Abstract
Objective
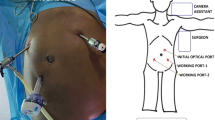
Laparoscopic surgery is the favored method for the surgical treatment of gynecologic diseases and malignancies. We have defined an anatomic landmark-based, easy-to-perform, and an alternative way of open laparoscopic entry technique named the ligamentum teres lift-up technique (TLU) that can be used in obese or normal-weight women to tackle the risks of the closed laparoscopic entry technique, namely, Veress needle entry (VNE).
Study design
In this retrospective comparative study, the participants were equally distributed to either the TLU group (n = 36) or the VNE group (n = 36) in a 1:1 ratio. The participants were stratified according to their BMI as follows: BMI between 20–25 kg/m2 (average weight), 25–30 kg/m2 (overweight), 30–35 kg/m2 (class I obesity), and 35–40 kg/m2 (class II obesity). Both laparoscopic access techniques were compared according to the entry time, vascular or visceral injuries, insufflation failures, trocar-related complications, and omental damage.
Results
The TLU group had a considerably shorter entry time than the VNE group (74.43 ± 21.45 s versus 192.73 ± 37.93 s; p < 0.001). Only one failed insufflation occurred in the VNE group (p = 0.32); however, that case was successfully insufflated with the TLU technique. Only one intestinal injury was seen in the VNE group, encountered during trocar site closure (p = 0.32). The subgroup analyses of the TLU and VNE groups based on BMI strata revealed a continuation of the statistical significance of entry time between BMI-matched groups.
Conclusion
The current study reveals that the new alternative TLU technique supplies an alternative, validated, and rapid access to the abdominal cavity in normal-weight and obese women. This new approach offers an easy-to-teach and easy-to-perform technique for surgical mentors and residents in gynecologic and oncologic surgeries.
Similar content being viewed by others
Data availability
The authors do not have the right to share any data information per their institution’s policies.
Code availability
Not applicable.
References
Koo YJ (2018) Recent advances in minimally invasive surgery for gynecologic indications. Yeungnam Univ J Med 35(2):150–155
Schorge JO (2020) Minimally Invasive Surgery in Morbidly Obese Women. Obstet Gynecol 135(1):199–210
Wang X, Li Y (2021) Comparison of perioperative outcomes of single-port laparoscopy, three-port laparoscopy, and conventional laparotomy in removing giant ovarian cysts larger than 15 cm. BMC Surg 21(1):20
Alkatout I (2017) Complications of laparoscopy in connection with entry techniques. J Gynecol Surg 33(3):81–91
Clapp B (2018) Optimal initial trocar placement for morbidly obese patients. JSLS. 22(4):e201700101
Ahmad G, Baker J, Finnerty J, Phillips K, Watson A (2019) Laparoscopic entry techniques. Cochrane Database Syst Rev. 1(1):CD006583
King NR, Lin E, Yeh C, Wong JMK, Friedman J, Traylor J et al (2021) Laparoscopic major vascular injuries in gynecologic surgery for benign indications: a systematic review. Obstet Gynecol 137(3):434–442
Fang Y, Huang H (2021) Abscess of ligamentum teres hepatis: a case report. Asian J Surg 44(10):1297–1299
Yamaoka T, Kurihara K, Kido A, Togashi K (2019) Four, “fine” messages from four kinds of “fine” forgotten ligaments of the anterior abdominal wall: have you heard their voices? Jpn J Radiol 37(11):750–772
Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ et al (2014) Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg 12:1500–1524
Thepsuwan J, Huang KG, Wilamarta M, Adlan AS, Manvelyan V, Lee CL (2013) Principles of safe abdominal entry in laparoscopic gynecologic surgery. Gynecol Minimally Invasive Therapy 2(4):105–109
Tinelli R, Litta P, Meir Y, Surico D, Leo L, Fusco A et al (2014) Advantages of laparoscopy versus laparotomy in extremely obese women (BMI>35) with early-stage endometrial cancer: a multicenter study. Anticancer Res 34(5):2497–2502
Colling KP, Glover JK, Statz CA, Geller MA, Beilman GJ (2015) Abdominal hysterectomy: reduced risk of surgical site infection associated with robotic and laparoscopic technique. Surg Infect (Larchmt) 16(5):498–503
Kassir R, Blanc P, Lointier P, Tiffet O, Berger JL, Amor IB, Gugenheim J (2014) Laparoscopic entry techniques in obese patient: veress needle, direct trocar insertion or open entry technique? Obes Surg 24(12):2193–2194
Lal P, Vindal A, Sharma R, Chander J, Ramteke VK (2012) Safety of open technique for first-trocar placement in laparoscopic surgery: a series of 6,000 cases. Surg Endosc 26(1):182–188
Ahmad G, O’Flynn H, Duffy JM, Phillips K, Watson A (2012) Laparoscopic entry techniques. Cochrane Database Syst Rev 2:CD006583
Fathi AH, Soltanian H, Saber AA (2012) Surgical anatomy and morphologic variations of umbilical structures. Am Surg 78(5):540–544
Funding
The authors declare they have no financial relationship with any company or product mentioned in this article.
Author information
Authors and Affiliations
Contributions
SA: conceptualization, methodology (lead), investigation, validation, visualization, writing-original draft (lead), writing-review and editing (lead), supervision (equal). CSU: investigation, supervision (equal). AU: conceptualization (lead), methodology, investigation, supervision. DL: investigation, validation. IG: validation (lead), visualization, writing-original draft. CBK: validation, visualization (lead), writing-original draft.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This retrospective comparative study was carried out as per the Helsinki Committee's principles after ethical approval of the study design by the Ethics Committee of Balikesir University (E-94025189-050.04-216887), and informed consent and consent to publish were acquired from all participants. STROBE (The Reporting of Observational Studies in Epidemiology) guidelines were followed during reporting [10].
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 27593 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Afsar, S., Usta, C.S., Usta, A. et al. Teres lift-up technique: a retrospective comparative study for an alternative route for laparoscopic entry in gynecologic and oncologic surgery. Arch Gynecol Obstet 308, 1549–1554 (2023). https://doi.org/10.1007/s00404-023-07191-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-023-07191-6