Abstract
Purpose
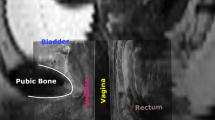
To explore 3D morphological changes of the bladder, urethra, and vagina following different numbers of vaginal deliveries.
Methods
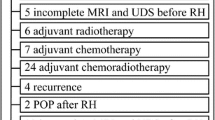
Sampled patients had undergone magnetic resonance imaging for gynecological diseases in Nanfang Hospital. A total of 167 patients who met the study inclusion and exclusion criteria were enrolled and divided into four groups. Mimics and UG software packages were used for reconstructions and measurements, and data were compared with one-way analyses of variance.
Results
A total of 167 3D models were constructed, and eight parameters related to the bladder and urethra were measured (5 angles, 2 lengths, and 1 thickness). No statistically significant differences were found between subgroups, although mean plot figures of urethra pubic and α angles showed trends to increase with more deliveries, and the opposite trend was seen for the urethra tilt angle. There were no obvious trends between other parameters and delivery number. There were seven vaginal parameters (6 lengths and 1 shape). Mid-urethral and vaginal gap measurements tended to become wider as delivery number increased, and the opposite was seen for the distal gap. Mid-vaginal 2D cross-sectional shape and the proportion of shallow concave types also tended to significantly increase with more deliveries, especially after the third birth.
Conclusion
As the number of deliveries through the vagina increases, the lateral support function of this organ and the urethra become relatively weaker. These fine anatomical changes are related to delivery numbers and become most obvious after the third birth.







Similar content being viewed by others
Data availability
All of our data and material can be open and availability.
Code availability
510,515.
References
Nygaard I, Barber MD, Burgio KL et al (2008) Prevalence of symptomatic pelvic floor disorders in US women. JAMA 300:1311–1316
Sung VW, Washington B, Raker CA (2010) Costs of ambulatory care related to pelvic floor disorders in the United States. Am J Obstet Gynecol 202:483.e1–4
Åkervall S, Al-Mukhtar Othman J, Molin M, Gyhagen M (2019) Symptomatic pelvic organ prolapse in middle-aged women - a national matched cohort study on the influence of childbirth [published online ahead of print, 2019 Oct 19]. Am J Obstet Gynecol S0002–9378(19)31224–4.
Grant A, Currie S (2020) Qualitative exploration of the acceptability of a postnatal pelvic floor muscle training intervention to prevent urinary incontinence. BMC Womens Health 20(1):9
Swenson CW, Masteling M, DeLancey JO, Nandikanti L, Schmidt P, Chen L (2019) Aging effects on pelvic floor support: a pilot study comparing young versus older nulliparous women [published online ahead of print, 2019 Aug 6]. Int Urogynecol J https://doi.org/10.1007/s00192-019-04063-z.
Petros PE, Ulmsten UI (1990) An integral theory of female urinary incontinence: experimental and clinical considerations. Acta Obstet Gynecol Scand 69(153):7–31
DeLancey JO (1994) Structural support of the urethra as it relates to stress urinary incontinence: the hammock hypothesis. Am J Obstet Gynecol 170(6):1713–1723
Kamisan AI, Gerges B, Shek KL et al (2015) The association between vaginal parity and hiatal dimensions: a retrospective observational study in a tertiary urogynaecological centre. BJOG 122(6):867–872
Walker GA, Prasanna G (2011) Pelvic organ prolapse and incontinence in developing countries review of prevalence and risk factors. Int Urogynecol J 22(2):127–135
Chen J, Chen C, Li Y, Chen L, Xu J, Liu P (2018) Impact of radical hysterectomy on the transobturator sling pathway: a retrospective three-dimensional magnetic resonance imaging study. Int Urogynecol J 29(9):1359–1366
Li P, Liu P, Chen C, Duan H, Qiao W, Ognami OH (2018) The 3D reconstructions of female pelvic autonomic nerves and their related organs based on MRI: a first step towards neuronavigation during nerve-sparing radical hysterectomy. Eur Radiol 28(11):4561–4569
Sze EH, Sherard GB 3rd, Dolezal JM (2002) Pregnancy, labor, delivery, and pelvic organ prolapse. Obstet Gynecol 100:981–986
Elenskaia K, Thakar R, Sultan AH, Scheer I, Onwude J (2013) Effect of childbirth on pelvic organ support and quality of life: a longitudinal cohort study. Int Urogynaecol J 24:927–937
Gyhagen M, Bullarbo M, Nielsen TF, Milsom I (2012) Prevalence and risk factors for pelvic organ prolapse 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG 120(2):152–160
Leijonhufvud A, Lundholm C, Cnattingius S et al (2011) Risks of stress urinary incontinence and pelvic organ prolapse surgery in relation to mode of childbirth. Am J Obstet Gynecol 204(1):70.e1–7
Bozkun M, Yumru AE, Sahin L (2014) Pelvic-floor dysfunction and effects of pregnancy and mode of delivery on pelvic floor. Taiwan J Obstet Gynecol 53(4):452–458
Rørtveit G, Hannestad YS (2014) Association between mode of delivery and pelvic floor dysfunction. Tidsskr Nor Laegeforen 134(19):1848–1852
Serati M, Salvatore S, Khullar V et al (2008) Prospective study to assess risk factors for pelvic ticker dysfunction after delivery. Acta Obstet Gynecol Stand 87(3):313–318
Lipsehuetz M, Cohen SM, Liebergall-Wischnitzer M et al (2015) Degree of bother from pelvic floor dysfunction in women one year after first delivery. Eur J Obstet Gynecol Reprod Biol 191:90–94
Patel DA, Xu X, Thomason AD et al (2006) Childbirth and pelvic floor dysfunction: an epidemiologic approach to the assessment of prevention opportunities at delivery. Am J Obstet Gynecol 195(1):23–28
Bump RC, Mattiasson A, Bø K et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 5(1):10–17
Kepenekci I, Keskinkilic B, Akinsu F et al (2011) Prevalence of pelvic floor disorders in the female population and the impact of age, mode of delivery, and parity. Dis Colon Rectum 54(1):85–94
Quiroz LH, Pickett SD, Peck JD et al (2017) Increasing age is a risk factor for decreased postpartum pelvic floor strength. Female Pelvic Med Reconstr Surg 23(2):136–140
Zhao Y, Zou L, Xiao M et al (2018) Effect of different delivery modes on the short-term strength of the pelvic floor muscle in Chinese primipara. BMC Pregnancy Childbirth 18(1):275
Chan SSC, Cheung RYK, Lee LL, Chung TKH (2018) Longitudinal pelvic floor biometry: which factors affect it? Ultrasound Obstet Gynecol 51(2):246–252
Leijonhufvud A, Lundholm C, Cnattingius S et al (2012) Risk of surgically managed pelvic floor dysfunction in relation to age at first delivery. Am J Obstet Gynecol 207(4):303.e1–7
Dietz H, Wilson P (1999) The influence of bladder volume on the position and mobility of the urethrovesical junction. Int Urogynecol J Pelvic Floor Dysfunct 10(1):3–6
Murad-Regadas SM, Bezerra LR, Silveira CR et al (2013) Anatomical and functional characteristics of the pelvic floor in nulliparous women submitted to three-dimensional endovaginal ultrasonography: case control study and evaluation of interobserver agreement. Rev Bras Ginecol Obstet 35(3):123–129
Siafarikas F, Staer Jensen J, Hilde G, Bø K, Engh ME (2015) The levator ani muscle during pregnancy and major levator ani defects diagnosed postpartum: a three and four-dimensional ultrasound study. BJOG 122(8):1083–1091
Fritsch H, Pinggera GM, Lienemann A, Mitterberger M, Bartsch G, Strasser H (2006) What are the supportive structures of the female urethra? Neurourol Urodyn 25(2):128–134
Larson KA, Luo J, Guire KE, Chen L, Ashton-Miller JA, DeLancey JO (2012) 3D analysis of cystoceles using magnetic resonance imaging assessing midline, paravaginal, and apical defects. Int Urogynecol J 23(3):285–293
Acknowledgements
We thank An Shenli for kindly providing statistical advice. We also thank the Imaging Center of Nanfang Hospital for patient scanning and data collection.
Funding
Funding was provided by the National Natural Science Foundation of China, which covered our research fees (Projects 81272585 and 81571422).
Author information
Authors and Affiliations
Contributions
CC and LP contributed to the conception and design of this study and also contributed to patient information collection. CL contributed to data collection, 3D reconstruction and measurement, statistical analysis, and paper writing and revising. FJ contributed to MRI scanning and image identification. TL and PC contributed to reconstruction work of 3D models. CXJ contributed to 3D reconstruction and measurement.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. On behalf of all authors, the corresponding authors state that there is no conflict of interest.
Ethical approval
The retrospective study was approved by the Ethics Committee of Nanfang Hospital, Southern Medical University.
Consent for publication
We deeply appreciate your consideration of our manuscript, and we look forward to sending this manuscript for peer review, and if possible, we all consent for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, L., Chen, C., Feng, J. et al. Vaginal delivery effects on 3D morphology of the bladder, urethra, and vagina: a pilot study comparing women with different numbers of deliveries. Arch Gynecol Obstet 307, 473–480 (2023). https://doi.org/10.1007/s00404-022-06622-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06622-0