Abstract
Purpose
High caffeine intake during pregnancy is associated with restricted fetal growth. We aimed to evaluate the association between maternal caffeine intake during early and late pregnancy and the risk of delivering a small for gestational age (SGA) baby.
Methods
Kuopio Birth Cohort (KuBiCo) is a prospective cohort study including women whose pregnancies and deliveries were treated at the prenatal clinics in outpatient healthcare centers and in Kuopio University Hospital, Finland. Maternal diet and caffeine intake during the first (n = 2007) and third (n = 4362) trimester of pregnancy were assessed using a 160-item food frequency questionnaire (2013–2022). SGA was defined as birth weight corrected for gestational age below − 2 standard deviations from the mean, according to the sex-specific Finnish fetal growth curves.
Results
Altogether in 32 and 38% (1st and 3rd trimester) of all women and in 44 and 52% of coffee drinkers, caffeine intake exceeded the recommendation for caffeine intake (\(\le \)200 mg/day) during pregnancy. The women with moderate (51–200 mg/day) (aOR 1.87; 95% CI: 1.16–3.02) and high (> 200 mg/day) (aOR 1.51; 95% CI: 1.08–2.10) caffeine intake during the first trimester were in the highest risk of having an SGA newborn. Caffeine intake in the third trimester of pregnancy was not associated with SGA.
Conclusions
Moderate and high caffeine intake during early pregnancy is associated with SGA. As the results suggest that even moderate caffeine intake during the first trimester may increase the risk of SGA, the intake within recommendation limits does not necessarily appear to be safe for pregnant women and their newborns.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Special attention should be paid to consumption of caffeine in early pregnancy and when planning for pregnancy. |
Introduction
Caffeine is a widely used central nervous system stimulant among pregnant women. It presents in many foods and drinks, and coffee and tea are the major sources of caffeine in the maternal diet worldwide [1,2,3]. According to European Food and Safety Authority (EFSA) [4], pregnant women should limit daily caffeine intake to 200 mg per day which equals to two small cups (150 ml) or one mug (300 ml) of coffee. However, in our recent study, we found that more than 40% of pregnant women in our Finnish cohort consumed more caffeine than recommended [5].
The EFSA recommendation is based on the prospective cohort studies, which have shown a dose-dependent association between maternal caffeine intake and weight-related pregnancy outcomes, such as low birth weight, small for gestational age (SGA) and fetal growth restriction (FGR) [1, 6]. Several recently published observational studies and meta-analyses have also confirmed that higher maternal caffeine intake is associated with an increased risk of low birth weight [7,8,9] and poorer fetal growth, such as lower birth length, and head and/or thigh circumference [3, 9]. Even the use of caffeine within recommendations has been related to reduced fetal growth [9]. Although higher maternal caffeine intake is associated with an increased risk for diverse pregnancy outcomes such as miscarriage and stillbirth [10,11,12,13], according to the meta-analyses, the higher intake of caffeine does not appear to increase the risk of preterm birth [10, 14, 15].
SGA is typically defined as children born below the 2.5th–10th percentile of the reference birthweight by sex and gestational weeks in a region [16,17,18]. Unlike preterm birth (delivery < 37 weeks), the gestational age at birth of SGA newborns may therefore be normal, and on the other hand, some of them may be genetically small but healthy [19]. Globally, the prevalence of preterm SGA was estimated to be 1.1% and term SGA 16.3% [20], but the prevalence varies across different countries in relations to the populations and definition criteria. SGA is strongly related to neonatal health problems [21], the need for neonatal intensive care [22, 23], and neonatal morbidity and mortality [24]. In addition to the acute health problems of newborns, insufficient fetal growth may increase the risk of diabetes and cardiovascular diseases in adulthood [25,26,27]. Besides maternal caffeine intake, also maternal factors like poor nutritional status, infections, hypertension, smoking, alcohol and drug use, poor placental function and various fetal factors have been associated with the development of SGA [19, 28].
Caffeine is absorbed rapidly and it crosses the placenta freely [29, 30]. Since the fetus and placenta lack the major xenobiotic metabolizing enzymes (e.g. cytochrome P450 1A2; CYP1A2) for caffeine metabolism, it relies on the maternal metabolic capacity. The maternal enzyme function decreases during pregnancy and the half-life of caffeine increases from 5 to 18 h from the first to the third trimester [31]. Due to these metabolic changes, fetal exposure to caffeine increases and it accumulates to fetal tissues [32]. High caffeine levels in maternal blood are accompanied by higher cyclic adenosine monophosphate (cAMP), greater inhibition of phosphodiesterase (PDE) [33], and higher epinephrine levels [29] leading to an increased risk of intrauterine fetal asphyxia, pregnancy loss and restricted fetal growth. Genetic polymorphisms may influence the potential effects of caffeine and its metabolites on perinatal outcomes in different races [34].
Most of previous studies on maternal caffeine intake have focused on the anthropometry of newborns and gestational length. In this study, we prospectively examined the association between the maternal first and third trimester caffeine intake measured by a food frequency questionnaire (FFQ), SGA birth and neonatal health in the Kuopio Birth Cohort Study (KuBiCo) in Finland.
Methods
Study participants
In KuBiCo, pregnant women were recruited (majority, > 90% during the first trimester) by personnel at the prenatal clinics of outpatient healthcare centers in Northern Savo, Finland. The only inclusion criteria in the study were that the participants were expected to give birth after 22nd gestational week in Kuopio University Hospital (KUH) and to be proficient in Finnish.
During the first and third trimesters of pregnancy, three questionnaires were filled out by the study participants (Environmental exposure questionnaires, Food frequency questionnaires (FFQ1 and FFQ2) and Edinburgh Postnatal Depression Scale questionnaires). In addition to these, all pregnant women filled out various questionnaires evaluating the background risk for ongoing pregnancy in Kuopio University Hospital’s Pikku-Haikara system intended for pregnant women. By agreeing to the KuBiCo study, the women give permission for the use of all those and hospital data related to pregnancy and childbirth in the KuBiCo study.
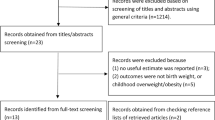
In this study, we included those who had given birth in KUH and whose dietary data were available. In total, 2007 (the first trimester) and 4362 (the third trimester) pregnant women, who had completed the FFQ between March 2013 and December 2022, were included in the study. Of these women, 1262 had completed both the first and third trimester FFQ. All women gave informed consent during recruitment. The study data were collected year-round with standardized, supervised methods according to the study protocol and it represent Finnish pregnant women well [35]. The overall participation in KuBiCo during 2013–2022 (7944 women) has been 35.2% of all parturients giving birth in KUH.
Maternal dietary assessment
Maternal diet was estimated using an FFQ filled by the participants during the first (up to 13rd week) and the third trimester of gestation (from 28th gestation week to delivery). The FFQ was designed to cover the whole diet during the preceding three months. Average daily nutrient and energy intakes were calculated using the Finnish national food composition (Fineli®) database in February 2023.
The FFQ used was a slightly modified version from that validated in the Kuopio Breast Cancer study [36]. To reflect the increased selection of food items available, for example information on the use of energy drinks and bars, were collected in the modified FFQ. In the KuBiCo, the participants completed the web-based FFQ which also produced automatized personal feedback to all study participants within 24 h after they returned the online FFQ.
The FFQ comprises a food list of 160 food and drink items with 9 frequency response options, ranging from ‘never’ to ‘6 or more times per day’. The portion sizes were fixed and specified with natural units (e.g., mug, glass, slice) or grams. The average daily intake of listed food items and nutrient intakes were calculated by multiplying the frequency of the food intake by the portion size (grams). The output provided more than 60 nutrients and 100 food groups. The caffeine intake was estimated by summarizing the daily intake of coffee (caffeine 70 mg/100 ml), cola drinks (20 mg/100 ml), tea (15 mg/100 ml), energy drinks (32 mg/100 ml), cocoa (3 mg/100 ml), and chocolate (30 mg/100 g).
Maternal and neonatal health examinations
In this study, the following descriptive characteristics were collected from the KUH birth registry: maternal age, body mass index (BMI; kg/m2) in the first trimester, weight change during pregnancy, smoking during pregnancy, the duration of education, relationship status, parity, the mode of delivery, and maternal diseases and complications. Also, newborn sex, the gestational age at birth, birth weight, head circumference, Apgar Scores (at 5 min), the duration of hospital stay after birth, the need of neonatal intensive care, and congenital anomaly (ICD-10, Q Codes) at birth, were recorded. According to WHO [37], low birth weight was defined as birth weight < 2500 g, and preterm birth was defined as delivery before 37 weeks of gestation. Macrosomia was classified as birth weight > 4500 g [38]. Further, we divided the birth weights into two subgroups according to birth weight for gestational age: SGA and large for gestational age (LGA). SGA and LGA were defined as birth weights corrected for gestational age beyond ± 2 standard deviations (SD) from the mean, according to the sex-specific Finnish fetal growth curves [39]. Maternal hypertension and pre-eclampsia were defined according to ICD-10 codes (O10, O11, O13, O14, O15 and O16).
Data analysis
The statistical analyses were conducted using IBM SPSS Statistics version 25 (SPSS Inc., Chicago, IL, USA). P-values < 0.05 were considered as significant. Caffeine intake was classified into three categories: low \(\le \)50 mg/d, moderate 51–200 mg/d and high caffeine intake > 200 mg/d. Caffeine and caffeine containing food intakes were expressed as the mean values with SD and the median values with interquartile range (IQR). Differences between the first and third trimester caffeine intakes were estimated by Wilcoxon test. Maternal and neonatal characteristics were expressed as the mean values with SDs in appropriate units or as percentages (%). Differences between caffeine intake groups were analyzed using ANOVA test for continuous variables and by Chi- square (χ2) test for categorical variables.
Logistic regression models were used to examine associations between maternal caffeine intake in categories and SGA. The results were expressed as odds ratios (ORs) with 95% confidence intervals (CIs) and P-values. Low-caffeine consumers were used as the reference group. Three regression models were used in the analyses. Model 1 was adjusted for maternal age and early pregnancy BMI. Model 2 was adjusted for model 1, smoking and energy intake. Model 3 was adjusted for model 2, the consumption of vegetables, fruits and berries and fish, and hypertension or pre-eclampsia during pregnancy. The association between the first trimester caffeine intake and SGA was also analyzed by dividing caffeine intake into quartiles, quintiles, deciles and into two groups based on the caffeine intake recommendation (\(\le/>\)200 mg). Also, coffee consumption was classified into tertiles and into two groups (\(\le/>\)100 ml), and the associations with SGA were examined by logistic regression. Pearson’s correlation was used to estimate the strength and the direction of the associations.
Results
Table 1 presents the maternal caffeine intake and the sources of caffeine during the first and third trimester of pregnancy. Median-caffeine intake during the first trimester of pregnancy was 121 mg/day and increased to 134 mg/day in the third trimester of pregnancy. The EFSA recommendation for caffeine intake (\(\le \)200 mg/day) was exceeded by 32% of the study participants in the first and 38% in the last trimester of the pregnancy. Median coffee intake during the first trimester of pregnancy was 118 ml/day and in the last trimester 150 ml/day. Coffee was the main source of caffeine, covering 74% and 75% of caffeine intake during the first and the third trimester of pregnancy, respectively. In the first trimester, 44% and in the third trimester, 52% of coffee drinkers consumed caffeine more than recommended. The consumption of tea, cola and energy drinks, cocoa, and chocolate increased from the first to the third trimester of pregnancy. Only 4% of women in the first trimester and 2% in the third trimester consumed energy drinks. The consumption of energy drinks during pregnancy correlated with smoking, younger age, and shorter education (detailed data not shown).
During the first trimester of pregnancy, 67.9% of women drank coffee, while during the third trimester of pregnancy the corresponding rate was 67.4%. The correlation coefficient between coffee consumption in FFQ1 and FFQ2 was 0.93 (P < 0.001). In total, 3.3% of women did not drink coffee in the first trimester but drank it during late pregnancy. In contrast, 3.9% of women drank coffee in the first trimester but stopped drinking it towards the end of pregnancy. It seemed that coffee consumption is relatively constant in this study population during pregnancy.
Maternal and neonatal characteristics according to the three caffeine intake groups are presented in Table 2. In both the first and the third trimester of pregnancy, caffeine intake was higher the higher the maternal age, parity and the daily energy intake were. In the first trimester, the caffeine intake was greater in women with higher early pregnancy BMI, and in the third trimester, in those with greater gestational weight gain. Women in the highest caffeine intake group also smoked more in both the first and third trimester of pregnancy (21% and 19%, respectively).
Regression models for neonatal risk of being SGA according to maternal caffeine intake during the first and last trimester of pregnancy are presented in Table 3. In model 1, adjusted with the maternal age and early pregnancy BMI, the women who consumed moderate (OR 1.69; 95% CI 1.06, 2.69) or high (OR 1.45; 95% CI 1.05, 1.99) amounts of caffeine during the first trimester of pregnancy were more likely to have SGA newborns as compared to the women with low caffeine intake. The association remained significant after additional adjustment in Model 2 (adjusted with model 1, smoking and energy intake) (OR 1.66; 95% CI 1.04, 2.64 for moderate consumers; OR 1.39; 95% CI 1.01, 1.93 for high consumers) and in Model 3 (adjusted with model 2, the consumption of vegetables, fruits and berries and fish, and hypertension or pre-eclampsia) (OR 1.87; 95% CI 1.16, 3.02 for moderate consumers; OR 1.51; 95% CI 1.08, 2.10 for high consumers). The trend was similar in sensitivity analyses with different caffeine intake categorizations.
Regarding coffee consumption, the risk of SGA was highest among the women with the highest coffee consumption during the first trimester of pregnancy. According to the regression model 3, women in the highest tertile of coffee consumption (151–900 ml daily) had OR 2.44 (95% CI 1.03, 5.78; P = 0.043) as compared to participants in the lowest tertile with 0–10 ml daily consumption. When coffee consumption was divided into two groups and adjusted with Model 3, the consumption of more than 100 ml of coffee daily was likely to associate with the increased the risk of SGA compared to lower consumption, but the result was not statistically significant (OR 1.73; 95% CI 0.88, 3.42; P = 0.112). Caffeine intake and coffee consumption during the third trimester of pregnancy were not associated with SGA.
Discussion
In this prospective birth cohort study in Finland, caffeine and its main source, coffee, were risk factors for SGA when the exposure was during the first trimester, but not when the exposure was during the third trimester. The risk of SGA increased considerably even when caffeine was used within EFSA recommendations (\(\le \)200 mg/day). Notably, the caffeine recommendations for pregnant women were exceeded by one-third of all women and half of coffee drinkers. The results can only be generalized to the Western population, where consumption of coffee is relatively high.
Our results are consistent with two earlier observational studies that have reported increased risks for SGA birth even with moderate caffeine intakes [21, 40]. However, in our study, the risk of SGA was much greater than found in these previous studies. Similarly to our study, Hoyt and associates [41] reported 57% increased risk for SGA birth with higher caffeine use (> 300 mg/day) in their population-based case–control study. According to the meta-analysis including 15 SGA studies, it was stated that each additional 100 mg daily amount of caffeine increase the risk of SGA by 10% [10]. In our study, dose response was not observed, rather the risk was highest with the moderate intake.
SGA
In our study, the risk of having an SGA newborn was 2% of all participants and 2.5–2.6% among women who consumed caffeine moderate or high amounts. Although the prevalence of SGA children born in this study population was low, a significantly higher prevalence was observed in the group of those who consumed the most caffeine (2.6%, n = 16/627) as compared to those in the lowest intake group (0.9%, n = 6/655) in the first trimester. The prevalence of SGA was at the similar level as in a Norwegian cohort study [21] and in an earlier Finnish birth cohort study [42]. The definition of SGA varies, and in some countries and studies, SGA has typically been defined as a newborn who is below the 10th percentile of birth weight for gestational age [17]. In our study, the definition of SGA was defined as having a birth weight more than two SDs below the mean weight for the gestational age which is stricter and gender and region-based way to select the cases. Compared to birth weight alone, SGA is more versatile concept for describing restricted fetal growth. In addition to SGA as a neonatal outcome, SGA newborns are in the risk for several health problems later in life.
In the analyses of this study, the associations between caffeine intake and SGA were strengthened when adjusted regression models were used. The association were most pronounced in the model with SGA-related covariates such as dietary factors and hypertension or pre-eclampsia. It is well known that caffeine intake is associated with unhealthy lifestyle habits, such as smoking [5, 43] which is also the known risk factor for SGA. Thus, we also adjusted the statistical analyses by smoking.
Exposures in early pregnancy may be more relevant for SGA because early pregnancy is an essential time for the development of the placenta and fetus. The placenta starts to develop in the very early pregnancy and maternal lifestyle can detrimentally influence early placental development and its function later [44] and contribute to restricted fetal growth [45]. Caffeine exposure during a sensitive time frame of pregnancy may also induce epigenetic changes in the developing fetus [46]. It is possible that the consumption of caffeine later in pregnancy does not affect fetal growth if the placenta has developed normally in the early pregnancy.
Caffeine intake during pregnancy
In Finland, coffee intake is the highest worldwide [47]. The Finnish recommendations for pregnant women state that caffeine should not be consumed more than 200 mg/day and energy drinks are not recommended during pregnancy at all [48]. Based on our recent and previous studies [5], pregnant women consume caffeine a lot. In this study, median-caffeine intake was 121 mg/day in early pregnancy and even higher, 134 mg/day in late pregnancy. In comparison to one recent Nordic study [21], maternal caffeine intake was much lower: median 58 mg/day during mid-pregnancy. The wide distribution of caffeine intake increases the reliability of our study. We also evaluated all dietary sources of caffeine, not only coffee. However, coffee was the primary source of caffeine covering three quarters of intake. Because the consumption of energy drinks was low during pregnancy (2–4% of pregnant women), it was not possible to assess its independent association with SGA.
According to our results, caffeine intake from various sources increases from the first to third trimester of pregnancy. We found that total caffeine intake during the first, but not the third trimester, was significantly associated with the increased risk of SGA. Because our FFQ covered the three preceding months, the first trimester questionnaire extended to the pre-pregnancy period in some participants, and since the first trimester FFQ was closed already at the end of the 13th week of pregnancy, not all study subjects completed the first nutrition questionnaire. Thus, if the results of our study were repeated in other studies, it would be important to extend caffeine recommendations also for women who are planning for pregnancy.
Nutrition studies have some limitations, such as self-reporting and recall bias related to the dietary intake methods. In caffeine-containing drinks, factors like the brand, the type of beans and leaves, preparation, and the amount of caffeine may also cause bias, considering our approximation of maternal caffeine intake [49]. However, Gleason et al. [9] found that the results from self-reported and biomarker-measured caffeine exposure are consistent with each other. As a dietary assessment method, the FFQ is reliable for epidemiological cohort studies like KuBiCo [50]. In this study, nutritional factors were assessed by using the validated and pregnancy-modified FFQ. The presented factors and limitations were addressed by using relevant statistical analyses with adjustments for several potential confounders. The strengths of this study were the population-based prospective study design and large range in caffeine intake due to the high consumption in Finland. Also, careful adjusting with potential cofounding factors brought novelty value to the research.
Conclusions
We found that moderate to high maternal caffeine intake during the first trimester of pregnancy was associated with the higher risk of delivering a SGA baby. Thus, even caffeine intake within the current recommendations (< 200 mg/day) may not appear to be safe for fetus. Because caffeine intake was exceeded in one third of all study women, and close to half of the coffee drinkers during the early pregnancy, recommendations for caffeine and coffee intake should be given to women already planning pregnancy. Our results also indicate that caffeine intake during early pregnancy is more significant for the development of SGA than caffeine intake later in pregnancy. Future studies should address more periconceptional factors and their importance in the placenta-related outcomes such as SGA.
References
Sengpiel V, Elind E, Bacelis J et al (2013) Maternal caffeine intake during pregnancy is associated with birth weight but not with gestational length: results from a large prospective observational cohort study. BMC Med 11:42. https://doi.org/10.1186/1741-7015-11-42
Miyake Y, Tanaka K, Okubo H et al (2019) Maternal caffeine intake in pregnancy is inversely related to childhood peer problems in Japan: The Kyushu Okinawa Maternal and Child Health Study. Nutr Neurosci 22:817–824. https://doi.org/10.1080/1028415X.2018.1450089
Chen LW, Fitzgerald R, Murrin CM et al (2018) Associations of maternal caffeine intake with birth outcomes: results from the Lifeways Cross Generation Cohort Study. Am J Clin Nutr 108:1301–1308. https://doi.org/10.1093/ajcn/nqy219
European Food Safety Authority (2015) Scientific opinion on the safety of caffeine. EFSA J 13:4102. https://doi.org/10.2903/j.efsa.2015.4102
Lehtonen A, Uusitalo L, Auriola S et al (2020) Caffeine content in newborn hair correlates with maternal dietary intake. Eur J Nutr 60:193–201. https://doi.org/10.1007/s00394-020-02231-2
Olsen, Bech, CARE Study Group (2008) Maternal caffeine intake during pregnancy and risk of fetal growth restriction: a large prospective observational study. BMJ 337:1334–1338. https://doi.org/10.1136/bmj.a2332
Jin F, Qiao C (2021) Association of maternal caffeine intake during pregnancy with low birth weight, childhood overweight, and obesity: a meta-analysis of cohort studies. Int J Obes 45:279–287. https://doi.org/10.1038/s41366-020-0617-4
Soltani S, Salari-Moghaddam A, Saneei P et al (2023) Maternal caffeine consumption during pregnancy and risk of low birth weight: a dose–response meta-analysis of cohort studies. Crit Rev Food Sci Nutr 63:224–233. https://doi.org/10.1080/10408398.2021.1945532
Gleason JL, Tekola-Ayele F, Sundaram R et al (2021) Association between maternal caffeine consumption and metabolism and neonatal anthropometry: a secondary analysis of the NICHD fetal growth studies-singletons. JAMA Netw Open 4:e213238. https://doi.org/10.1001/jamanetworkopen.2021.3238
Greenwood DC (2014) Caffeine intake during pregnancy and adverse birth outcomes: a systematic review and dose-response metaanalysis. Eur J Epidemiol 29(10):725–734
Jafari A, Naghshi S, Shahinfar H et al (2022) Relationship between maternal caffeine and coffee intake and pregnancy loss: a grading of recommendations assessment, development, and evaluation-assessed, dose-response meta-analysis of observational studies. Front Nutr 9:886224. https://doi.org/10.3389/fnut.2022.886224
Chen L-W, Wu Y, Neelakantan N et al (2016) Maternal caffeine intake during pregnancy and risk of pregnancy loss: a categorical and dose–response meta-analysis of prospective studies. Public Health Nutr 19:1233–1244. https://doi.org/10.1017/S1368980015002463
Li J, Zhao H, Song J-M et al (2015) A meta-analysis of risk of pregnancy loss and caffeine and coffee consumption during pregnancy. Int J Gynaecol Obstet 130:116–122. https://doi.org/10.1016/j.ijgo.2015.03.033
Maslova E, Bhattacharya S, Lin S-W, Michels KB (2010) Caffeine consumption during pregnancy and risk of preterm birth: a meta-analysis. Am J Clin Nutr 92:1120–1132. https://doi.org/10.3945/ajcn.2010.29789
Askari M, Bazshahi E, Payande N et al (2023) Relationship between caffeine intake and small for gestational age and preterm birth: a dose-response meta-analysis. Crit Rev Food Sci Nutr 1–11. https://doi.org/10.1080/10408398.2023.2177606
Campisi SC, Carbone SE, Zlotkin S (2019) Catch-up growth in full-term small for gestational age infants: a systematic review. Adv Nutr 10:104–111. https://doi.org/10.1093/advances/nmy091
Damhuis SE, Ganzevoort W, Gordijn SJ (2021) Abnormal fetal growth. Obstet Gynecol Clin North Am 48:267–279. https://doi.org/10.1016/j.ogc.2021.02.002
Wilcox AJ, Cortese M, McConnaughey DR et al (2021) The limits of small-for-gestational-age as a high-risk category. Eur J Epidemiol 36:985–991. https://doi.org/10.1007/s10654-021-00810-z
Osuchukwu OO, Reed DJ (2022) Small for gestational age. In: StatPearls. StatPearls Publishing, Treasure Island, FL
Lawn JE, Ohuma EO, Bradley E et al (2023) Small babies, big risks: global estimates of prevalence and mortality for vulnerable newborns to accelerate change and improve counting. Lancet 401:1707–1719. https://doi.org/10.1016/S0140-6736(23)00522-6
Modzelewska D, Bellocco R, Elfvin A et al (2019) Caffeine exposure during pregnancy, small for gestational age birth and neonatal outcome—results from the Norwegian Mother and Child Cohort Study. BMC Pregnancy Childbirth 19:80. https://doi.org/10.1186/s12884-019-2215-9
Hoffmire CA, Chess PR, Ben Saad T, Glantz JC (2012) Elective delivery before 39 weeks: the risk of infant admission to the Neonatal Intensive Care Unit. Matern Child Health J 16:1053–1062. https://doi.org/10.1007/s10995-011-0830-9
Abali S, Beken S, Albayrak E et al (2021) Neonatal problems and infancy growth of term SGA infants: does “SGA” definition need to be re-evaluated? Front Pediatr 9:660111. https://doi.org/10.3389/fped.2021.660111
Kramer MS (2013) Born too small or too soon. Lancet Glob Health 1:e7–e8. https://doi.org/10.1016/S2214-109X(13)70014-7
Barker D, Eriksson J, Forsén T, Osmond C (2002) Fetal origins of adult disease: strength of effects and biological basis. Int J Epidemiol 31:1235–1239. https://doi.org/10.1093/ije/31.6.1235
Li Y, Ley SH, Tobias DK et al (2015) Birth weight and later life adherence to unhealthy lifestyles in predicting type 2 diabetes: prospective cohort study. BMJ 351:h3672. https://doi.org/10.1136/bmj.h3672
Eriksson JG (2011) Early growth and coronary heart disease and type 2 diabetes: findings from the Helsinki Birth Cohort Study (HBCS). Am J Clin Nutr 94:S1799–S1802. https://doi.org/10.3945/ajcn.110.000638
Lee PA, Chernausek SD, Hokken-Koelega ACS et al (2003) International Small for Gestational Age Advisory Board Consensus Development Conference statement: management of short children born small for gestational age, April 24–October 1, 2001. Pediatrics 111:1253–1261. https://doi.org/10.1542/peds.111.6.1253
Darakjian LI, Kaddoumi A (2019) Physiologically based pharmacokinetic/pharmacodynamic model for caffeine disposition in pregnancy. Mol Pharm 16:1340–1349. https://doi.org/10.1021/acs.molpharmaceut.8b01276
Goldstein A, Warren R (1962) Passage of caffeine into human gonadal and fetal tissue. Biochem Pharmacol 11:166–168. https://doi.org/10.1016/0006-2952(62)90106-5
Knutti R, Rothweiler H, Schlatter C (1981) Effect of pregnancy on the pharmacokinetics of caffeine. Eur J Clin Pharmacol 21:121–126. https://doi.org/10.1007/BF00637512
Rhee J, Kim R, Kim Y et al (2015) Maternal caffeine consumption during pregnancy and risk of low birth weight: a dose-response meta-analysis of observational studies. PLoS One 10:e0132334. https://doi.org/10.1371/journal.pone.0132334
Daly JW (2000) Alkylxanthines as research tools. J Auton Nerv Syst 81:44–52. https://doi.org/10.1016/S0165-1838(00)00110-7
Grosso LM, Bracken MB (2005) Caffeine metabolism, genetics, and perinatal outcomes: a review of exposure assessment considerations during pregnancy. Ann Epidemiol 15:460–466. https://doi.org/10.1016/j.annepidem.2004.12.011
Huuskonen P, Keski-Nisula L, Heinonen S et al (2018) Kuopio birth cohort—design of a Finnish joint research effort for identification of environmental and lifestyle risk factors for the wellbeing of the mother and the newborn child. BMC Pregnancy Childbirth 18:381–389. https://doi.org/10.1186/s12884-018-2013-9
Männistö S, Virtanen M, Mikkonen T, Pietinen P (1996) Reproducibility and validity of a food frequency questionnaire in a case-control study on breast cancer. J Clin Epidemiol 49:401–409. https://doi.org/10.1016/0895-4356(95)00551-x
World Health Organization (2022) WHO recommendations for care of the preterm or low-birth-weight infant. WHO, Geneva
American College of Obstetricians and Gynecologists (2020) Macrosomia: ACOG Practice Bulletin, Number 216. Obstet Gynecol 135:e18–e35. https://doi.org/10.1097/AOG.0000000000003606
Sankilampi U, Hannila M-L, Saari A et al (2013) New population-based references for birth weight, length, and head circumference in singletons and twins from 23 to 43 gestation weeks. Ann Med 45:446–454. https://doi.org/10.3109/07853890.2013.803739
Kobayashi S, Sata F, Murata K et al (2019) Dose-dependent associations between prenatal caffeine consumption and small for gestational age, preterm birth, and reduced birthweight in the Japan Environment and Children’s Study. Paediatr Perinat Epidemiol 33:185–194. https://doi.org/10.1111/ppe.12551
The National Birth Defects Prevention Study, Hoyt AT, Browne M et al (2014) Maternal caffeine consumption and small for gestational age births: results from a population-based case-control study. Matern Child Health J 18:1540–1551. https://doi.org/10.1007/s10995-013-1397-4
Räisänen S, Gissler M, Sankilampi U et al (2013) Contribution of socioeconomic status to the risk of small for gestational age infants—a population-based study of 1,390,165 singleton live births in Finland. Int J Equity Health 12:28. https://doi.org/10.1186/1475-9276-12-28
Treur JL, Taylor AE, Ware JJ et al (2017) Smoking and caffeine consumption: a genetic analysis of their association: smoking and caffeine. Addict Biol 22:1090–1102. https://doi.org/10.1111/adb.12391
Reijnders IF, Mulders AGMGJ, Van Der Windt M et al (2019) The impact of periconceptional maternal lifestyle on clinical features and biomarkers of placental development and function: a systematic review. Hum Reprod Update 25:72–94. https://doi.org/10.1093/humupd/dmy037
Maulik D (2006) Fetal growth restriction: the etiology. Clin Obstet Gynecol 49:228–235. https://doi.org/10.1097/00003081-200606000-00006
Qian J, Chen Q, Ward SM et al (2020) Impacts of caffeine during pregnancy. Trends Endocrinol Metab 31:218–227. https://doi.org/10.1016/j.tem.2019.11.004
Finfood—Finnish Food Information (2023) Forkful of facts: Finnish Food Industry Statistics 2023. Finfood
National Institute for Health and Welfare in Finland (THL) Eating together—food recommendations for families with children
Leviton A (2018) Biases inherent in studies of coffee consumption in early pregnancy and the risks of subsequent events. Nutrients 10:1152. https://doi.org/10.3390/nu10091152
Shim JS, Oh K, Kim HC (2014) Dietary assessment methods in epidemiologic studies. Epidemiol Health 36:e2014009. https://doi.org/10.4178/epih/e2014009
Acknowledgements
We gratefully acknowledge the support of Juho Kopra from the statistical consulting services at the University of Eastern Finland.
Funding
Open access funding provided by University of Eastern Finland (including Kuopio University Hospital). Research Committee of the Kuopio University Hospital Catchment Area for the State Research Funding and the Pediatric Research Foundation for KuBiCo study. Juho Vainio Foundation, Finnish Food Research Foundation and Doctoral Programme in Health Sciences at the University of Eastern Finland for Anni Kukkonen.
Author information
Authors and Affiliations
Contributions
S Hantunen, L Keski-Nisula, M Pasanen, K Backman, T-P Tuomainen and R Voutilainen were involved in developing the study design. A Kukkonen analyzed the data, wrote the first draft of the manuscript, and had primary responsibility for the final content. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The research Ethics Committee of the Hospital District of Central Finland in Jyväskylä reviewed and approved the KuBiCo plan in 2011 (18U/2011). All participants gave informed consent during recruitment.
Consent to participate
All women gave informed consent during recruitment.
Consent to publish
All women gave informed consent during recruitment.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kukkonen, A., Hantunen, S., Voutilainen, A. et al. Maternal caffeine intake during pregnancy and the risk of delivering a small for gestational age baby: Kuopio Birth Cohort. Arch Gynecol Obstet 310, 359–368 (2024). https://doi.org/10.1007/s00404-024-07538-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-024-07538-7