Abstract
Purpose
This study aims to describe the differences in the urethral motion profile (UMP) of primiparous and multiparous women immediately postpartum.
Methods
This prospective study recruited 65 women (29 primiparous, 36 multiparous) one–seven days postpartum. The patients underwent a standardised interview and two-dimensional translabial ultrasound (TLUS). To evaluate the UMP, the urethra was manually traced and divided into five segments with six equidistant points. The mobility vector (MV) for each point was calculated as \(\sqrt{{{(V}_{y}-{R}_{y})}^{2}+{{(V}_{x}-{R}_{x})}^{2}}\). A Shapiro–Wilk test was conducted to test normality. An independent t-test and a Mann–Whitney test were conducted to express differences between the groups. The Pearson correlation coefficient was used to determine the relationships among MVs, parity and confounders. Finally, a univariate generalised linear regression analysis was performed.
Results
MV1–MV4 were found to be normally distributed. A significant difference for all MVs, except for MV5, was demonstrated between parity groups (MV1: t = 3.88 (p < .001), MV2: t = 3.82 (p < .001), MV3: t = 2.65 (p = .012), MV4: t = 2.54 (p = .015), MV6: U = 150.00 (exact sig. two tailed = .012)). A strong-to-very strong mutual correlation was observed between MV1 to MV4. The univariate generalised linear regression showed that parity can predict up to 26% of urethral mobility.
Conclusion
This study shows that multiparous women have significantly higher urethral mobility compared to primiparous women in the first week postpartum, with the most significant effect observed in the proximal urethra.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This study shows that multiparous women have a significantly greater urethral mobility compared to primiparous women in the first week postpartum. Since SUI is known to be associated with increased mobility of the proximal urethra, this study’s findings can instigate further research on the value of the UMP to predict SUI in daily practice. |
Introduction
Pregnancy and childbirth are associated with changes in the pelvic floor structures. Compared to caesarean section, vaginal delivery is associated with an increased number of levator ani defects, increased bladder neck mobility and enlargement of the hiatal area. These are all known risk factors for organ prolapse and urinary incontinence [1]. Bladder neck mobility and changes in urethrovesical angle are also associated with urinary incontinence and parity [2].
Several hypotheses have been proposed regarding the origin of these changes. Labour can cause laxity through stretching of the muscles and connective tissue or through damaging events, such as lacerations or episiotomies. Stretching of the pudendal and pelvic nerves is also described as a potential reason for urethral sphincter insufficiency [3, 4].
To evaluate the pelvic floor, several ultrasound methods, such as endovaginal, endoanal, transabdominal and transperineal or translabial ultrasound (TPUS/TLUS), are used. TPUS and TLUS are used interchangeably and will be referred to as TLUS hereafter in this article. Since 1986, TLUS has been increasingly used to image the pelvic floor, allowing more insight into the correlation between pelvic floor changes and complaints and, thus, improving treatment and prevention strategies [5].
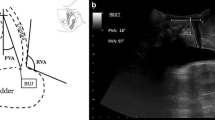
Bladder neck mobility was among the first parameters to be described with TLUS [5]. In 2008, Shek and Dietz investigated and validated a new method to study the urethra in its entirety: the urethral motion profile (UMP) [6]. This parameter assesses urethral mobility using coordinates of six equidistant points along the urethra length in rest and during Valsalva, allowing the full length of the urethra to be considered.
An increase in urethral mobility assessed by the UMP has been observed in a population of primigravidae postpartum compared to prepartum, as well as in parous women compared to nulliparous women [6,7,8]. However, neither the effect of subsequent childbirth on the UMP nor the association of the UMP with stress urinary incontinence (SUI) has yet been investigated. This study aims to measure and compare the UMP of primiparous and multiparous women in the immediate postpartum period to determine changes in urethral mobility after childbirth between these groups. We hypothesise that a significant difference can be found in the UMP between primiparous and multiparous women in the immediate postpartum period.
Materials and methods
This descriptive prospective cohort study was conducted according to the Reporting of Observational Studies in Epidemiology guidelines [9]. After receiving approval from the local Ethics Committee of Antwerp University Hospital, women were recruited at the maternity ward of a tertiary hospital between March 2021 and December 2021. In total, 65 women were enrolled after they provided their informed consent. All participants were at least 18 years old and were approached 1–7 days after vaginal delivery. The exclusion criteria involved not being able to communicate in Dutch or English, preterm childbirth (defined as gestational age less than 37 weeks) and multiple pregnancy. The participants were divided into two groups according to parity: primiparous and multiparous women. A sample size of 114 was deemed necessary to compare the means of the two sample groups, with a power level of 80% (b = 0.20) and a significance level of 95% (a = 0.05). A mean sample size calculator was used (www.sample-size.net) with values derived from Chan et al. article [10]. After the inclusion, the participants were subjected to a standardised interview. As no confounding or modifying factors of the UMP have been described in the literature so far, the questionnaire was based on confounding or modifying factors known to be associated with the presence of pelvic floor dysfunction, such as parity, instrumental delivery, age, ethnicity (Caucasian), body mass index (BMI), chronic obstructive pulmonary disease, connective tissue diseases and gestational diabetes mellitus [11, 12]. Birth weight, former or present anal sphincter injuries and former or present episiotomy were also included.
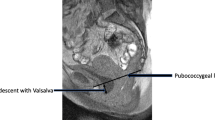
Thereafter, a two-dimensional (2D) translabial ultrasound was performed in accordance with the guidelines of the International Urogynecology Association Special Interest Group Imaging using the GE Healthcare Voluson S6 equipped with a 4D convex transducer (RAB 4-8-RS, 2–8 MHz). The probe was placed translabially to visualise the urethra in the midsagittal plane. Two images were acquired in the supine position after bladder emptying, one at rest and one on maximal Valsalva manoeuvre. At least three Valsalva manoeuvres were performed for each patient, of which the image showing maximum pelvic organ descent was used for further analysis. Data collection was performed by three researchers (DD, NM and TL). Measurement and interpretation of the ultrasound data were performed by TL on offline pseudonymised datasets, using OS X. Horos (version 3.3.6, 2019) [13]. The urethra was manually traced in the midsagittal plane on.dcm images with identification of the bladder neck (point 1) and external meatus (point 6) for both at rest and on maximal Valsalva. The traced length was then divided into five segments with six equidistant points, as shown in Fig. 1. Per point, the horizontal (y-coordinate) and vertical (x-coordinate) distances relative to the dorsocaudal margin of the pubic symphysis were measured. The mobility vector (MV) for each of the six points was calculated as\(\sqrt{{{(V}_{y}-{R}_{y})}^{2}+{{(V}_{x}-{R}_{x})}^{2}}\). This manual measurement method of the UMP is proven to be highly reproducible, with an intraclass correlation coefficient (ICC) of 0.80 [95% CI 0.73–0.86] [6]. To test the intra-rater reliability, a test–retest series on the datasets of five patients was performed, where the determination of the UMP points and calculation of MV1 were repeated five times per patient. The ICC was computed using a single-rater, absolute-agreement, two-way mixed-effects model. The ICC amounted to 0.86 (p < 0.001, [95% CI 0.60–0.98]), suggesting moderate-to-good intra-rater reliability [14]. All data were inserted into Microsoft Excel (version 16.16.4, 2018). All statistical analyses were computed using IBM® SPSS® statistical package version 28.0. Descriptive statistics were performed to assess the baseline differences between the two groups in terms of characteristics. Continuous variables were expressed as mean and standard deviation (SD), and categorical variables were expressed as number (n) and percentage (%). Normal distribution of the MVs was tested using Shapiro–Wilk analysis. Outliers were identified using Q–Q plots and Z-scores and defined as a Z-score lesser or greater than \(\left| 3 \right|\) for the respective MV. The effect of subsequent childbirth on urethral mobility was studied to determine the difference between the MVs of primiparous and multiparous women, using an independent t-test for normally distributed data and a Mann–Whitney test in the absence of normal distribution. A p-value of less than 0.05 was considered statistically significant. Subsequently, all MVs were correlated with parity and each other, as well as with the queried confounding and effect-modifying factors through the Pearson correlation coefficient. The confounder ‘delivery mode’ was investigated through the parameters ‘current delivery mode’ (non-instrumental or instrumental vaginal delivery), ‘delivery mode history’ and ‘overall mode of delivery’. For the multiparous group, the delivery mode history was divided into three categories, ranked by the impact on the pelvic floor (1: only C-sections in history, 2: history of at least one vaginal delivery, 3: history of at least one instrumental delivery). The overall mode of delivery was defined as the ‘overall most damaging delivery mode’ in terms of pelvic floor injuries. As the current vaginal delivery was the inclusion criterion, two categories were established (1: only non-instrumental vaginal deliveries, 2: at least one instrumental vaginal delivery). The confounder ‘perineal defect’ (anal sphincter injury and/or episiotomy) was investigated through the parameters ‘overall highest grade of perineal defect’, ‘highest grade of perineal defect in history’ and ‘current grade of perineal defect’. Anal sphincter injuries (ASIs) were coded according to OASI classification, and episiotomy was coded as grade 2 [15]. ‘Overall highest grade of perineal defect’ refers to the highest grade of perineal defect in current and previous deliveries. Finally, a univariate generalised linear regression analysis was performed to investigate the predictive value of parity on urethral mobility and the statistically significant correlated factors.
Results
Of the 65 women included, 29 (44.6%) were primiparous and 36 (55.4%) were multiparous (P2 n = 28; P3 n = 5; P4 n = 2; P5 n = 1). Their age ranged from 20 to 40 years old (mean 30.7 ± 4.8). Most participants (n = 56, 86.2%) were Caucasian. Fifty-two (80.0%) had given birth by non-instrumental vaginal delivery, 13 (20.0%) by vacuum extraction and none by forceps. Their pre-pregnancy BMI ranged from 15.8 to 40.4 (mean 24.1 ± 4.6), with 2 (3.1%) being underweight and 8 (12.3%) having a BMI above 30. Both groups were comparable in terms of BMI, gestational age and newborn birthweight. Nineteen cases were excluded based on the ultrasound images: one due to the impossibility of attaining an adequate Valsalva manoeuvre, one because the inclusion criteria were not met and 17 because the ultrasound images were technically inadequate for UMP determination. The remaining 46 datasets with complete UMP determination were included in the final statistical analysis. The distribution between primiparous and multiparous women after exclusion was 22 (47.8%) and 24 (52.2%), respectively. A comparison of the mean MV from the bladder neck (point 1) to the external meatus (point 6) for the primiparous and multiparous women is shown in Table 1. According to the result of the Shapiro–Wilk test for normality, MV1–MV4 were normally distributed (MV1 D(46) = 0.97, p = 0.22, MV2 D(46) = 0.96, p = 0.09, MV3 D(46) = 0.97, p = 0.27, MV4 D(46) = 0.96, p = 0.14). MV5 and MV6 had no normal distribution, with MV5 D(46) = 0.90, p < 0.001 and MV6 D(46) = 0.93, p = 0.009. Case 042 was identified as an outlier for MV5 (MV5 = 1.437 cm, Z-score = 3.26). After excluding case 042, the MV5 values remained not normally distributed (D(45) = 0.93, p = 0.007). Further statistical analysis for MV5 was conducted with the exclusion of case 042. An independent t-test demonstrated a significant difference between MV1 and MV4 of primiparous and multiparous women, as shown in Table 1. MV1 and MV2 had the largest effect sizes of Cohen’s d = 0.54, [95% CI − 1.77 to − 0.52] and d = 0.48 [95% CI − 1.73 to − 0.48], respectively, followed by MV3 (d = 0.39, [95% CI − 1.36 to − 0.16]) and MV4 (d = 0.28, [95% CI − 1.33 to − 0.14]). A non-parametric Mann–Whitney test was performed for MV5 and MV6. A significant difference was found for MV6 (U = 150.00, exact sig. two tailed = 0.012) but not for MV5 (U = 199.50, exact sig. two tailed = 0.237). To investigate the direction and extent of the relation, MV1 to MV4 and MV6 were correlated with each MV and parity group. A moderate-to-strong statistically significant correlation was found between all MVs and parity. Furthermore, strong-to-very strong correlations were observed between MV1, MV2, MV3 and MV4. MV6 was moderately correlated with MV1, MV2 and MV5, but not significantly correlated to the other two vectors. Details of the correlations are shown in Table 2. Many weak, non-significant correlations were observed between the MVs and possible confounding or effect-modifying variables (age, BMI, gestational age, days postpartum at the moment of ultrasound performance and newborn birthweight). History of the delivery mode and overall mode of delivery showed a moderate-to-strong negative correlation of r(22) = − 0.454 (p = 0.026) and (r(22) = − 0.553, p = 0.005), respectively, with MV6 in the multiparous group. However, these parameters were also strongly correlated with each other (r(22) = 0.59, p = 0.002). The other delivery mode parameters were run in the entire research population, as well as in the multiparous group, but were found to be weak and statistically non-significant for both overall and current delivery modes. In the entire study population, ‘current grade of perineal defect’ was moderately negatively correlated to MV1 (r(44) = − 0.475 p < 0.001), MV2 (r(44) = − 0.475 p < 0.001) and MV6 (r(44) = − 0.322, p = 0.029). Logically, the same tendency was observed for the ‘overall highest grade of perineal defect’, considering its very strong correlation to the ‘current grade of perineal defect’ (r(44) = 0.926, p < 0.001). When further differentiated, MV1 and MV2 were significantly negatively correlated with episiotomy (MV1: r(44) = − 0.415, p = 0.004; MV2: r(44) = − 0.370, p = 0.011) but not with ASI at current delivery. Finally, a univariate generalised linear regression analysis was performed for MV1–4 and 6. Parity predicted the difference of 26% in MV1 (R2 = 0.26, F(1,44) = 15.1, p < 0.001), 24% in MV2 (R2 = 0.24, F(1,44) = 14.1, p < 0.001), 13% in MV3 (R2 = 0.13, F(1,44) = 6.8, p = 0.013), 13% in MV4 (R2 = 0.13, F(1,44) = 6,27, p = 0.016) and 12% in MV6 (R2 = 0.12, F(1,44) = 6.2, p = 0.017). When the current grade of perineal defect was added to the regression model, the adjusted R2 for MV1 was 0.29 (F(2,43) = 10.2, p < 0.001). The regression model for MV2 was found to be the most predictive when the overall highest grade of perineal defect was added (R2 = 0.29, F(2,43) = 10.2, p < 0.001). There was no added predictive value of the current or overall highest grade of perineal defect for MV6.
Discussion
In this descriptive prospective cohort study, a significant difference between primiparous and multiparous women was demonstrated for all MVs of UMP, except for MV5. This is consistent with our hypothesis. The greatest effect of parity on urethral mobility was observed in MV1 and MV2. These results are remarkable, since there is no consensus in the literature on the association of parity and proximal urethral mobility, as different studies have contradicting results [8, 16,17,18,19,20]. Furthermore, this study found that parity predicts up to 26% of urethral mobility. The proximal segments were almost perfectly correlated with each other and strongly correlated with mid-urethral segments. MV6, however, was weak-to-moderately correlated with other MVs. More research is necessary to assess the additional value of UMP compared to bladder neck mobility and the clinical significance of the mobility of the distal urethra. According to the literature, increased bladder neck mobility is associated with a higher incidence of SUI [21]. This study showed that multiparous women have greater mobility in proximal urethral segments. Therefore, this group theoretically has an increased risk for SUI development. Above all studied confounders, the negative correlation between the current grade of perineal defect, particularly episiotomy, and MV1, MV2 and MV6 was striking. Thus, the following two hypotheses can be formed. First, the presence of perineal rupture or episiotomy can protect the anterior compartment from further damage. Second, discomfort can limit the maximal Valsalva manoeuvre of participants with perineal defects. These hypotheses require further research. A limitation of this study is that the desired sample size of 114 participants was not achieved due to the shortening of the foreseen recruitment time following COVID-19 restrictions. Therefore, the statistical power was limited and differentiation in subgroups, such as multiparity or delivery mode, was restricted. In addition, there is a possibility of sampling bias and reduced applicability to the general population: the study population was largely Caucasian, the participants were recruited at a tertiary clinic and the researchers were reluctant to approach women with a traumatic birth experience or child loss. One of the strengths of this study is that it is the first to compare the UMP of primiparous and multiparous women immediately postpartum. Moreover, the method proposed to measure and calculate the UMP is accessible, requiring no 3D or 4D applications or specialised software. This offers an opportunity for further research with a larger sample size.
In summary, to the best of the authors’ knowledge, this is the first study to assess the UMP of primiparous and multiparous women on TLUS immediately postpartum. The study found a significant difference between primiparous and multiparous women for 5 out of 6 MVs. Therefore, the association between multiparity and bladder neck mobility suggested by previous research can now be extended to the entire urethra [8, 17]. However, more research is needed on the impact of distinct parity grades, superiority of the UMP compared to bladder neck mobility, association of UMP and SUI symptoms and clinical significance of MV6.
Data availability
The blinded data that support the findings of this study are available from the corresponding author, DD, upon request.
Abbreviations
- (O)ASI:
-
(Obstetric) Anal sphincter injury
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- ICC:
-
Intraclass correlation coefficient
- MV:
-
Mobility vector
- SUI:
-
Stress urinary incontinence
- TLUS:
-
Translabial ultrasound
- UMP:
-
Urethral motion profile
References
de Araujo CC, Coelho SA, Stahlschmidt P, Juliato CRT (2018) Does vaginal delivery cause more damage to the pelvic floor than cesarean section as determined by 3D ultrasound evaluation? A systematic review. Int Urogynecol J 29(5):639–645. https://doi.org/10.1007/s00192-018-3609-3
Luo D, Chen L, Yu X, Ma L, Chen W, Zhou N, Cai W (2017) Differences in urinary incontinence symptoms and pelvic floor structure changes during pregnancy between nulliparous and multiparous women. PeerJ 5:e3615. https://doi.org/10.7717/peerj.3615
Dietz HP, Steensma AB, Hastings R (2003) Three-dimensional ultrasound imaging of the pelvic floor: the effect of parturition on paravaginal support structures. Ultrasound Obstet Gynecol 21(6):589–595. https://doi.org/10.1002/uog.100
Hunskaar S, Arnold EP, Burgio K, Diokno AC, Herzog AR, Mallett VT (2000) Epidemiology and natural history of urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 11(5):301–319. https://doi.org/10.1007/s001920070021
Dietz HP (2016) Pelvic floor ultrasound -atlas and textbook. Creative commons Attribution-Noncommercial-NoDerivatives 4.0.6.
Shek KL, Dietz HP (2008) The urethral motion profile: a novel method to evaluate urethral support and mobility. Aust N Z J Obstet Gynaecol 48(3):337–342. https://doi.org/10.1111/j.1479-828X.2008.00877.x
Wen L, Shek KL, Dietz HP (2019) Changes in urethral mobility and configuration after prolapse repair. Ultrasound Obstet Gynecol 53(1):124–128. https://doi.org/10.1002/uog.19165
Dickie KJ, Shek KL, Dietz HP (2010) The relationship between urethral mobility and parity. BJOG 117(10):1220–1224. https://doi.org/10.1111/j.1471-0528.2010.02649.x
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, Initiative S (2014) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg 12(12):1495–1499. https://doi.org/10.1016/j.ijsu.2014.07.013
Chan SS, Cheung RY, Yiu KW, Lee LL, Chung TK (2014) Pelvic floor biometry in Chinese primiparous women 1 year after delivery: a prospective observational study. Ultrasound Obstet Gynecol 43(4):466–474. https://doi.org/10.1002/uog.13249
Danforth KN, Townsend MK, Lifford K, Curhan GC, Resnick NM, Grodstein F (2006) Risk factors for urinary incontinence among middle-aged women. Am J Obstet Gynecol 194(2):339–345. https://doi.org/10.1016/j.ajog.2005.07.051
MacLennan AH, Taylor AW, Wilson DH, Wilson D (2000) The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. BJOG 107(12):1460–1470. https://doi.org/10.1111/j.1471-0528.2000.tb11669.x
OS X (2019) Horos In. (Version 3.3.6) https://horosproject.org
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15(2):155–163. https://doi.org/10.1016/j.jcm.2016.02.012
Harvey M-A, Pierce M, Walter J-E, Chou Q, Diamond P, Epp A, Thakar R (2015) Obstetrical anal sphincter injuries (OASIS): prevention, recognition, and repair. J Obstet Gynaecol Can 37(12):1131–1148. https://doi.org/10.1016/S1701-2163(16)30081-0
Peschers U, Schaer G, Anthuber C, Delancey JOL, Schuessler B (1996) Changes in vesical neck mobility following vaginal delivery [Article]. Obstet Gynecol 88(6):1001–1006. https://doi.org/10.1016/S0029-7844(96)00338-9
Meyer S, De Grandi P, Schreyer A, Caccia G (1996) The assessment of bladder neck position and mobility in continent nullipara, mulitpara, forceps-delivered and incontinent women using perineal ultrasound: a future office procedure? [Article]. Int Urogynecol J 7(3):138–146. https://doi.org/10.1007/BF01894202
Horak TA, Guzman-Rojas RA, Shek KL, Dietz HP (2014) Pelvic floor trauma: does the second baby matter? [Article]. Ultrasound Obst Gynecol 44(1):90–94. https://doi.org/10.1002/uog.13252
Jundt K, Scheer I, Von Bodungen V, Krumbachner F, Friese K, Peschers UM (2010) What harm does a second delivery to the pelvic floor? [Article]. Eur J Med Res 15(8):362–366. https://doi.org/10.1186/2047-783X-15-8-362
Chan SSC, Cheung RYK, Lee LL, Chung TKH (2018) Longitudinal pelvic floor biometry: which factors affect it? [Article]. Ultrasound Obstet Gynecol 51(2):246–252. https://doi.org/10.1002/uog.17446
Horosz E, Pomian A, Zwierzchowska A, Lisik W, Majkusiak W, Tomasik P, Barcz E (2020) Epidemiological features of the bladder neck rest position and mobility. J Clin Med. https://doi.org/10.3390/jcm9082413
Acknowledgements
This research received no funding or grants. There were no conflicts of interests.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
NM: project development, data collection, manuscript writing, data analysis. TL: project development, data collection, manuscript writing, data analysis. DD: project development, data collection, manuscript writing. YJ: supervision, review of results. HN: supervision, review of results.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of University of Antwerp.
Consent to participate
Written informed consent was obtained from all individual participants included in the study.
Consent for publication
The authors affirm that participants provided informed consent for publication of the image in Fig. 1.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maes, N., Lakerveld, T., Dekelver, D. et al. Relationship between urethral motion profile and parity assessed by translabial ultrasound imaging. Arch Gynecol Obstet 307, 1833–1838 (2023). https://doi.org/10.1007/s00404-022-06897-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06897-3