Abstract
Purpose
To evaluate the risk of miscarriage in IVF cycles in women with PCOS.
Methods
Systematic review and meta-analysis. Systematic search of MEDLINE, EMBASE and Google Scholar. The language search was restricted to English, Spanish and French, from 2000 to 2019, with crosschecking of references from relevant articles. Inclusion criteria were: (1) IVF cycles (2) a group of patients with PCOS was considered separately, (3) the miscarriage rate was reported, (4) there was a control group, (5) definition of PCOS according the Rotterdam criteria. Exclusion criteria were been excluded from the meta-analysis: (1) publication prior to the year 2000, (2) animal studies, (3) reviews, (4) abstracts or conference papers, (5) letters, (6) case reports, (7) studies comparing different IVF techniques, (8) studies comparing groups with and without metformin or other treatments, (9) studies on induced abortions. Risk of bias was assessed by the Newcastle–Ottawa score (NOS). All the included studies had a low risk of bias (NOS scores ranging 7–8). The review protocol was registered in PROSPERO (CRD42020186713). Seventeen studies were included in the meta-analysis. There was a total of 10,472 pregnancies (2650 in PCOS and 7822 in controls) of which 1885 were miscarriages (682 in PCOS and 1203 in controls). We considered the miscarriage rate (MR), preclinical MR, early MR, and late MR.
Results
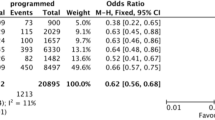
In IVF pregnancies the risk of miscarriage was significantly increased when considering miscarriages in total (RR = 1.59; CI = 1.45–1.75), preclinical miscarriages (RR = 1.59; CI = 1.35–1.88), and early miscarriages (RR = 1.44; CI = 1.16–1.79). The increased miscarriage rate persisted in Chinese and Western populations when considered separately. The risk of miscarriage was increased in the subgroup of fresh transfers (RR = 1.21; CI = 1.06–1.39) as well as in the subgroup including either fresh or frozen transfers (RR = 1.95; CI = 1.72–2.22).
Conclusion
PCOS is linked to an increased MR in IVF pregnancies both of miscarriages in total, and to an increase in preclinical and early miscarriages.
Prospero number
CRD42020186713.




Similar content being viewed by others
References
Teede H, Deeks A, Moran L (2010) Polycystic ovary syndrome: a complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Med 8:41
Azziz R, Carmina E, Chen Z, Dunaif A, Laven JS, Legro RS et al (2016) Polycystic ovary syndrome. Nat Rev Dis Primers 2:16057
Bellver J, Rodríguez-Tabernero L, Robles A, Muñoz E, Martínez F, Landeras J et al (2018) Polycystic ovary syndrome throughout a woman’s life. J Assist Reprod Genet 35:25–39
Azziz R, Carmina E, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Futterweit W et al (2006) Androgen Excess Society. Positions statement: criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: an Androgen Excess Society guideline. J Clin Endocrinol Metab 91:4237–4245
Qin JZ, Pang LH, Li MJ, Fan XJ, Huang RD, Chen HY (2013) Obstetric complications in women with polycystic ovary syndrome: a systematic review and meta-analysis. Reprod Biol Endocrinol 11:56
Palomba S, de Wilde MA, Falbo A, Koster MP, La Sala GB, Fauser BC (2015) Pregnancy complications in women with polycystic ovary syndrome. Hum Reprod Update 21:575–592
Homburg R, Armar NA, Eshel A, Adams J, Jacobs HS (1988) Influence of serum luteinising hormone concentrations on ovulation, conception, and early pregnancy loss in polycystic ovary syndrome. BMJ 297:1024–1026
Balen AH, Laven JS, Tan SL, Dewailly D (2003) Ultrasound assessment of the polycystic ovary: international consensus definitions. Hum Reprod Update 9:505–514
Boomsma CM, Eijkemans MJ, Hughes EG, Visser GH, Fauser BC, Macklon NS (2006) A meta-analysis of pregnancy outcomes in women with polycystic ovary syndrome. Hum Reprod Update 12:673–683
Heijnen EMEW, Eijkemans MJC, Hughes EG, Laven JSE, Macklon NS, Fauser BCJM (2006) A meta-analysis of outcomes of conventional IVF in women with polycystic ovary syndrome. Hum Reprod Update 12:13–21
Kjerulff LE, Sanchez-Ramos L, Duffy D (2011) Pregnancy outcomes in women with polycystic ovary syndrome: a metaanalysis. Am J Obstet Gynecol 204(558):e1-6
Yu HF, Chen HS, Rao DP, Gong J (2016) Association between polycystic ovary syndrome and the risk of pregnancy complications: a PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore) 95:e4863
Bahri Khomami M, Joham AE, Boyle JA, Piltonen T, Silagy M, Arora C et al (2019) Increased maternal pregnancy complications in polycystic ovary syndrome appear to be independent of obesity—a systematic review, meta-analysis, and meta-regression. Obes Rev 20:659–674
Sha T, Wang X, Cheng W, Yan Y (2019) A meta-analysis of pregnancy-related outcomes and complications in women with polycystic ovary syndrome undergoing IVF. Reprod Biomed Online 39:281–293
Kalra SK, Ratcliffe SJ, Dokras A (2013) Is the fertile window extended in women with polycystic ovary syndrome? Utilizing the Society for Assisted Reproductive Technology registry to assess the impact of reproductive aging on live-birth rate. Fertil Steril 100:208–213
Palomba S, Daolio J, La Sala GB (2017) Oocyte competence in women with polycystic ovary syndrome. Trends Endocrinol Metab 28:186–198
Palomba S, Piltonen TT, Giudice LC (2021) Endometrial function in women with polycystic ovary syndrome: a comprehensive review. Hum Reprod Update 27:584–618
Kolte AM, Bernardi LA, Christiansen OB, Quenby S, Farquharson RG, Goddijn M et al (2015) ESHRE Special Interest Group, Early Pregnancy. Terminology for pregnancy loss prior to viability: a consensus statement from the ESHRE early pregnancy special interest group. Hum Reprod 30:495–498
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group (2004) Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome+e. Fertil Steril 81:19–25
Johnson T, Kaplan L, Ouyang P, Rizza P.National institutes of health evidence-based methodology workshop on polycystic ovary syndrome. Nih ebmw reports. Bethesda, md: National institutes of health. 2019; 1 (2012; Executive summary. Available at: https://prevention.nih.gov/docs/programs/pcos/FinalReport.pdf. 1–14): 1–14
Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L et al (2018) International PCOS Network. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod 33:1602–1618
Bender-Atik R, Christiansen OB, Elson J, Kolte AM, Lewis S, Middeldorp S et al (2018) ESHRE Guideline Group on RPL, ESHRE guideline: recurrent pregnancy loss. Hum Reprod Open 2018(2):hoy004. https://doi.org/10.1093/hropen/hoy00
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Plos Med 2009;6:e1000097. http://prismastatement.org/PRISMAStatement. Accessed 26 Apr 2021
Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S (2014) PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res 14:579
Lo CK, Mertz D, Loeb M (2014) Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol 14:45
Palomba S, Falbo A, Daolio J, Battaglia FA, Sala GB (2018) Pregnancy complications in infertile patients with polycystic ovary syndrome: updated evidence. Minerva Ginecol 70:754–760
Wang Y, Gu X, Tao L, Zhao Y (2016) Co-morbidity of cervical incompetence with polycystic ovarian syndrome (PCOS) negatively impacts prognosis: a retrospective analysis of 178 patients. BMC Pregnancy Childbirth 16:308
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analysis. 2011. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 26 Apr 2021
Wang Q, Luo L, Lei Q, Lin M, Huang X, Chen M et al (2016) Low aneuploidy rate in early pregnancy loss abortuses from patients with polycystic ovary syndrome. Reprod Biomed Online 33:85–92
Sterling L, Liu J, Okun N, Sakhuja A, Sierra S, Greenblatt E (2016) Pregnancy outcomes in women with polycystic ovary syndrome undergoing in vitro fertilization. Fertil Steril 105:791–797
Liu L, Tong X, Jiang L, Li TC, Zhou F, Zhang S (2014) A comparison of the miscarriage rate between women with and without polycystic ovarian syndrome undergoing IVF treatment. Eur J Obstet Gynecol Reprod Biol 176:178–182
Rehman R, Mehmood M, Ali R, Shaharyar S, Alam F (2018) Influence of body mass index and polycystic ovarian syndrome on ICSI/IVF treatment outcomes: a study conducted in Pakistani women. Int J Reprod Biomed 16:529–534
Huang Q, Niu Y, Xu L, Chen B, Zhang Y, Song LJ et al (2018) Relationship between a low ratio of serum estradiol to follicle number and fertility treatment outcomes: a retrospective cohort study of 516 cases. Medicine (Baltimore) 97:e12017
Kdous M, Chaker A, Zhioua A, Zhioua F (2009) Oocyte and embryo quality and outcome of ICSI cycles in patients with polycystic ovary syndrome (PCOS) versus normo-ovulatory. J Gynecol Obstet Biol Reprod 38:133–143 (French)
Luo L, Gu F, Jie H, Ding C, Zhao Q, Wang Q et al (2017) Early miscarriage rate in lean polycystic ovary syndrome women after euploid embryo transfer—a matched-pair study. Reprod Biomed Online 35:576–582
Sahu B, Ozturk O, Ranierri M, Serhal P (2008) Comparison of oocyte quality and intracytoplasmic sperm injection outcome in women with isolated polycystic ovaries or polycystic ovarian syndrome. Arch Gynecol Obstet 277:239–244
Khrouf M, Kdous M, Bouyahia M, Chaker A, Zhioua F, Zhioua A (2010) Clinicals and biological aspects of ICSI cycles on patients with polycystic ovary syndrome. Tunis Med 88:152–157 (French)
Han AR, Kim HO, Cha SW, Park CW, Kim JY, Yang KM et al (2011) Adverse pregnancy outcomes with assisted reproductive technology in non-obese women with polycystic ovary syndrome: a case-control study. Clin Exp Reprod Med 38:103–108
Nejad ES, Saedi T, Saedi S, Rashidi BH, Nekoo ZA, Jahangiri N (2011) Comparison of in vitro fertilisation success in patients with polycystic ovary syndrome and tubal factor. Gynecol Endocrinol 27:117–120
Okohue JE, Onuh SO, Ikimalo JI (2013) Comparison of IVF/ICSI outcome in patients with polycystic ovarian syndrome or tubal factor infertility. Niger J Clin Pract 16:207–210
Li HWR, Lee VC, Lau EY, Yeung WS, Ho PC, Ng EH (2014) Cumulative live-birth rate in women with polycystic ovary syndrome or isolated polycystic ovaries undergoing in-vitro fertilisation treatment. J Assist Reprod Genet 31:205
Huang K, Liao X, Dong X, Zhang H (2014) Effect of overweight/obesity on IVF-ET outcomes in chinese patients with polycystic ovary syndrome. Int J Clin Exper Med 7:5872–5876
Zhang CM, Zhao Y, Li R, Yu Y, Yan LY, Li L et al (2014) Metabolic heterogeneity of follicular amino acids in polycystic ovary syndrome is affected by obesity and related to pregnancy outcome. BMC Pregnancy Childbirth 14:11
Rees DA, Jenkins-Jones S, Morgan CL (2016) Contemporary reproductive outcomes for patients with polycystic ovary syndrome: a retrospective observational study. J Clin Endocrinol Metab 101:1664–1672
Hwang Y, Cha S, Song I, Yang K, Min E, Kim H (2016) Fertility of patients with polycystic ovary syndrome undergoing in vitro fertilization by age. Int J Gynecol Obstet 135:91–95
Li XL, Huang R, Fang C, Wang YF, Liang XY (2018) Logistic regression analysis of risk factors associated with spontaneous abortion after in vitro fertilization/intracytoplasmic sperm injection-embryo transfer in polycystic ovary syndrome patients. Reprod Dev Med 2:105–110
Goldstein SR (1994) Embryonic death in early pregnancy: a new look at the first trimester. Obstet Gynecol 84:294–297
Edmonds DK, Lindsay KS, Miller JF, Williamson E, Wood PJ (1982) Early embryonic mortality in women. Fertil Steril 38:447–453
Gomez R, Hafezi N, Amrani M, Schweiger S, Dewenter MK, Thomas P, Lieb C, Hasenburg A, Skala C (2021) Genetic findings in miscarriages and their relation to the number of previous miscarriages. Arch Gynecol Obstet 303:1425–1432
Wang X, Chen C, Wang L, Chen D, Guang W, French J (2003) Conception, early pregnancy loss, and time to clinical pregnancy: a population-based prospective study. Fertil Steril 79:577–584
Wilcox AJ, Weinberg CR, O’Connor JF, Baird DD, Schlatterer JP, Canfield RE et al (1988) Incidence of early loss of pregnancy. N Engl J Med 319:189–194
Diaz-Nuñez M, Rabanal A, Exposito A, Ferrando M, Quintana F, Soria JM et al (2019) Recurrent miscarriage and implantation failure of unknown cause studied by a panel of thrombophilia conditions: increased frequency of FXIII Val34Leu polymorphism. J Reprod Infertil 20:76–82
Açbay O, Gündoğdu S (1996) Can metformin reduce insulin resistance in polycystic ovary syndrome? Fertil Steril 65:946–949
Ehrmann DA, Cavaghan MK, Imperial J, Sturis J, Rosenfield RL, Polonsky KS (1997) Effects of metformin on insulin secretion, insulin action, and ovarian steroidogenesis in women with polycystic ovary syndrome. J Clin Endocrinol Metab 82:524–530
Kelestimur F, Unluhizarci K, Bayram F, Sahin Y, Tutus A (2000) Metformin and polycystic ovary syndrome. Clin Endocrinol (Oxf) 52:244–246
Olivennes F, Cunha-Filho JS, Fanchin R, Bouchard P, Frydman R (2002) The use of GnRH antagonists in ovarian stimulation. Hum Reprod Update 8:279–290
Ron-El R, Raziel A, Schachter M, Strassburger D, Kasterstein E, Friedler S (2000) Induction of ovulation after gnRH antagonists. Hum Reprod Update 6:318–321
Glujovsky D, Farquhar C, Quinteiro Retamar AM, Alvarez Sedo CR, Blake D (2016) Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology. Cochrane Database Syst Rev 6:CD002118. https://doi.org/10.1002/14651858.CD002118.pub5
Matorras R, Pijoan JI, Perez-Ruiz I, Lainz L, Malaina I, Borjaba S (2021) Meta-analysis of the embryo freezing-transfer interval. Reprod Med Biol 20:144–158
Wang S, Alvero R (2013) Racial and ethnic differences in physiology and clinical symptoms of polycystic ovary syndrome. Semin Reprod Med 31:365–369
Zhao Y, Qiao J (2013) Ethnic differences in the phenotypic expression of polycystic ovary syndrome. Steroids 78:755–760
Butler AE, Abouseif A, Dargham SR, Sathyapalan T, Atkin SL (2020) Metabolic comparison of polycystic ovarian syndrome and control women in Middle Eastern and UK Caucasian populations. Sci Rep 10:18895
Burgart JM (2021) Clinical obstetrics & gynecology: polycystic ovary disease ethnicity, diversity, and psychosocial ramifications. Clin Obstet Gynecol 64:76–82
Ghaffari F, Chekini Z, Vesali S (2022) Duration of estradiol supplementation in luteal phase support for frozen embryo transfer in hormone replacement treatment cycles: a randomized, controlled phase III trial. Arch Gynecol Obstet 305:767–777
Chen ZJ, Shi Y, Sun Y, Zhang B, Liang X, Cao Y et al (2016) Fresh versus frozen embryos for infertility in the polycystic ovary syndrome. N Engl J Med 375:523–533
Vuong LN, Dang VQ, Ho TM, Huynh BG, Ha DT, Pham TD et al (2018) IVF transfer of fresh or frozen embryos in women without polycystic ovaries. N Engl J Med 378:137–147
Fedorcsak P, Dale PO, Storeng R, Tanbo T, Abyholm T (2001) The impact of obesity and insulin resistance on the outcome of IVF or ICSI in women with polycystic ovarian syndrome. Hum Reprod 16:1086–1091
Bellver J, Rossal LP, Bosch E, Zuniga A, Corona JT, Melendez F et al (2003) Obesity and the risk of spontaneous abortion after oocyte donation. Fertil Steril 79:1136–1140
Ke RW (2014) Endocrine basis for recurrent pregnancy loss. Obstet Gynecol Clin North Am 41:103–112
Homburg R (2006) Pregnancy complications in PCOS. Best Pract Res Clin Endocrinol Metab 20:281–292
Zhang Y, Zhao W, Xu H, Hu M, Guo X, Jia W et al (2019) Hyperandrogenism and insulin resistance-induced fetal loss: evidence for placental mitochondrial abnormalities and elevated reactive oxygen species production in pregnant rats that mimic the clinical features of polycystic ovary syndrome. J Physiol 597:3927–3950
Palomba S, Falbo A, Russo T, Tolino A, Orio F, Zullo F (2010) Pregnancy in women with polycystic ovary syndrome: the effect of different phenotypes and features on obstetric and neonatal outcomes. Fertil Steril 94:1805–1811
Palomba S (2021) Is fertility reduced in ovulatory women with polycystic ovary syndrome? An opinion paper. Hum Reprod 18(36):2421–2428
Kelley AS, Smith YR, Padmanabhan V (2019) A narrative review of placental contribution to adverse pregnancy outcomes in women with polycystic ovary syndrome. J Clin Endocrinol Metab 104:5299–5315
Leary C, Leese HG, Sturmey RG (2015) Human embryos from overweight and obese women display phenotypic and metabolic abnormalities. Hum Reprod 30:122–132
Matorras R, Exposito A, Ferrando M, Mendoza R, Larreategui Z, Laínz L et al (2020) Oocytes of women who are obese or overweight have lower levels of n-3 polyunsaturated fatty acids compared with oocytes of women with normal weight. Fertil Steril 113:53–61
Patel SS, Carr BR (2008) Oocyte quality in adult polycystic ovary syndrome. Semin Reprod Med 26:196–203
Cano F, García-Velasco JA, Millet A, Remohí J, Simón C, Pellicer A (1997) Oocyte quality in polycystic ovaries revisited: identification of a particular subgroup of women. J Assist Reprod Genet 14:254–261
Wissing ML, Bjerge MR, Olesen AI, Hoest T, Mikkelsen AL (2014) Impact of PCOS on early embryo cleavage kinetics. Reprod Biomed Online 28:508–514
Papanikolaou EG, Tournaye H, Verpoest W, Camus M, Vernaeve V, Van Steirteghem A et al (2005) Early and late ovarian hyperstimulation syndrome: early pregnancy outcome and profile. Hum Reprod 20:636–641
Frick AP (2021) Advanced maternal age and adverse pregnancy outcomes. Best Pract Res Clin Obstet Gynaecol 70:92–100. https://doi.org/10.1016/j.bpobgyn.2020.07.005
Best D, Avenell A, Bhattacharya S (2017) How effective are weight-loss interventions for improving fertility in women and men who are overweight or obese? A systematic review and meta-analysis of the evidence. Hum Reprod Update 23:681–705
Feng L, Lin XF, Wan ZH, Hu D, Du YK (2015) Efficacy of metformin on pregnancy complications in women with polycystic ovary syndrome: a meta-analysis. Gynecol Endocrinol 31:833–839
Author information
Authors and Affiliations
Contributions
MR and MD conceived the study design. MD made the systematic review of literature. MD, SH, DNM and LL performed data extraction. MD performed data processing. PJI and PFS performed the meta-analysis. MR wrote the article. All authors approved the final article.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
404_2022_6757_MOESM2_ESM.pdf
Supplemmentary figure 2. Total miscarriages in IVF pregnancies and ethnic background. A. Miscarriage rate in IVF pregnancies in China. B. Miscarriage rate in IVF pregnancies in Western Countries. C. Miscarriage rate in IVF pregnancies in South Korea. D. Miscarriage rate in IVF pregnancies in Tunisia. (PDF 337 KB)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Matorras, R., Pijoan, J.I., Laínz, L. et al. Polycystic ovarian syndrome and miscarriage in IVF: systematic revision of the literature and meta-analysis. Arch Gynecol Obstet 308, 363–377 (2023). https://doi.org/10.1007/s00404-022-06757-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06757-0