy. Testing was stopped when the patient had severe pain or a strong gag reflex.
The Wilcoxon-signed rank test with Bonferroni correction was used to confirm significant differences between each testing time. A correlation between the sensation levels of the epiglottis and the arytenoid region was analysed using the Spearman’s rank correlation. Comparison of sensation levels between mild mucositis and severe mucositis was analysed using the repeated measures analysis of variance test.
The grade of radiation mucositis was classified based on the National Cancer Institute’s Common Terminology Criteria for Adverse Events v.3 (Table 2).
Results
Laryngeal paralysis did not occur before or after treatment in any patient, and arytenoid adduction during phonation was preserved. In patients 8 and 9, sensation testing 1 year after radiotherapy was cancelled because of lung metastasis and personal reasons, respectively.
Figure 3 shows the results of laryngeal sensation testing and the grade of radiation mucositis. Mucositis was mild in seven patients (grade 1 in 1 patient, grade 2 in 6 patients) and severe in five patients (grade 3 in 5 patients). All patients showed sensory deterioration of the epiglottis and/or the arytenoids until 3 months after radiotherapy. One year after radiotherapy, 60% of patients showed the same sensation levels in the epiglottis as before radiotherapy, or better sensation levels than at 1 or 3 months after radiotherapy. With respect to arytenoids sensation, 90% of patients showed the same sensation levels as before radiotherapy or better sensation levels than at 3 months after radiotherapy.
The sensation levels of the epiglottis and arytenoid; before, 1, 3 months, and 1 year after radiotherapy in each patient. Closed symbols (filled circle, filled triangle, filled square, filled diamond, filled inverted triangle) are the severe mucositis group; other symbols are the mild mucositis group
With respect to sensation of the epiglottis, the Wilcoxon-signed rank test with Bonferroni correction showed a significant deterioration (P < 0.017) in sensation 1 and 3 months after radiotherapy compared with before radiotherapy. However, there was no significant difference in sensation 1 year after radiotherapy when compared with before radiotherapy (P = 0.04). With respect to arytenoids sensation, the Wilcoxon-signed rank test with Bonferroni correction showed a significant deterioration (P < 0.017) in sensation 1 and 3 month after radiotherapy when compared with before radiotherapy, but at 1 year, the difference was not significant when compared with before radiotherapy (P = 0.12). There was a significant correlation (P < 0.0001) between the sensation levels of the epiglottis and the arytenoid region on the Spearman rank correlation.
Figure 3 also compares the sensation levels between mild mucositis and severe mucositis; there were no significant differences on the repeated measures analysis of variance test for both the epiglottis (P = 0.09) and the arytenoid region (P = 0.58).
Discussion
Radiotherapy of the laryngopharynx sometimes leads to functional disabilities including swallowing dysfunction [2–5]. The reasons for these disabilities are mucosal and muscular inflammation, fibrosis, reduced saliva secretion and deterioration of laryngeal sensation [4]. Laryngeal sensation is an important factor in swallowing [11], and we decided to evaluate laryngeal sensation. Procedures for testing laryngeal sensation by laryngoscope include fiberoptic endoscopic evaluation of swallowing with sensory testing (FEESST) with an air-puff stimulator, as described by Aviv et al. [10], direct mucosal contact with a flexible laryngoscope, and the use of probes, as discussed in the present report. FEESST is a minimally invasive procedure to quantify sensation by air pulses stimulating the laryngeal mucosa at a constant pressure and time [13–16], but the need for a special air-puff stimulator has limited its use. Direct contact with a flexible laryngoscope is simple, but it is not very quantitative, with large inter-operator variability. Our method using probes, originally described by Yaguchi et al. [12], permits semiquantitative evaluation, is minimally invasive, and is convenient for use in clinical settings; it allowed us to evaluate changes in laryngeal sensation before and after radiotherapy.
First, the test method used in the present study and its development are described. The novel narrow flexible laryngoscope with probe port was considered more appropriate for sensation testing because it was less irritating and unlikely to touch other sites during testing. In selecting an appropriate diameter of nylon filament to use with this method, Yaguchi et al. [12] considered Semmes–Weinstein monofilaments, which are used to measure tactile sensation by pressing nylon fibres against the skin. However, the thinnest commercially available nylon filament (diameter, 0.13 mm), in a kit from Arkray Inc. (Kyoto, Japan), is adequately perceived by the tongue. Therefore, Yaguchi et al. [12] decided to develop a thinner nylon filament with half the diameter (0.06 mm), and selected four sizes of nylon filaments for testing: 0.06, 0.13, 0.2, and 0.3 mm. We considered these sizes optimal for sensation testing, and the same size nylon filaments were used in the present study.
Our selection of measurement sites (the epiglottic tip and the arytenoid) was also based on the previous research [12]. These areas are innervated mainly by the superior laryngeal nerve, have a dense distribution of sensory fibres, and are relatively accessible to testing.
In determining the sensation level, Aviv et al. [16] and Yaguchi et al. [12] used subjective and objective findings, and a “positive” sensory response was based on the agreement between findings. Both authors reported a high correlation between findings. Therefore, in the present study, as in previous research, a “positive” response was based on the agreement between subjective and objective findings.
When evaluating laryngeal sensation using a flexible laryngoscope, Yaguchi et al. [12] limited the number of contacts to avoid patient discomfort, and estimated the sensation level based on two of three positive responses. Accordingly, in the present study, sensation level was based on two of three positive responses. Although increasing the number of contacts may improve repeatability and precision, we were concerned that increasing the number of contacts might be painful and uncomfortable for patients and may increase the study dropout rate.
Next, the measurement results are described. In this study, in both the epiglottis and the arytenoid, laryngeal sensation deteriorated significantly 1 and 3 month after radiotherapy compared with before radiotherapy. Parise et al. [14] evaluated laryngeal sensation in patients with dysphagia by FEESST, and they reported a direct association between radiotherapy of the head and neck and severe laryngeal sensation deficits. The present study also clearly demonstrates the deterioration of laryngeal sensation with radiotherapy. On the other hand, 1 year after radiotherapy, there was no significant difference compared with before radiotherapy for both the epiglottis and the arytenoid. As mentioned in our results, most patients showed the same sensation levels as before radiotherapy, or better sensation levels than 3 months after radiotherapy. Laryngeal sensation tended to recover 1 year after radiotherapy. However, we suggest the testing should be repeated 2 or 3 years after radiotherapy. According to Dietz et al. [2], 16% of patients who underwent chemoradiatiotherapy for larynx/hypopharynx carcinoma still showed dysphagia 3 years after chemoradiotherapy.
In the present study, a significant correlation was observed between the sensation levels of the epiglottis and the arytenoid region. The probes could be inserted into the forceps port of a conventional flexible laryngoscope. Therefore, in cases where tests are conducted using a conventional laryngoscope with a rather long diameter with a forceps port, or where measurement in the arytenoid region is difficult due to severe pain, it may be possible to determine deterioration of sensation in the arytenoid region to some degree by measuring the sensation in the epiglottis.
The reasons for deterioration of laryngeal sensation after radiotherapy need to be considered. Bodin et al. [17] reported that a dose of 64 Gy in the head and neck field can damage sensory nerves. Another study reported peripheral neuropathy in 75% of patients receiving radiotherapy doses of 63 Gy [18]. Neuropathologic features in peripheral neuropathy include necrosis and hyalinization of the media of small arteries, fibrous replacement of nerve fibres, demyelination, and fibrosis of the nerve sheath [19]. In the present study, 3 of 12 patients received 60 Gy, and the other 9 patients had doses of 66–70 Gy; thus, peripheral neuropathy was highly likely.
The loss of sensory receptors was also considered because, in a study on taste dysfunction in patients receiving radiotherapy to the oropharynx, pathologic analyses showed diminished taste buds [20]. In the same manner, radiotherapy of the laryngopharynx probably causes loss of sensory receptors.
In the present study, there was no significant difference in sensory deterioration and sensory recovery between the severe radiation mucositis group and the mild radiation mucositis group. However, based on the underlying mechanism, a correlation between grade of radiation mucositis and deterioration of laryngeal sensation is possible. This issue must be further investigated by accumulating more cases.
Finally, there have been reports of peripheral paresthesia caused by anticancer agents [21–23]. In the present study, we did not find a significant difference in deterioration and recovery of sensation with the combination of chemotherapy and radiotherapy, but this issue must also be further investigated by accumulating more cases.
Conclusion
A novel procedure using a flexible laryngoscope and probes allowed convenient evaluation of changes in laryngeal sensation in patients before and after radiotherapy. In both the epiglottis and the arytenoid, laryngeal sensation deteriorated significantly after radiotherapy. One year after radiotherapy, laryngeal sensation recovered in most cases.
References
Franchin G, Vaccher E, Politi D, Minatel E, Gobitti C et al (2009) Organ preservation in locally advanced head and neck cancer of the larynx using induction chemotherapy followed by improved radiation schemes. Eur Arch Otorhinolaryngol 266:719–726
Dietz A, Rudat V, Dreyhaupt J, Pritsch M, et al (2008) Induction chemotherapy with paclitaxel and cisplatin followed by radiotherapy for larynx organ preservation in advanced laryngeal and hypopharyngeal cancer offers moderate late toxicity outcome (DeLOS-I-trial). Eur Arch Otorhinolaryngol. doi: 10.1007/s00405-008-846-y
Rudat V, Eckel H, Volling P et al (2008) Long-term results of a prospective multicenter phase II study to preserve the larynx function using concomitant boost radiochemotherapy with carboplatin. Radiother Oncol 89:33–37
Jensen K, Lambertsen K, Grau C (2007) Late swallowing dysfunction and dysphagia after radiotherapy for pharynx cancer: frequency, intensity and correlation with dose and volume parameters. Radiother Oncol 85:74–82
van der Molen L, van Rossum MA, Burkhead LM, Smeele LE, Hilgers FJ (2009) Functional outcomes and rehabilitation strategies in patients treated with chemoradiotherapy for advanced head and neck cancer: a systematic review. Eur Arch Otorhinolaryngol 266:889–900
Aviv JE, Martin JH, Sacco RL, Zagar D, Diamond B, Keen MS, Blitzer A (1996) Supraglottic and pharyngeal sensory abnormalities in stroke patients with dysphagia. Ann Otol Rhinol Laryngol 105:92–97
Aviv JE, Martin JH, Keen MS, Debell M, Blitzer A (1993) Air pulse quantification of supraglottic and pharyngeal sensation: a new technique. Ann Otol Rhinol Laryngol 102:777–780
Ikegami S, Shoji K, Suzuki S, Kishimoto Y, Kojima T, Takahashi A (2006) Prediction of aspiration pneumonia by laryngopharyngeal sensory testing under flexible endoscopy. Jibirin 99:227–231
Sato S, Fujishima I, Setsu K, Katagiri N, Inao R, Mizuma M (2002) Evaluation for dysphagia by testing laryngeal sensation with a flexible laryngoscope. Nitisesshokuenngeriha 6:44–52
Aviv JE, Kim T, Sacco RL, Kaplan S, Goodhart K, Diamond B, Close LG (1998) FEESST: a new bedside endoscopic test of the motor and sensory components of swallowing. Ann Otol Rhinol Laryngol 107:378–387
Ishibashi A, Fujishima I, Takahashi H, Katagiri N, Ohno R et al (2007) A new method of laryngeal sensory testing using endoscopy and fine probes for patients with dysphasia. Jibi 53:S153–S161
Yaguchi H, Fujishima I, Ohno T (2006) A new method of testing laryngopharyngeal sensory discrimination using a flexible laryngoscope and probes. Jibi 52:S256–S262
Hafner G, Neuhuber A, Hirtenfelder S, Schmedler B, Eckel HE (2008) Fiberoptic endoscopic evaluation of swallowing in intensive care unit patients. Eur Arch Otorhinolaryngol 265:441–446
Parise Junior O, Miguel RE, Gomes DL, Menon AD, Hashiba K (2004) Laryngeal sensitivity evaluation and dysphagia: Hospital Sirio-Libanes experience. Sao Paulo Med J 122:200–203
Aviv JE, Liu H, Parides M, Kaplan ST, Close LG (2000) Laryngopharyngeal sensory deficits in patients with laryngopharyngeal reflux and dysphagia. Ann Otol Rhinol Laryngol 109:1000–1006
Aviv JE, Sacco RL, Mohr JP, Thompson JL, Levin B, Sunshine S, Thomson J, Close LG (1997) Laryngopharyngeal sensory testing with modified barium swallow as predictors of aspiration pneumonia after stroke. Laryngoscope 107:1254–1260
Bodin I, Jaghagen EL, Isberg A (2004) Intraoral sensation before and after radiotherapy and surgery for oral and pharyngeal cancer. Head Neck 26:923–929
Stoll BA, Andrew JT (1966) Radiation-induced peripheral neuropathy. Br Med J 2:834–837
Gillette EL, Mahler PA, Powers BE, Gillette SM, Vujaskovic Z (1995) Late radiation injury to muscle and peripheral nerves. Int J Radiat Oncol Biol Phys 31:1309–1318
Yamashita H, Nakagawa K, Tago M, Nakamura N, Shiraishi K, Eda M, Nakata H, Nagamatsu N et al (2006) Taste dysfunction in patients receiving radiotherapy. Head Neck 28:508–516
Krarup-Hansen A, Helweg-Larsen S, Schmalbruch H, Rorth M, Krarup C (2007) Neuronal involvement in cisplatin neuropathy: prospective clinical and neurophysiological studies. Brain 130:1076–1088
Ongerboer de Visser BW, Tiessens G (1985) Polyneuropathy induced by cisplatin. Prog Exp Tumor Res 29:190–196
Greven KM, White DR, Browne JD, Williams DW 3rd, McGuirt WF Sr, D’Agostino RB Jr (2008) Swallowing dysfunction is a common sequelae after chemoradiation for oropharynx carcinoma. Am J Clin Oncol 31:209–212
Acknowledgment
This work was supported in part by a Health and Labour Sciences Research Grant for Clinical Cancer Research (H20- ganrinshou- ippan-014) from the Ministry of Health, Labour and Welfare, Japan. Olympus (Tokyo, Japan) provided a flexible laryngoscope and probes for the study. No additional financial or personal support was provided.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Ozawa, K., Fujimoto, Y. & Nakashima, T. Changes in laryngeal sensation evaluated with a new method before and after radiotherapy. Eur Arch Otorhinolaryngol 267, 811–816 (2010). https://doi.org/10.1007/s00405-009-1069-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-009-1069-6