Abstract
Objective
We aimed to study the association between obesity and survival in ovarian cancer (OC) patients, accounting for confounders as disease stage, histology, and comorbidities.
Methods
Retrospective matched case-control study of consecutive patients, with epithelial OC. Obese (body mass index [BMI] ≥ 35 kg m−2) patients were matched in a 1:4 ratio with patients having lower BMIs (BMI < 35 kg m−2) based on disease stage, cytoreduction state, tumor histology and ASA score. We compared the 3-year and total recurrence-free survival and overall survival through Kaplan–Meier survival curves and Cox proportional hazards.
Results
Overall, 153 consecutive patients were included, of whom 32 (20.9%) had a BMI ≥ 35. and 121 a BMI < 35. The median follow-up time was 39 months (interquartile range 18–67). Both study groups were similar in multiple prognostic factors, including American Society of Anesthesiologists physical status, completion of cytoreduction, histology and stage of disease (p = 0.981, p = 0.992, p = 0.740 and p = 0.984, respectively). Ninety-five (62.1%) patients underwent robotic surgery and conversion rate from robotic to laparotomy was similar in both groups 2 (6.3%) in obese group vs. 6 (5.0%) in lower BMI patients, p = 0.673. During the follow-up time, the rate of recurrence was similar in both groups; 21 (65.6%) in obese group vs. 68 (57.1%), p = 0.387 and the rate of death events was similar; 16 (50.0%) in obese group vs. 49 (40.5%), p = 0.333). The 3-year OS was higher in the obese group (log rank p = 0.042) but the 3-year RFS was similar in both groups (log rank p = 0.556). Median total OS was similar in both groups 62 months (95% confidence interval 25–98 months) in obese vs. 67 months (95% confidence interval 15–118) in the lower BMI group, log rank p = 0.822. Median RFS was similar in both groups; 61 months (95% confidence interval 47–74) in obese, vs. 54 (95% confidence interval 43–64), log rank p = 0.842. In Cox regression analysis for OS, including obesity, age, laparotomy and neoadjuvant treatment – only neoadjuvant treatment was independently associated with longer OS: odds ratio 1.82 (95% confidence interval 1.09–3.05) and longer RFS: odds ratio 2.16 (95% confidence interval 1.37–3.41).
Conclusions
In the present study on consecutive cases of ovarian cancer, obesity did not seem to be associated with outcome, except for an apparent improved 3-year survival that faded away thereafter.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Obesity does not seem to be associated with ovarian cancer outcome, Except for an apparent improved 3-year survival that fades away thereafter. |
Introduction
Ovarian cancer (OC) is the deadliest of gynecologic malignancies [1, 2], with an average lifetime risk of approximately 1.5%, [1, 3]. It is mostly diagnosed at a late stage and the stage at diagnosis is the most important predictor of overall survival [3]. Other main prognostic factors, among others, are age, tumor grade, and the amount of residual disease after cytoreduction [4].
In general, obesity is associated with greater mortality in patients with cancer [5]. However, in some specific cancers such as lung cancer, renal cell carcinoma, and melanoma obese patients have longer survival than their slimmer counterparts [5]. Several studies, including meta-analyses, have examined the association between obesity and OC survival, yielding conflicting results [6].
Considering the conflicting evidence, this study addresses the association of obesity with survival in OC patients taking into account confounders such as disease stage, histology, and comorbidities.
Materials and methods
Study population
The study population was composed of all consecutive patients who were diagnosed with and treated for International Federation of Gynecology and Obstetrics (FIGO) stages I–IV epithelial OC, including serous, endometrioid, clear cell and mucinous types, between 2006 and 2022. We categorized patient by body mass index (BMI) into two groups: (1) obese (BMI ≥ 35 kg m−2) and (2) lower BMI (BMI < 35 kg m−2).
Study design
We matched cases (obese) to controls (lower BMI) in a 1:4 ration, matched by disease stage, cytoreduction status at end of surgery, American Society of Anesthesiologists (ASA) score and tumor histology. No tolerance for matching was allowed. Cases with no matching controls—were excluded (n = 8). Data for the study were collected retrospectively from a prospectively maintained computerized database. We extracted information for each patient, including age, BMI, histologic type, grade, International Federation of Gynecology and Obstetrics (FIGO) stage, extent of cytoreduction at surgery and residual disease, administration of neoadjuvant chemotherapy (NACT), and type of surgery (robotic vs. laparotomy vs. conversion from robotics to laparotomy). The extent of cytoreduction was defined as R0 if no macroscopic disease was observed at the end of the operation; R1 cytoreduction was defined as total disease measuring less than 1 cm, and R2 was defined as total disease measuring more than 1 cm.
Overall survival (OS) was defined as the time from diagnosis to either last follow-up or death. In patients who had recurrence-progression-free survival (PFS) was defined as the time from diagnosis to recurrence. Recurrences were diagnosed clinically by patient symptoms or radiologically when triggered by abnormal CA-125 levels.
Statistical analysis
Statistical analysis was performed using SPSS 29 (IBM, Chicago, IL). Matching of cases to controls was performed by SPSS. Statistical significance was calculated using the chi-square test and Fischer’s exact test for differences in categorical variables, and the Mann–Whitney U test for continuous variables. Kaplan–Meier survival curves were used to calculate survival estimates (PFS and OS), and the log-rank test was used to quantify survival differences according to different variables. Cox regression analysis was performed to determine independent factors associated with OS and PFS.
Ethics approval
An institutional review board approval (protocol #15–070) was granted for this study, with yearly reviews.
Results
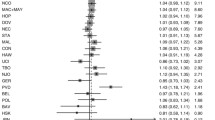
Overall, 153 patients were included in this study during 2006–2022, 32 (20.9%) obese patients (BMI ≥ 35.0) were matched with 121 patients with lower BMI. The median follow-up time was 39 months [interquartile range 18–67] and was similar in both groups (p = 0.572) (Table 1). The median BMI of the study groups were as follows: Obese 38.0 [IQR 36.0–41.9], lower BMI 24.6 [IQR 21.2–27.8]. Both study groups had similar ASA, residual disease after cytoreduction, histology and stage of disease (p = 0.981, p = 0.992, p = 0.740 and p = 0.984, respectively). Ninety-five (62.1%) patients underwent robotic surgery and conversion rate from robotic to laparotomy was similar in both groups 2 (6.3%) in obese group vs. 6 (5.0%) in lower BMI patients, p = 0.673. During the follow-up time, the rate of recurrence was similar in both groups; 65.6% (21 patients) in the obese group vs. 57.1% (68 patients), p = 0.387 and the rate of death events was similar; 50.0% (16 patients) in the obese group vs. 40.5% (49 patients), p = 0.333. Figure 1 presents 3-year OS in both study groups. The 3-year OS was higher in the obese group (log rank p = 0.042). Figure 2 present 3-year RFS, which was similar in both group (log rank p = 0.556). Survival curves for total OS and RFS are presented in Figs. 3and4. Median total OS was similar in both groups 62 months (95% confidence interval 25–98 months) in obese vs. 67 months (95% confidence interval 15–118) in lower BMI group, log rank p = 0.822. Median RFS was similar in both groups; 61 months (95% confidence interval 47–74) in obese vs. 54, 95% (confidence interval 43–64), log rank p = 0.842. Table 2 presents Cox regression for total OS, including obesity, age, laparotomy, and neoadjuvant treatment. Neoadjuvant treatment was the only independent factor associated with longer OS: odds ratio 1.82 (95% confidence interval 1.09–3.05). Table 3 presents Cox regression for RFS. Once again, neoadjuvant treatment was the only independent factor associated with longer RFS: odds ratio 2.16 (95% confidence interval 1.37–3.41).
Discussion
The major finding from this study is that obese women (BMI ≥ 35 kg m−2) have similar OS to their slimmer counterpart. There is an advantage in 3-year OS for obese patients, probably driven by lower recurrence rates during this period, and OS curves meet back at 5-years of follow-up. The only independent factor associated with OS and RFS is treatment with neoadjuvant chemotherapy.
Obesity has emerged as a significant factor influencing survival outcomes in many malignancies [7]. As it is theoretically modifiable, it is drawing increasing attention from the medical community. While the prevalence of obesity continues to rise, understanding and addressing the impact of obesity on OC survival is becoming increasingly crucial, with potential implications for clinical management and public health strategies. In OC, research has inconsistently shown different results. Some studies support that obese individuals with OC face a higher risk of both diagnosis at advanced stages and poorer OS [8,9,10,11]. These studies raise several mechanisms that possibly underlie this association, including chronic inflammation, hormonal imbalances, and insulin resistance, which can facilitate the growth and spread of OC. Furthermore, obesity can complicate surgical and chemotherapy interventions, potentially leading to suboptimal treatment outcomes. However, other studies found contrasting results [12,13,14,15], suggesting the‘obesity paradox’ [16]. Furthermore, many studies have found no association of BMI with OC survival [17,18,19].
Importantly, many of these studies did not account for prognostic factors other than BMI, which may explain these conflicting findings. It is therefore, that our study, which matched patients for comorbidities (e.g., ASA), disease stage, level of cytoreduction and the type of OC — sheds some additional light on the apparent controversy.
In our study, the 3-year survival rate was superior in obese patients. The recurrence-free survival in the first 3-years did not reach statistical significance, however the curves do separate. It is suggested that the superior 3-year OS may be driven by lower recurrence among obese patients in this period. One explanation may be that chemotherapy doses are calculated by weight formulas, and obese patients receive higher doses if not reduced as per patient’s tolerance [20]. However, it is possible that this gap may be explained by the obesity paradox.
The concept of the “obesity paradox” in cancer highlightens the unexpected phenomenon where obese individuals exhibit better outcomes in certain cancer types. While obesity is a well-established risk factor for various malignancies, recent studies have suggested that obese patients with cancer, particularly those with advanced stages or undergoing aggressive treatments, might experience improved survival rates. This intriguing observation has prompted extensive research into potential mechanisms underlying this paradox, such as enhanced energy reserves, metabolic adaptations, and differences in tumor biology [21,22,23].
Our study results indicating that obesity has no independent association with overall survival is in line with some previous literature [17, 18], however others have showed adverse outcomes [24], although none of these studies accounted for confounders as in our study.
Interestingly, the use of neoadjuvant chemotherapy was the only independent factor associated with improved survival in our study. While there are many confounders, this goes in line with a large study which underlined that higher provision of neoadjuvant chemotherapy is associated with improvements in median overall survival and larger decrease in the short-term mortality [25].
Our study has some limitations. First, this is a retrospective study, carrying inherent biases such as selection and information bias. Although in our study, all data were complete for each patient. Furthermore, as this is a retrospective study, it is impossible to account for many confounders, as provider bias, different treatment protocols as OC patients may undergo multiple lines of chemotherapy and dose interruptions. Furthermore, we must acknowledge the sample size of our study, which might be too small to identify statistical significance and to generalize. Further studies with larger sample size are needed to deepen the understanding of our findings. Nevertheless, the strength of our study is the matching in a 1:4 ratio for the most significant factors of disease outcome as disease stage and degree ofcytoreduction, as well as histology and patient’s comorbidities.
Conclusions
In this study, we found a temporary association, with obese patients having a limited overall survival advantage for the first 3 years, that then fades away with no further association with oncological outcome.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
Abbreviations
- OC:
-
Ovarian cancer
- OS:
-
Overall survival,
- RFS:
-
Recurrence-free survival
References
Lheureux S et al (2019) Epithelial ovarian cancer. Lancet 393(10177):1240–1253
Baldwin LA et al (2012) Ten-year relative survival for epithelial ovarian cancer. Obstet Gynecol 120(3):612–618
Pearce CL et al (2015) Population distribution of lifetime risk of ovarian cancer in the United States. Cancer Epidemiol Biomarkers Prev 24(4):671–676
Peres LC et al (2020) Predictors of survival trajectories among women with epithelial ovarian cancer. Gynecol Oncol 156(2):459–466
Petrelli F et al (2021) Association of obesity with survival outcomes in patients with cancer: a systematic review and meta-analysis. JAMA Netw Open 4(3):e213520
Yang HS et al (2011) Effect of obesity on survival of women with epithelial ovarian cancer: a systematic review and meta-analysis of observational studies. Int J Gynecol Cancer 21(9):1525–1532
Demark-Wahnefried W et al (2012) The role of obesity in cancer survival and recurrence. Cancer Epidemiol Biomarkers Prev 21(8):1244–1259
Pavelka JC et al (2006) Effect of obesity on survival in epithelial ovarian cancer. Cancer 107(7):1520–1524
Iyoshi S et al (2022) Obesity contributes to the stealth peritoneal dissemination of ovarian cancer: a multi-institutional retrospective cohort study. Obesity (Silver Spring) 30(8):1599–1607
Zhang M et al (2005) Body mass index in relation to ovarian cancer survival. Cancer Epidemiol Biomarkers Prev 14(5):1307–1310
Kjaerbye-Thygesen A et al (2006) Smoking and overweight: negative prognostic factors in stage III epithelial ovarian cancer. Cancer Epidemiol Biomarkers Prev 15(4):798–803
Münstedt K et al (2008) Influence of body mass index on prognosis in gynecological malignancies. Cancer Causes Control 19(9):909–916
Skírnisdóttir I, Sorbe B (2010) Body mass index as a prognostic factor in epithelial ovarian cancer and correlation with clinico-pathological factors. Acta Obstet Gynecol Scand 89(1):101–107
Bandera EV et al (2017) Impact of body mass index on ovarian cancer survival varies by stage. Br J Cancer 117(2):282–289
Bae HS et al (2014) The effect of body mass index on survival in advanced epithelial ovarian cancer. J Korean Med Sci 29(6):793–797
Lennon H et al (2016) The obesity paradox in cancer: a review. Curr Oncol Rep 18(9):56
Barrett SV et al (2008) Does body mass index affect progression-free or overall survival in patients with ovarian cancer? Results from SCOTROC I trial. Ann Oncol 19(5):898–902
Fotopoulou C et al (2011) Impact of obesity on operative morbidity and clinical outcome in primary epithelial ovarian cancer after optimal primary tumor debulking. Ann Surg Oncol 18(9):2629–2637
Suh DH et al (2012) Body mass index and survival in patients with epithelial ovarian cancer. J Obstet Gynaecol Res 38(1):70–76
Bandera EV et al (2015) Impact of chemotherapy dosing on ovarian cancer survival according to body mass index. JAMA Oncol 1(6):737–745
Childers DK, Allison DB (2010) The “obesity paradox”: a parsimonious explanation for relations among obesity, mortality rate and aging? Int J Obes (Lond) 34(8):1231–1238
Kocarnik JM et al (2016) Relationship of prediagnostic body mass index with survival after colorectal cancer: Stage-specific associations. Int J Cancer 139(5):1065–1072
Purcell SA et al (2016) Impact of body weight and body composition on ovarian cancer prognosis. Curr Oncol Rep 18(2):8
Nagle CM et al (2015) Obesity and survival among women with ovarian cancer: results from the ovarian cancer association consortium. Br J Cancer 113(5):817–26
Melamed A et al (2021) Association between overall survival and the tendency for cancer programs to administer neoadjuvant chemotherapy for patients with advanced ovarian cancer. JAMA Oncol 7(12):1782–1790
Funding
Open access funding provided by Hebrew University of Jerusalem. This study was supported by grants from the Israel Cancer Research Fund, the Gloria’s Girls Fund, and the Susan and Jonathan Wener Fund.
Author information
Authors and Affiliations
Contributions
GL, and WG: Conceptualization, formal analysis, investigation and methodology, writing—— original draft, and writing—— review and editing. YB, YT, TB, MB, SS, SL, and SS data acquisition, investigation, drafting and revising.
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest among all authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Levin, G., Brezinov, Y., Tzur, Y. et al. Association between BMI and oncologic outcomes in epithelial ovarian cancer: a predictors-matched case-control study. Arch Gynecol Obstet 310, 587–593 (2024). https://doi.org/10.1007/s00404-024-07537-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-024-07537-8