Abstract
Purpose
To compare the effects of using heated tobacco products (HTP) or traditional cigarettes (C) on maternal and neonatal outcomes.
Methods
This is a retrospective, monocentric study conducted at San Marco Hospital from July 2021 to July 2022. We compared a cohort of pregnant patients who smoked HTP (HS), with pregnant women smoking cigarettes (CS), ex-smoker (ES) and non-smoker (NS) pregnant women. Biochemistry, ultrasound, and neonatal evaluations were performed.
Results
In total, 642 women were enrolled, of which 270 were NS, 114 were ES, 120 were CS, and 138 were HS. CS had the greatest weight gain and had more difficulty getting pregnant. Smokers and ES experienced more frequently threats of preterm labor, miscarriages, temporary hypertensive spikes, and higher rates of cesarean sections. Preterm delivery was more associated with CS and HS groups. CS and HS had lower awareness of the risks to which the mother and the fetus are exposed. CS were more likely to be depressed and anxious. Biochemical parameters did not show significant differences between the groups. CS had the greatest difference in days between the gestational age calculated based on the last menstrual period and the one based on the actual ultrasound age. The average percentile newborn weight range of CS was lower, as well as the mean 1st minute and the 5th minute Apgar scores.
Conclusion
The comparison of the data obtained between CS and HS underlines the greater danger of C. Nevertheless, we do not recommend HTP because the maternal–fetal outcomes are not superimposable to the NS outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The comparison of maternal-fetal outcomes from the use of traditional cigarettes and heated tobacco products during pregnancy highlights the greater danger of the former, especially in relation to fetal growth, infertility problems, and the risk of preterm birth. | |
The use of heated tobacco is not recommended, considering that obstetric outcomes are not comparable with those of non-smokers. |
Introduction
Traditional cigarettes (C) represent a risk factor for over 17 types of tumors (on top of which lung and airway cancers) respiratory diseases (such as chronic obstructive pulmonary disease), and cardiovascular events multiplying the risk up to 5 times (as it acts damaging the endothelium and promoting atherosclerosis); it also represents a risk factor for osteoporosis, anxiety, and depression [1,2,3,4]. It can act on the reproductive system of both sexes causing a reduction in fertility [5,6,7,8,9,10,11,12,13,14], and in pregnancy, it has been shown to increase the risk of abortion [15, 16], preterm birth, premature rupture of membranes, and low birth weight [17, 18]. Despite the available data, up to 13% of pregnant women continue to smoke during pregnancy. Heated tobacco products (HTP) consist of devices placed on the market in 2014 that allow smoking of heated and unburned tobacco, thanks to the presence of a temperature regulation software that heats the tobacco contained in the stick up to 350 °C without ever reaching combustion: this would mean that about 90% of the normally toxic substances emitted by combustion are not produced, thus creating an advantage for both smokers and those exposed to smoke. It also contains about 50% less nicotine than cigarettes on the market. The reason that led us to address the present issue lies in the evidence of the growing number of smokers despite the few data in the literature, with the hope of finding data that allow us to understand if the use of HTP is less harmful than that of C. The long-term effects of these products are not yet known because of the few data in the literature despite the growing number of smokers: according to some studies, these devices could still cause inflammatory damage by increasing oxidative stress [19], while it has been reported that the effects of vasoconstriction, endothelial damage, and inflammation could be much lower than those induced by smoking [1].
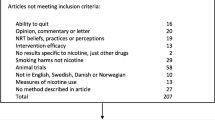
Materials and methods
Study design and population
This is a retrospective, monocentric cohort study including pregnant women attending San Marco Hospital from 1st July 2021 to 1st July 2022. Female patients with physiologic pregnancies were included in the study. Moreover, patients with a previous or current history of obstetrics pathologies (such as gestational hypertension and/or gestational diabetes) under control as well as those with physiologic twin pregnancies were also included in the analysis. Conversely, women with previous or obstetric pathologies that could have altered the significance of the results, monochorial monoamniotic twin pregnancies, and multiple pregnancies were excluded due to their high risk of complications. Women under 18 years were excluded. The patients included were divided into the following categories: non-smokers (NS), ex-smokers (ES), traditional cigarette smokers (CS), and heated tobacco cigarette smokers (HS). It was observed that in all cases, the HTP corresponded to the same type of device, namely “IQOS”.
Epidemiological and anamnestic evaluation
All patients underwent epidemiological evaluation through oral questionnaires and data about their age, profession, marital status, and schooling were obtained. They were all subjected to a specific smoking questionnaire, which included questions about the presence of cohabiting smokers, awareness of the risks and impact of smoking on the health of the fetus and mother, and their opinion on which product they exposed to a higher risk among CS and HS. Two questionnaires were then addressed separately which assessed the level of anxiety according to the Zung scale and the level of depression according to the PHQ-9 test. Questions about changes in smoking habits since the discovery of pregnancy and, if there was a reduction, the kind of reduction there was and in which week of gestation were asked only to smokers.
Questions about the number of cigarettes smoked daily and the duration of the smoking habit in annual terms were asked to smokers and ex-smokers. Moreover, it was asked whether smoking represented a practice sometimes aimed at replacing or reducing food consumption and appetite. The anamnestic evaluation used both oral questionnaires and patients' medical records to evaluate the number of previous pregnancies and the types of deliveries, the pre-pregnancy and the pre-partum body mass index (BMI), any difficulty in getting pregnant, any threat of preterm delivery, any blood pressure peaks during pregnancy, the gestational weeks at birth, the type of delivery, and whether labor induction was made. Finally, we recorded if a I trimester screening was done, and which test was performed between combined test and non-invasive prenatal testing (NIPT).
Biochemical evaluation
Pre-partum biochemical data were carried out during the hospitalization and processed by the analysis laboratory located in our institution and obtained using the “Modulab” laboratory management system. These parameters included: hemoglobin (Hb) (normal value, n.v. = 11.7–65–16 g/dL), platelets (PLT) (n.v. = 150,000–450,000/mm3), white blood cells (WBC) (n.v. = 5200–12.400/mm3), prothrombin time (PT) (n.v. = 11–13.5 s), international normalized ratio (INR) (n.v. = 0.8–1.2 s), activated partial thromboplastin time (APTT) (n.v. = 26–40 s), fibrinogen (n.v. = 170–450 mg/dL), antithrombin (AT) (n.v. = 75–125%).
Ultrasound evaluation
I, II, and III trimesters were done using the Voluson E6 ultrasound (US) system. I trimester US was performed between the 11th and the 13th gestational week, measuring the crown-rump length (CRL). II trimester morphology US was done between the 19th and 23rd gestational week, evaluating the parameters used for fetal biometry: biparietal diameter (BPD), head circumference (CC), abdominal circumference (CA), and femur length (FL). From these parameters, it was possible to calculate the gestational age (GA) based on the actual ultrasound age (AUA) according to Hedlock, and then extrapolate any difference in days with the GA calculated according to the last menstrual period (LMP), the estimated weight according to Hedlock and the corresponding weight percentile correspondent through the Intergrowth-21st software. The same procedure was applied for the evaluation of the III trimester growth US, carried out between the 29th and 33rd gestational week.
Neonatal evaluation
Through the maternal medical records, the neonatal weight was extrapolated (from which the percentile with respect to the gestational period at the time of delivery was obtained), the 1st minute and 5th minuteApgar scores, and umbilical cord blood gas values were obtained, in particular pH (n.v. 7.35–7.45), lactates (n.v. < 4 mEq/L), and base excess (n.v. − 2/ + 2 mmol/L).
Statistical analysis
Statistical analysis was performed by the arithmetic mean for each group of the following parameters: age, number of pregnancies, pre-pregnancy weight, pre-partum weight, pre-pregnancy BMI, pre-partum BMI, difference between pre-partum BMI and pre-pregnancy BMI, biochemical values, GA (LMP), GA (AUA), estimated weight and percentile corresponding to the I, II, and III trimester US, and the relative difference between GA (LMP) and GA (AUA), GA at delivery, neonatal weight and corresponding percentile, Apgar score, and blood gas analysis values. The percentages for each group of the following parameters were calculated: profession, marital status, education, parity, difficulty in becoming pregnant, threat of preterm birth, patients with blood pressure spikes, I trimester screening method, full-term and preterm births, type of delivery, induction and data extrapolated from smoking questionnaires.
Results
Epidemiological and anamnestic evaluation
In total, 642 pregnant women were enrolled, of which 270 were NS, 114 were ES, 120 were CS, and 138 were HS.
HS had the lowest mean age. Compared to the other three groups, NS more frequently had employment, were married and graduated. CS were more frequently pluriparous, had a greater weight gain (together with the HS), and had more difficulty getting pregnant. Most of the NIPTs were performed by NS and HS groups; conversely, most of the cases in which no I trimester screening test was done involved the other two groups. Smokers and ES experienced threats of preterm labor, miscarriages, temporary hypertensive spikes during pregnancy more frequently, and higher rates of cesarean deliveries (CD) than NS. Preterm delivery and induction of labor were more associated with CS and HS groups. Smokers and ES were more likely to have cohabiting smokers. CS and HS had lower awareness of the risks to which the mother and the fetus are exposed. We investigated their opinion about the possible different dangers between cigarettes and HTP, and it appeared that 55% of NS, 61% of ES, 35% of CS, and 24% of HS considered the two products at the same level of danger; on the other hand, 43%, 27%, 30%, and 76% of the respective categories believed that cigarettes expose to more risks, and 2%, 12%, 35%, and 0%, respectively, believed that HTP were more dangerous for maternal and fetal health. CS were more likely to be depressed according to the PHQ-9 test and anxious according to Zung than the other groups. 60% of CS and 78% of HS reduced the daily number of cigarettes smoked, and this occurred on average at 5 gestational weeks of amenorrhea. CS on average smoked more cigarettes per day and for more years than HS and ES. Finally, smokers and ES did not present significant differences on whether smoking constituted an expedient to replace and reduce the consumption of food. Epidemiological and anamnestic characteristics are illustrated in Table 1.
Biochemical evaluation
Biochemical parameters did not show significant differences between the groups, although CS had slightly lower Hb and higher PLT and WBC values. Biochemical data are displayed in Table 2.
US evaluation
In the II trimester US, CS had the greatest difference in days between GA (LMP) and GA (AUA) (NS = 0 vs. CS = 4 vs. HS = 1 vs. ES = 2), with greater involvement of the AC (NS = 152.2 vs. CS = 139.5 vs. HS = 156.9 vs. ES = 150.3), and the lowest weight percentile (NS = 60 vs. CS = 16 vs. HS = 58 vs. ES = 47).
Regarding the III trimester US, CS had the greatest difference in days between GA (LMP) and GA (AUA), followed by ES (NS = 0 vs. CS = 7 vs. HS = 0 vs. ES = 4), with greater involvement of the AC (NS = 276.0 vs. CS = 250.7 vs. HS = 270.3 vs. ES = 270.3). CS and ES had the lowest weight percentile (NS = 62 vs CS = 34 vs HS = 70 vs ES = 30). US outcomes are reported in Table 3.
Neonatal evaluation
The average percentile newborn weight range of CS was lower than the other categories of patients, as well as the mean 1st minute and the 5th minute Apgar scores. The umbilical cord gas values analyzed fell within the normal range: the only exception was found in average newborns’ pH from CS which was slightly highest. Neonatal data are illustrated in Table 4.
Discussion
In this study, we analyzed systematically for the first time epidemiological, biochemical, and US data to compare the maternal–fetal outcomes between the use of C and HTP during pregnancy.
Epidemiological and anamnestic evaluation
The epidemiological questionnaire allowed us to highlight the fact that CS were more often unemployed, single, and, together with HS, with a lower average education than NS. HS had a lower average age than the other groups, probably due to the greater diffusion of these products among the youngest. From the questionnaires relating to smoking habits, it emerged that the percentage of cohabiting smokers was much higher for CS (85%) than for other categories and that awareness of the risks to which smoking exposes was present in all NS and in almost all ES, while it was lower in CS and HS, respectively. Furthermore, their opinion on the different dangerousness between C and HTP highlighted that while most NS and ES considered HTP less dangerous or equal to the danger of C, 76% of HS considered C more dangerous, differently from CS. HS smoked on average the same amount as CS, and in both cases, more than half reduced their consumption as soon as they became aware of their pregnancy. Previous papers reported a higher rate of anxiety and depression among smokers [1,2,3,4] and these data were also confirmed by the present study. Moreover, in the present study, ES showed higher levels of anxiety than controls and this could have contributed to the cessation of smoking in anticipation of pregnancy. It has been shown that 1/3 of smokers used smoking as an expedient to replace and, therefore, reduce their food consumption. In fact, BMI gain during pregnancy was slightly higher in women who smoked. Smoking affects fertility, in fact CS in our population had infertility problems three times more often than NS, as other studies confirmed [5,6,7,8,9,10,11,12,13,14]. This occurs for several reasons: first, nicotine-induced vasoconstriction can reduce uterine blood flow and, therefore, cause difficulties in embryo implantation, and second it can interfere with estrogen production and, therefore, with menstrual cyclicality, as well as alter the process of maturation of the oocyte, damaging it and, therefore, reducing the ovarian reserve. On the other hand, HS, NS, and ES had the same rates of difficulty to get pregnant. In accordance with the literature, CS had a higher rate of miscarriages (six times higher) [15, 16] compared to NS. This correlation has been noted by several studies, even though it has never been close enough to be considered certain. To a lesser extent, HS have also been shown to have a higher abortion rate than NS, with percentages equal to those of ES. Most of the NIPT was performed by NS and HS groups, probably for a better economic condition; conversely, most of the cases in which no I trimester screening test was performed involved the other two groups. Cigarette smoking causes pro-inflammatory changes and an increase in oxidative stress, leading to various consequences: an increase in the production of prostaglandins, and therefore a stimulation of the uterine smooth muscle, an increase in the sensitivity of oxytocin receptors, and a reduction of progesterone production [17, 18]. All these changes greatly increase the risk of preterm birth. In fact, CS suffered five times more often than NS threatened with preterm birth, and they went into preterm birth four times more often. On the other hand, HS suffered of threat of preterm birth four times greater than NS, and of preterm birth two times greater than NS (in any case lower than CS). It is known that nicotine, being a vasoconstrictor agent, can induce hypertension, so cigarette smoking represents a risk factor for the development of gestational hypertension [20]. In 25% of CS, there were occasional pressure peaks during pregnancy, many more than those that occurred in other categories. Smokers of both categories and ES delivered by CD and have been subjected to labor induction more often than NS.
Biochemical evaluation
The blood count values were comparable among the categories of NS, ES, and HS, while they reveal slight alterations in CS, in particular: lower Hb values, and higher PLT and WBC values. The slightly lower Hb value could be explained by the fact that the carbon monoxide contained in tobacco interferes with the transportation of oxygen in the blood [21], while the higher WBC values could be due to the induced pro-inflammatory state from smoking. Values of the coagulation tests were comparable in the four categories, except the fibrinogen which was on average higher in CS, and these could be influenced by tobacco, representing a risk factor especially for venous thrombosis.
US evaluation
In the morphological US performed on CS, some data of fetal biometry were lower than in other categories, in particular those regarding the AC, as already stated in several studies [22]. GA (AUA) was on average lower than 4 days compared to GA (LMP), as well as the estimated weight (when compared to the corresponding percentile) was lower. In the growth US, some values of fetal biometry were lower in CS than in other categories too, as in the II trimester US. GA (AUA) was lower than 7 days compared to GA (LMP), as well as the estimated weight in relation to the growth percentile. In fact, several studies stated that the impact of smoking on fetal growth is visible since nutritional requirements increase, therefore from the II trimester onwards [23]. Compared to the morphological US values, the differences are more evident in the growth US, that is, in fact the period in which the uterus-placental flow must satisfy a greater nutritional requirement, precisely because the fetus has reached a higher weight. The fetuses of ES also showed a reduction in growth which becomes evident in the III trimester, and this testifies to the persistence of the vasoconstrictive effects induced by smoking that could become evident when fetal nutritional requirements increase. In fact, nicotine, as well as other toxic substances present in smoke, induces vasoconstriction which, as stated by several studies [24], can reduce the blood supply to the fetus, and therefore cause type 2 intrauterine growth restriction.
Neonatal evaluation
As other studies supported [25], the average newborn weight from CS was lower than the other categories, if compared with the corresponding percentiles: in particular, it was between the 10th and 25th percentiles (while in NS was between the 50th and 75th percentiles). On the other hand, newborns from HS had a slightly lower weight when compared to those born from NS (between the 25th and 50th percentiles), but were still similar to those of ES. The 1st minute and 5th minute Apgar scores from CS were slightly lower than the other groups. Dawood et al. [26] found that in heavy smokers, neonatal Apgar can have values even four times lower than the average. The umbilical cord gas values show physiological changes in the term newborn, such as a lower pH (7.18–7.38), and a base excess with lower values (between − 8 and − 0 mEq/L). All values analyzed in the present study were within the normal range: the only exception was found in those born from CS, in which an average pH value was slightly higher than in the other categories. As reported in previous studies [27], this could be linked to maternal hyperventilation caused by cigarette smoke which could also be reflected in the fetal acid–base balance. In fact, in this category, the lactate values were lower, and the base excess values were higher, in accordance with the pH. Due to the lack of long follow-up, we could not evaluate some newborn parameters, such as lung function during development, which was, however, evaluated in other studies in which reduced lung function was found in children born from mothers who smoked during pregnancy, as well as increased risk of developing asthma and lung infections [28, 29]. Moreover, it was not possible to evaluate the development of other organs, although several studies found, in some cases, underdevelopment of some organs (such as liver and kidneys) in children born from CS [30, 31]. The reason why maternal and fetal outcomes have a lower impact in HS than in CS could be explained by the fact that the amount of nicotine is 85% lower in HTP compared to the average values found in C, as well as the absence of numerous toxic substances released by C combustion (primarily carbon monoxide) which contribute to cause many obstetric problems. The values examined in ES showed that the effects of tobacco on the body can persist in the long term even after years of cessation. In fact, the percentages of miscarriages, preterm births, and blood pressure peaks were higher when compared with the percentages of NS. The II and III trimester fetal growth values observed by US were also lower than those found in NS.
This study has several strengths: it is the first of its kind to assess the risks associated with the use of HTP in pregnancy, the fact that the women were hospitalized and allowed us to carry out a precise anamnestic evaluation; the biochemical and US assessments were conducted at a single center. Nevertheless, it has some limitations: the design of the study (retrospective), and the total number of patients evaluated. Moreover, a large confounder is the fact that women who smoked appear to be older and from lower socio-economic levels than those who used heated tobacco products. Women who used heated tobacco products also appeared to be using it for fewer years than smokers. This potential bias may have influenced the results on the risk of preterm birth, infertility, and fetal growth restriction. Therefore, although there is a suggestion that heated tobacco products cause less harm, the risk of bias is present, and we cannot make a firm conclusion that using heated tobacco products is safer than smoking.
In conclusion, the comparison of the data obtained between CS and HS underlines the greater danger of C compared to HTP, especially in relation to fetal growth evaluated in different US, infertility problems, and the risk of preterm birth. The comparison between values obtained in NS and ES with those obtained in HS did not reveal any noteworthy differences, either at the anamnestic, laboratory or US level. A slight increase in the percentage of infertility, miscarriages, and preterm births was found in HS compared to NS, but comparable with the percentages found in ES. In fact, compared to NS, ES had a higher rate of miscarriages, preterm births, and blood pressure peaks, as well as a slight reduction in II and III trimester fetal growth parameters. Some effects induced by nicotine and tobacco toxicants are likely to persist long-term even after smoking cessation. These results do not represent an encouragement to the use of heated tobacco, which, therefore, is not recommended, considering that obstetric outcomes are not comparable with those of NS. Furthermore, more numerous and prospective studies, with long-term follow-up, are necessary to confirm these data and clarify the exact degree of danger associated with the use of HTP during pregnancy.
References
van der Toorn M, Frentzel S, De Leon H, Goedertier D, Peitsch MC, Hoeng J (2015) Aerosol from a candidate modified risk tobacco product has reduced effects on chemotaxis and transendothelial migration compared to combustion of conventional cigarettes. Food Chem Toxicol 86:81–87. https://doi.org/10.1016/j.fct.2015.09.016. (Epub 2015 Oct 1)
Haziza C, de La Bourdonnaye G, Donelli A, Poux V, Skiada D, Weitkunat R et al (2020) Reduction in exposure to selected harmful and potentially harmful constituents approaching those observed upon smoking abstinence in smokers switching to the menthol tobacco heating system 2.2 for 3 months (part 1). Nicotine Tob Res 22(4):539–548. https://doi.org/10.1093/ntr/ntz013
Haziza C, de La Bourdonnaye G, Donelli A, Skiada D, Poux V, Weitkunat R et al (2020) Favorable changes in biomarkers of potential harm to reduce the adverse health effects of smoking in smokers switching to the menthol tobacco heating system 2.2 for 3 months (part 2). Nicotine Tob Res 22(4):549–559. https://doi.org/10.1093/ntr/ntz084
Fagerström K (2012) The epidemiology of smoking. Drugs 62:2. https://doi.org/10.2165/00003495-200262002-00001
He S, Wan L (2023) Associations between smoking status and infertility: a cross-sectional analysis among USA women aged 18–45 years. Front Endocrinol (Lausanne) 19(14):1140739. https://doi.org/10.3389/fendo.2023.1140739
de Angelis C, Nardone A, Garifalos F, Pivonello C, Sansone A, Conforti A, Di Dato C, Sirico F, Alviggi C, Isidori A, Colao A, Pivonello R (2020) Smoke, alcohol and drug addiction and female fertility. Reprod Biol Endocrinol 18(1):21. https://doi.org/10.1186/s12958-020-0567-7
Tawfik H, Kline J, Jacobson J, Tehranifar P, Protacio A, Flom JD et al (2015) Life course exposure to smoke and early menopause and menopausal transition. Menopause 22(10):1076–1083. https://doi.org/10.1097/GME.0000000000000444
Fertil S (2006) Practice committee of the American society for reproductive medicine. Smoking Infertility. https://doi.org/10.1016/j.fertnstert.2006.08.018
Dechanet C, Anahory T, Quantin X, Reyftmann L, Hamamah S, Hedon B (2011) Effects of cigarette smoking on reproduction. Hum Reprod Update 17(1):76–95. https://doi.org/10.1093/humupd/dmq033
Mai Z, Lei M, Yu B, Du H, Liu J (2014) The effects of cigarette smoke extract on ovulation, oocyte morphology and ovarian gene expression in mice. PLoS ONE 9(4):e95945. https://doi.org/10.1371/journal.pone.0095945
Sterzik K, Strehler E, De Santo M, Trumpp N, Abt M, Rosenbusch B et al (1996) Influence of smoking on fertility in women attending an in vitro fertilization program. Fertil Steril 65(4):810–814. https://doi.org/10.1016/s0015-0282(16)58219-3
Barbieri RL, Sluss PM, Powers RD, McShane PM, Vitonis A, Ginsburg E et al (2005) Association of body mass index, age, and cigarette smoking with serum testosterone levels in cycling women undergoing in vitro fertilization. Fertil Steril 83(2):302–308. https://doi.org/10.1016/j.fertnstert.2004.07.956
Shiloh B, Lahav Baratz S, Koifman M, Ishai D, Bidder D, Weiner-Meganzi Z et al (2004) The impact of cigarette smoking on zona pellucida thickness of oocytes and embryos prior to transfer into the uterine cavity. Hum Reprod 19(1):157–159
Gruber I, Just A, Birner M, Lösch A (2008) Effect of a woman’s smoking status on oocyte, zygote, and day 3 pre-embryo quality in in vitro fertilization and embryo transfer program. Fertil Steril 90(4):1249–1252. https://doi.org/10.1016/j.fertnstert.2007.06.108. (Epub 1)
Mueller L, Ciervo CA (2023) Smoking in women. J Osteopath Med 98(s12):s7–s10. https://doi.org/10.1515/jom-1998-0124
Yuan S, Liu J, Larsson SC (2021) Smoking, alcohol and coffee consumption and pregnancy loss: a Mendelian randomization investigation. Fertil Steril 116(4):1061–1067. https://doi.org/10.1016/j.fertnstert.2021.05.103
Fantuzzi G, Aggazzotti G, Righi E, Facchinetti F, Bertucci E, Kanitz S et al (2007) Preterm delivery and exposure to active and passive smoking during pregnancy: a case-control study from Italy. Paediatr Perinat Epidemiol 21(3):194–200. https://doi.org/10.1111/j.1365-3016.2007.00815.x
Simpson WJ (1957) A preliminary report on cigarette smoking and the incidence of prematurity. Am J Obstet Gynecol 73(4):807–815
Sohal SS, Eapen MS, Naidu VGM, Sharma P (2019) IQOS exposure impairs human airway cell homeostasis: direct comparison with traditional cigarette and e-cigarette. ERJ Open Res 5(1):00159–02018. https://doi.org/10.1183/23120541.00159-2018
Qiuying Y, Shi WuW, Graeme S, Chen J, Krewski D, Chen XK, Walker MC (2006) Maternal cigarette smoking and the risk of pregnancy-induced hypertension and eclampsia. Int J Epidemiol 35(2):288–293. https://doi.org/10.1093/ije/dyi247
Calverley PM, Leggett RJ, McElderry L, Flenley DC (1982) Cigarette smoking and secondary polycythemia in hypoxic cor pulmonale. Am Rev Respir Dis 125(5):507–510. https://doi.org/10.1164/arrd.1982.125.5.507
Abraham M, Alramadhan S, Iniguez C, Duijts L, Jaddoe VW et al (2017) A systematic review of maternal smoking during pregnancy and fetal measurements with meta-analysis. PLoS ONE 12(2):e0170946. https://doi.org/10.1371/journal.pone.0170946
Hapangama D, Neilson JP (2009) Mifepristone for induction of labour. Cochrane Database Syst Rev 3:CD002865. https://doi.org/10.1002/14651858.CD002865.pub2
Davies CS, Ismail A (2016) Nicotine has deleterious effects on wound healing through increased vasoconstriction. BMJ 353:i2709. https://doi.org/10.1136/bmj.i2709
Johnston M, Ridella MS, Petzold AS (1981) Effect of maternal cigarette smoking on apgar scores. Am J Dis Child 135(6):503–506. https://doi.org/10.1001/ARCHPEDI.1981.02130300003003
Dawood MA, Al-Arnous MA (2002) The effect of maternal oxygen administration during the second stage of normal vaginal delivery or during cesarean section under general anaesthesia on umblical cord blood gases and acid-base state. Alexandria J Pediatr 16(2):233
Ayatbakhsh MR, Sadasivam S, Mamun AA et al (2009) Maternal smoking during and after pregnancy and lung function in early adulthood: a prospective study. Thorax 2009(64):810–814
Burke H, Leonardi-Bee J, Hashim A, Pine-Abata H, Chen Y, Cook DG et al (2012) Prenatal and passive smoke exposure and incidence of asthma and wheeze: systematic review and meta-analysis. Pediatrics 129(4):735–744. https://doi.org/10.1542/peds.2011-2196. (Epub 2012 Mar 19)
Spindel ER, McEvoy CT (2016) The role of nicotine in the effects of maternal smoking during pregnancy on lung development and childhood respiratory disease. Implications for dangers of E-cigarettes. Am J Respir Crit Care Med 193(5):486–494. https://doi.org/10.1164/rccm.201510-2013PP
Chen H, Saad S, Sandow SL, Bertrand PP (2012) Cigarette smoking and brain regulation of energy homeostasis. Front Pharmacol 25(3):147. https://doi.org/10.3389/fphar.2012.00147
Bosley AR, Sibert JR, Newcombe RG (1981) Effects of maternal smoking on fetal growth and nutrition. Arch Dis Child 56(9):727–729. https://doi.org/10.1136/adc.56.9.727
Funding
Open access funding provided by Università degli Studi di Catania within the CRUI-CARE Agreement. The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
GGI: conceptualization, methodology, writing—original draft. LG: investigation, data curation, writing—review and editing. MP: supervision, project administration, validation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This retrospective study was conducted in accordance with ethic guidelines for retrospective studies of our institution Ethics Committee of University of Catania. Patients’ anonymity was guaranteed. The principles of the Helsinki Declaration form were respected.
Consent to participate
Informed consent was obtained from all individuals included in the study.
Consent for publication
Informed consent was obtained from all individuals included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Incognito, G.G., Grassi, L. & Palumbo, M. Use of cigarettes and heated tobacco products during pregnancy and maternal–fetal outcomes: a retrospective, monocentric study. Arch Gynecol Obstet 309, 1981–1989 (2024). https://doi.org/10.1007/s00404-023-07101-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-023-07101-w