Abstract
Purpose
To reveal the prevalence of eating disorders (EDs) and related factors in pregnancy.
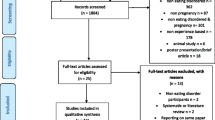
Methods
The search was performed in PubMed, EBSCOhost, Web of Science, Scopus, Google Scholar, and Ovid databases search up to April 3, 2022, using the keywords combination of "(eating disorders OR anorexia nervosa OR bulimia nervosa OR binge eating disorder) AND (pregnancy OR pregnant)". Two researchers independently extracted data from the articles using a standard form. We evaluated the quality of the studies according to the Joanna Briggs Institute assessment tools.
Results
The prevalence of EDs in pregnant women in the 11 studies involving 2,369,520 pregnant women was ranging between 0.5 and 10.6%. The prevalence of EDs in pregnant women was 4.3% (95% confidence interval 2%–9%; I2 = 99.5%). The prevalence of anorexia nervosa and binge eating disorder during pregnancy shows a statistically significant increase compared to pre-pregnancy, and the prevalence of bulimia nervosa during pregnancy decreases. The prevalence of EDs is higher in pregnant women under 30 years of age, secondary school graduates, married, and with normal BMI. Half of the pregnant women with EDs had anxiety and about one-third of pregnant women had depression. Excessive exercise is observed in 0.7% of pregnant women, fasting in 0.3%, laxative or diuretic use in 0.1%, and self-induced vomiting in 0.6%.
Conclusions
This study is important as it is the first systematic review and meta-analysis to reveal the global prevalence of EDs in pregnant women and related factors. Continuing routine screening tests to detect EDs during pregnancy may contribute to taking special preventive measures for risk groups and protecting mother–child health.
Trial registration
PROSPERO registration number (CRD42022324721), date of registration: 10/05/2022.



Similar content being viewed by others
Data availability
As this study is a meta-analysis of previous data, no new data were generated in support of this research.
References
Treasure J, Duarte TA, Schmidt U (2020) Eating disorders. Lancet (London, England) 395:899–911. https://doi.org/10.1016/S0140-6736(20)30059-3
American Psychiatric Association (2013) American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM-5), 5th edn. DC, USA, Washington
Bye A, Martini MG, Micali N (2021) Eating disorders, pregnancy and the postnatal period: a review of the recent literature. Curr Opin Psychiatry 34:563–568. https://doi.org/10.1097/YCO.0000000000000748
Bye A, Mackintosh N, Sandall J et al (2018) Supporting women with eating disorders during pregnancy and the postnatal period. J Heal Visit. https://doi.org/10.12968/JOHV.2018.6.5.224
Zauderer C (2012) Eating disorders and pregnancy: supporting the anorexic or bulimic expectant mother. J Obstet Gynecol Neonatal Nurs 41:S177–S178. https://doi.org/10.1111/J.1552-6909.2012.01363_25.X
Currin L, Schmidt U, Treasure J, Jick H (2005) Time trends in eating disorder incidence. Br J Psychiatry 186:132–135. https://doi.org/10.1192/bjp.186.2.132
Dörsam AF, Preißl H, Micali N et al (2019) The impact of maternal eating disorders on dietary intake and eating patterns during pregnancy: a systematic review. Nutrients 11:1–17. https://doi.org/10.3390/nu11040840
Sollid C, Clausen L, Maimburg RD (2021) The first 20 weeks of pregnancy is a high-risk period for eating disorder relapse. Int J Eat Disord 54:2132–2142. https://doi.org/10.1002/EAT.23620
Tierney S, Fox JRE, Butterfield C et al (2011) Treading the tightrope between motherhood and an eating disorder: aqualitative study. Int J Nurs Stud 48:1223–1233. https://doi.org/10.1016/J.IJNURSTU.2010.11.007
Mantel Ä, Hirschberg AL, Stephansson O (2020) Association of maternal eating disorders with pregnancy and neonatal outcomes. JAMA Psychiat 77:285–293. https://doi.org/10.1001/JAMAPSYCHIATRY.2019.3664
Zanardo V, Volpe F, Giliberti L et al (2018) Prepregnancy Body Mass Index shift across gestation: primary evidence of an association with eating disorders. J Matern Fetal Neonatal Med 33:415–420. https://doi.org/10.1080/14767058.2018.1494709
Mancini K (2017) Body image, eating attitudes and breastfeeding intention: implications for mental health and maternal child nurses. Issues Ment Health Nurs 38:750–755. https://doi.org/10.1080/01612840.2017.1324928
Martínez-Olcina M, Rubio-Arias JA, Reche-García C et al (2020) Eating disorders in pregnant and breastfeeding women: a systematic review. Medicina (B Aires) 56:1–19. https://doi.org/10.3390/MEDICINA56070352
Janas-Kozik M, Żmijowska A, Zasada I et al (2021) Systematic review of literature on eating disorders during pregnancy-risk and consequences for mother and child. Front psychiatry. https://doi.org/10.3389/FPSYT.2021.777529
PRISMA (2020) PRISMA
Methley AM, Campbell S, Chew-Graham C et al (2014) PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res 14:1–10. https://doi.org/10.1186/S12913-014-0579-0/TABLES/7
JBI (2022) Critical Appraisal Tools
Higgins J, Green S (2011) Cochrane Handbook for Systematic Reviews of Interventions. In: Cochrane Collab.
Baskin R, Meyer D, Galligan R (2020) Psychosocial factors, mental health symptoms, and disordered eating during pregnancy. Int J Eat Disord 53:873–882. https://doi.org/10.1002/EAT.23264
Bye A, Nath S, Ryan EG et al (2020) Prevalence and clinical characterisation of pregnant women with eating disorders. Eur Eat Disord Rev 28:141–155. https://doi.org/10.1002/erv.2719
Coker EL, Mitchell-Wong LA, Abraham SF (2013) Is pregnancy a trigger for recovery from an eating disorder? Acta Obstet Gynecol Scand 92:1407–1413. https://doi.org/10.1111/aogs.12256
Easter A, Bye A, Taborelli E et al (2013) Recognising the symptoms: how common are eating disorders in pregnancy? Eur Eat Disord Rev 21:340–344. https://doi.org/10.1002/erv.2229
Kolstad E, Gilhus NE, Veiby G et al (2015) Epilepsy and eating disorders during pregnancy: prevalence, complications and birth outcome. Seizure 28:81–84. https://doi.org/10.1016/j.seizure.2015.02.014
Larsen PS, Nybo Andersen AM, Olsen EM et al (2016) What’s in a self-report? A comparison of pregnant women with self-reported and hospital diagnosed eating disorder. Eur Eat Disord Rev 24:460–465. https://doi.org/10.1002/erv.2464
Maihara A, Rosana G, Benute GRG et al (2017) Presence of eating disorders and its relationship to anxiety and depression in pregnant women. Midwifery 51:12–15. https://doi.org/10.1016/j.midw.2017.05.005
Mohamadirizi S, Kordi M, Shakeri M, Modares-Gharavi M (2015) The relationship between eating disorder symptoms and obsessive compulsive disorder in primigravida women. Iran J Nurs Midwifery Res 20:642–646. https://doi.org/10.4103/1735-9066.170015
Watson HJ, Von Holle A, Hamer RM et al (2013) Remission, continuation and incidence of eating disorders during early pregnancy: a validation study in a population-based birth cohort. Psychol Med 43:1723–1734. https://doi.org/10.1017/S0033291712002516
Baskin R, Meyer D, Galligan R (2021) Predicting the change in perinatal disordered eating symptoms: an examination of psychosocial factors. Body Image 37:162–171. https://doi.org/10.1016/j.bodyim.2021.02.002
Ante Z, Luu TM, Healy-Profitós J et al (2020) Pregnancy outcomes in women with anorexia nervosa. Int J Eat Disord 53:403–412. https://doi.org/10.1002/eat.23251
Galmiche M, Déchelotte P, Lambert G, Pierre Tavolacci M (2019) Prevalence of eating disorders over the 2000–2018 period: a systematic literature review. Am J Clin Nutr 109:1402–1413
Knoph C, Von Holle A, Zerwas S et al (2013) Course and predictors of maternal eating disorders in the postpartum period. Int J Eat Disord 46:355–368. https://doi.org/10.1002/EAT.22088
Sebastiani G, Andreu-Fernández V, Herranz Barbero A et al (2020) Eating disorders during gestation: implications for mother’s health, fetal outcomes, and epigenetic changes. Front Pediatr. https://doi.org/10.3389/FPED.2020.00587
Larsen JT, Bulik CM, Thornton LM et al (2021) Prenatal and perinatal factors and risk of eating disorders. Psychol Med 51:870–880. https://doi.org/10.1017/S0033291719003945
Czech-Szczapa B, Szczapa T, Merritt TA et al (2015) Disordered eating attitudes during pregnancy in mothers of newborns requiring Neonatal intensive care unit admission: a case control study. J Matern neonatal Med 28:1711–1715. https://doi.org/10.3109/14767058.2014.966675
Ward ZJ, Rodriguez P, Wright DR et al (2019) Estimation of eating disorders prevalence by age and associations with mortality in a simulated nationally representative US cohort. JAMA Netw Open 2:e1912925–e1912925. https://doi.org/10.1001/JAMANETWORKOPEN.2019.12925
Zeeni N, Doumit R, Abi Kharma J, Sanchez-Ruiz MJ (2018) Media, technology use, and attitudes: associations with physical and mental well-being in youth with implications for evidence-based practice. Worldviews Evid-Based Nurs 15:304–312. https://doi.org/10.1111/WVN.12298
Udo T, Grilo CM (2018) Prevalence and correlates of DSM-5–Defined eating disorders in a nationally representative sample of U.S. Adults Biol Psychiatry 84:345–354. https://doi.org/10.1016/J.BIOPSYCH.2018.03.014
Kotwas A, Karakiewicz-Krawczyk K, Zabielska P et al (2020) The incidence of eating disorders among upper secondary school female students. Psychiatr Pol 54:253–263. https://doi.org/10.12740/PP/OnlineFirst/99164
Sundquist J, Ohlsson H, Winkleby MA et al (2016) School achievement and risk of eating disorders in a swedish national cohort. J Am Acad Child Adolesc Psychiatry 55:41. https://doi.org/10.1016/J.JAAC.2015.09.021
Fergus KB, Copp HL, Tabler JL, Nagata JM (2019) Eating disorders and disordered eating behaviors among women: associations with sexual risk. Int J Eat Disord 52:1310–1315. https://doi.org/10.1002/EAT.23132
Tabler J, Utz RL (2020) Hospitalization following eating disorder diagnosis: the buffering effect of marriage and childbearing events. SSM - Popul Heal. https://doi.org/10.1016/J.SSMPH.2020.100672
Spagnoletti BRM, Bennett LR, Kermode M, Wilopo SA (2018) “I wanted to enjoy our marriage first... but I got pregnant right away”: a qualitative study of family planning understandings and decisions of women in urban Yogyakarta. Indonesia BMC Pregnancy Childbirth 18:1–14. https://doi.org/10.1186/S12884-018-1991-Y/TABLES/2
Vartanian LR, Porter AM (2016) Weight stigma and eating behavior: a review of the literature. Appetite 102:3–14. https://doi.org/10.1016/J.APPET.2016.01.034
Koubaa S, Hällström T, Brismar K et al (2015) Biomarkers of nutrition and stress in pregnant women with a history of eating disorders in relation to head circumference and neurocognitive function of the offspring. BMC Pregnancy Childbirth. https://doi.org/10.1186/S12884-015-0741-7
Silvani J, Schmidt MI, Zajdenverg L et al (2020) Impact of binge eating during pregnancy on gestational weight gain and postpartum weight retention among women with gestational diabetes mellitus: LINDA-Brasil. Int J Eat Disord 53:1818–1825. https://doi.org/10.1002/EAT.23361
Demmler JC, Brophy ST, Marchant A et al (2020) Shining the light on eating disorders, incidence, prognosis and profiling of patients in primary and secondary care: national data linkage study. Br J Psychiatry 216:105–112. https://doi.org/10.1192/BJP.2019.153
Chapuis-de-Andrade S, de Araujo RM, Lara DR (2017) Association of weight control behaviors with body mass index and weight-based self-evaluation. Brazilian J Psychiatry 39:237–243. https://doi.org/10.1590/1516-4446-2016-2038
Marshall NE, Abrams B, Barbour LA et al (2022) The importance of nutrition in pregnancy and lactation: lifelong consequences. Am J Obs Gynecol. 226:607–632. https://doi.org/10.1016/j.ajog.2021.12.035
das Neves MC, Teixeira AA, Garcia FM, et al (2022) Eating disorders are associated with adverse obstetric and perinatal outcomes: a systematic review. Braz J Psychiatry. 44:201–2014. https://doi.org/10.1590/1516-4446-2020-1449
Ward N, Correia H, McBride N (2021) Maternal psycho-social risk factors associated with maternal alcohol consumption and fetal alcohol spectrum disorder: a systematic review. Arch Gynecol Obs 304(6):1399
Nurmi M, Rautava P, Gissler M et al (2022) Readmissions due to hyperemesis gravidarum: a nation-wide Finnish register study. Arch Gynecol Obs 306:1519–1529
Yu Y, Groth SW (2023) Risk factors of lower birth weight, small-for-gestational-age infants, and preterm birth in pregnancies following bariatric surgery: a scoping review. Arch Gynecol Obs 307:343–378
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study's conception and design. Material preparation, data collection, and analysis were performed by PÇÖ and ATO. The first draft of the manuscript was written by ATO and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Çiçekoğlu Öztürk, P., Taştekin Ouyaba, A. Prevalence and related factors of eating disorders in pregnancy: a systematic review and meta-analysis. Arch Gynecol Obstet 309, 397–411 (2024). https://doi.org/10.1007/s00404-023-07051-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-023-07051-3