Abstract
Purpose
To evaluate the impact of endocervical and decidual polypectomy on obstetrical outcomes of pregnant women.
Methods
MEDLINE, Scopus, ClinicalTrials.gov, Scielo, EMBASE, Cochrane Library at the CENTRAL Register of Controlled Trials, and LILACS were searched from inception to April 2021. No language or geographical restrictions were applied. Inclusion criteria regarded observational studies concerning pregnant women with a cervical lesion who underwent cervical polypectomy. Co-primary outcomes were incidence of late pregnancy loss and preterm birth in women with endocervical or decidual polypectomy as well as polypectomy versus expectant management. Random effect meta-analyses to calculate risk ratio (RR) with 95% confidence interval (CI) were performed. Quality assessment of included papers was performed using Newcastle–Ottawa Scale criteria.
Results
Three studies, with data provided for 3097 women, were included in quantitative analysis, with comparisons between endocervical and decidual polyps extracted from two studies and 156 patients. After a first trimester endocervical or decidual polypectomy, no significant differences were found for late pregnancy losses (RR 0.29 [95% CI 0.05, 1.80], I2 = 11%). Risk for preterm birth was significantly higher for decidual polyps’ removal (RR 6.13 [95% CI 2.57, 14.59], I2 = 0%). One paper compared cervical polypectomy vs expectant management, with increased incidence of late pregnancy loss (4/142 vs 5/2799; p < 0.001) and preterm birth (19/142 vs 115/2799; p < 0.001) in women subjected to polypectomy.
Conclusions
Evidence regarding the removal of cervical polyps in pregnancy is extremely limited. However, the removal of either decidual or endocervical polyps seems associated with increased risk of pregnancy loss and preterm birth, with increased preterm birth risk following endocervical rather than decidual polypectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical polyps are a common cause of genital bleeding and vaginal discharge [1]. Their presence is also related to an increased risk of cervicitis and pelvic inflammatory disease due to chronic inflammation [2]. When they are discovered in non-pregnant women, their removal is a feasible way to reduce complaints and abnormal bleeding [3]. It can be done using in-office hysteroscopy without anesthesia with little-to-no discomfort for the patient or by twisting the lesion with forceps [4,5,6,7,8]. Moreover, endocervical lesions should be sent to histopathological analysis for confirming the benignity of the pathology [9,10,11].
Cervical polyps can be also discovered during pregnancy; they may provoke recurrent bleeding and infection in every phase of the pregnancy, increasing the risk of chorioamnionitis [12, 13]. Moreover, under the influence of pregnancy-related hormones, their size notably increases, with the possibility of a significant protrusion of the lesion toward the external cervical os [14]. For this reason, it can act as a physical obstacle during labor and increase the risk of active bleeding [14].
The role of cervical polypectomy during pregnancy is still debated. It has been reported that the polypectomy during pregnancy significantly reduces the incidence of chorioamnionitis compared to women in which the polypectomy was delayed until delivery [12, 15]. Based on this scenario, some studies recommend the resection of cervical polyps for pregnant women with clinical symptoms (i.e., active genital bleeding or vaginal discharge). However, new evidence shows that cervical polypectomy itself could raise the risk of pregnancy loss and preterm delivery [16, 17].
Moreover, cervical polyps have various histopathological diagnoses. Endocervical polyps, the most common lesions, are hyperplastic protrusions of the endocervical mucosa [18]. During pregnancy, endocervical polyps may undergo a focal stromal pseudodecidualization, which leads the pathologist to commonly diagnose them as “decidual polyps” [2]. It is still unclear whether decidual and endocervical polyps should be treated as a common entity or have different scenarios on the symptoms and on the pursuance of pregnancy.
There are no clear guidelines on whether cervical polyps found during pregnancy should be removed. Subsequently, it currently remains vague whether cervical polyps during pregnancy should be considered a significant harm for late pregnancy loss or spontaneous preterm birth.
To clarify the state of evidence, the aim of this systematic review and meta-analysis was to investigate the impact of endocervical or decidual polypectomy performed during pregnancy on the risk of late pregnancy loss and preterm birth.
Materials and methods
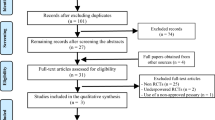
This meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) [19]. The protocol of the systematic review was structured a priori. It outlined strategies for screening the literature, including and examining articles, as well as data extraction, tabulation, integration, and analysis. Therefore, it was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database (CRD42021260847).
Study search
Seven electronic databases (MEDLINE, Scopus, ClinicalTrials.gov, Scielo, EMBASE, the Cochrane Library at the CENTRAL Register of Controlled Trials, and LILACS) were searched starting from their inception to April 2021. Search terms used were the following text words and Medical Subject Headings (MeSH): “cervical polyps” or “decidual polyps” or “cervical polypectomy” and “pregnancy (MeSH)”. Neither language nor geographic location limitations were adopted. In addition, we screened the reference lists of all eligible papers to retrieve potential studies not captured by electronic searches. The electronic search as well as the eligibility of the selected studies were assessed independently by two authors (G.R. and L.D.C.), while disagreement was solved by involving a third reviewer (P.D.F.).
Primary and secondary outcomes
Co-primary outcomes of this meta-analysis were the incidence of late pregnancy loss and preterm birth. Late pregnancy loss was defined as a spontaneous interruption of pregnancy occurred after the 12th week of gestational age. Preterm birth was defined as the birth of a living fetus before 37 weeks of gestational age.
Risk of bias
For studies with an observational design, the risk of bias was judged using the Newcastle–Ottawa Scale (NOS) criteria [20]. According to NOS, each study is evaluated on three broad elements: the selection of study groups, their comparability, as well as the ascertainment of the outcome of interest. Assessment of the selection of a study includes the following criteria: representativeness of the exposed cohort evaluation, non-exposed cohort selection, ascertainment of the exposure of the cohorts, and proof that outcome of interest was not likely to occur spontaneously at the beginning of the study. The comparability of studies is assessed including the evaluation of the comparability of cohorts based on the design or analysis. Moreover, the ascertainment of the outcome of interest is evaluated including the method of determining the outcome of interest, duration, and adequacy of follow-up. According to NOS, a study can be granted a maximum of one star for each numbered item within the Selection and Outcome categories. A maximum of two stars can be awarded for Comparability. Risk-of-bias assessment was independently assessed by three authors (M.L.V., P.G., and S.G.V.). Disagreement was resolved by discussion with a fourth reviewer (P.D.F.).
Statistical analysis
Two authors conducted the data analysis in an independent manner using Review Manager 5.3 (The Nordic Cochrane Centre 2014, Copenhagen, Denmark) and Stata 14.1 (Stata corp., College Station, TX, 2013).
The summary measures were reported as risk ratios (RR) with 95% of confidence interval (CI) using the random-effects model of Der Simonian and Laird. Higgins I-squared (I2) index was used to target between-studies heterogeneity. An I2 index higher than 0% was used to target potential heterogeneity with 25, 50, and 75% identified as cut-offs for low, moderate, and high heterogeneity [21]. The potential publication bias was evaluated by means of the Egger test. A p value < 0.05 was considered statistically significant.
Results
General characteristics
202 studies were originally identified through database search. Of those, seven were removed as duplicates. After title and abstract screening, 54 studies were removed as out-of-topic case-reports, out-of-topic conference abstracts (61 records) and review articles (24 records), letters/conference papers, or short survey (4 records) or out-of-topic original articles (45 records). Three studies, with data provided for 3097 women, were selected and included in meta-analysis [16, 22, 23] (Fig. 1). Of those, comparisons between endocervical and decidual polyps were retrieved from two studies [22, 23], with data provided for 156 patients. In addition, the above-mentioned studies were supplied by the qualitative analysis of two case-reports [2, 17] and two conference abstracts [24, 25]. Main characteristics of papers included in quantitative synthesis as well as inclusion and exclusion criteria are summarized in Table 1. All the studies were conducted in Japan and had a historical cohort design. One research compared the incidence of late pregnancy losses and preterm birth in women with and without cervical polyp diagnosed in pregnancy [16]. Two studies compared the risk for preterm birth and late pregnancy loss after removal of endocervical lesions in pregnancy [22, 23].
Quality characteristics and publication bias
Quality characteristics of included studies, reported by means of the NOS criteria, showed high ratings for all the papers regarding the selection and comparability of the study groups, as well as for ascertainment of the outcomes of interest (Supplementary Table 1).
Publication bias, evaluated by means of the Egger Test, was not apparent (p = 0.144).
Presence of a cervical lesion in first trimester
Hirayama et al. evaluated how the presence of an endocervical lesion (cervical or decidual polyp) might impact on the pregnancy [16]. Even adopting an expectant management, without the removal of the lesion, a cervical organic lesion was associated with poor obstetrical outcomes.
The polyp group showed a statistically significant higher incidence of pregnancy losses (4/142 vs 5/2799; p < 0.001) and preterm birth before 28 (3/142 vs 9/3799; p = 0.001), 34 (7/142 vs 22/2799; p < 0.001), and 37 (19/142 vs 115/2799; p < 0.001) weeks of pregnancy.
Differences between endocervical and decidual polyps
Two papers evaluated the risk for pregnancy loss after a first trimester endocervical or decidual polypectomy. No significant differences were found between the two groups (RR 0.29 [95% CI 0.05, 1.80], I2 = 11%) (Fig. 2).
The possibility of preterm birth before the 34th week of gestation was analyzed by the same two papers. The removal of a decidual polyp was associated with an increased risk if compared to an endocervical polyp resection (RR 6.13 [95% CI 2.57, 14.59], I2 = 0%) (Fig. 3).
Qualitative analysis of case-reports and conference abstracts
Two case-reports described experiences of cervical polypectomies during pregnancy and were included in qualitative analysis. Seo et al. described a single case of first trimester pregnancy loss after a diagnostic polypectomy in a woman with vaginal bleeding [2]. Aoki et al. showed that performing a cervical polypectomy with an Endoloop polydioxanone suture II (Ethicon Endo-Surgery, Germany) led to chorioamnionitis and subsequent premature rupture of membrane at 22 gestational weeks, with spontaneous delivery at 24 weeks and 6 days [17].
The purpose of this review was also discussed by two conference abstracts. Butt et al. showed that, in two primigravidae women, a conservative approach for an endocervical lesion, although with a complaint of first trimester heavy bleeding, is a successful approach to achieve a term delivery, with spontaneous resolution of the polyp after the delivery [24]. Conversely, Yoshida et al. described a case-series of 20 women with a diagnosis of decidual polyp who were managed conservatively. They reported a case of spontaneous pregnancy loss at 13 weeks of gestation, 13 cases of cervical cerclage due to shortened cervical length, and 2 cases of preterm birth before the 28th gestational week, showing the presence of adverse obstetric outcomes even with expectant management [25].
Discussion
This systematic review found that the presence of an endocervical or decidual polyp is a common risk factor for late pregnancy loss and preterm birth. In case of a cervical polypectomy, neoformations who received a histopathological diagnosis of decidual polyps exhibited an increased risk for preterm birth relative to endocervical mucosal polyps. The risk for late pregnancy loss was the same for decidual and endocervical polyps.
Hirayama et al. gave some insights about the reason for late pregnancy loss in women with and without an endocervical lesion [16]. In their cohorts, four out of five cases of late pregnancy losses in the non-polyp group were due to membrane rupture or fetal membrane prolapse, which all happened after the 20th of pregnancy. Conversely, in the polyp group, premature membrane rupture or acute genital bleeding was diagnosed before the 16th week of gestation, without neither cervical enlargement nor funneling or shortening of the cervix, resulting into earlier pregnancy loss in every patient. Pathological chorioamnionitis was found in all the histopathological samples of those pregnancy losses [14].
Based on this purpose, previous studies report two main causes that can be considered crucial in determining preterm birth. First, cervical polyps become the site of progressive ascending pelvic infection which leads to chorioamnionitis [26, 27]. Second, degeneration and necrosis of cervical polyps cause a considerable release of inflammatory cytokines which are expected to promote cervical ripening [2, 28].
According to that, Kanayama and Terao evaluated both the cervical granulocyte elastase activity and white blood cell count from the cervical mucus of mid-pregnancy women with and without cervical polyps [29]. They reported that both the parameters were significantly higher in women with cervical polyps and were reduced after the polypectomy. In addition, with the histopathological analysis of the placenta, they confirmed an association between cervical polyps and histological chorioamnionitis [29].
An additional concern, as mentioned by Hirayama et al. [16], is that in the majority of women that were conservatively managed, cervical polyps were referred to be spontaneously regressed by the first half of the pregnancy, since they were no longer visible from the external uterine os [29]. However, preterm birth or late pregnancy losses were also found, in their cohort of women, lately during pregnancy [16]. For this reason, it should be emphasized that even if cervical polyps are no longer visible during pregnancy, the risk for spontaneous preterm birth and late pregnancy loss is still present [16, 29]. However, such findings need to be validated by further research.
Moreover, Fukuta et al. emphasized, when the resection of the cervical polyps is unavoidable, to stratify risks in accordance with the size of the lesion, since resected polyps with a diameter of at least 12 mm were significantly related to an increased risk of preterm birth [22].
This systematic review has several limitations. First, the most obvious is related to the extremely low number of papers qualified for meta-analysis. Second, the number of the events investigated, concerning all the outcomes, was relatively small, with one paper providing the vast majority of analyzed women [16]. However, both late pregnancy losses and preterm births are uncommon complications that show low incidence rates also in the general population, as reported by Hirayama et al. in the non-polyp group. An additional limitation is related to the design of available studies, which were all historical cohort analysis, reducing the overall quality of available evidence. Nonetheless, the quality assessment using NOS criteria reported high scores for all evaluated papers, reassuring about the quality of included studies. It should be also acknowledged that, due to ethical constraints, it would be impossible to carry out randomized trials comparing cervical polypectomy to expectant management in pregnant women. Finally, all the studies were carried out in Japan, limiting the possible generalization of the findings to more countries.
Despite the above-mentioned limitations, this review is first quantitative synthesis and meta-analysis on the impact of cervical polyps on late pregnancy losses and preterm delivery.
Conclusions
Data concerning the removal of cervical polyps during pregnancy are still limited. To date, polypectomy should be avoided on pregnant women, especially in the case of a decidual rather than an endocervical polyp. Suspected malignancy should be considered the only reason for carrying out the procedure. It is still unclear whether this in-office or inpatient surgical treatment is beneficial, and therefore, the operator should use extreme caution when counseling the patient about the risk and benefits, since the risk of spontaneous pregnancy loss or preterm birth may be relevant. Further research should better address the differences between expectant and active management in terms of preterm birth and late pregnancy loss incidence.
Availability of data and materials
The data that support this systematic review and meta-analysis are available from the corresponding author, upon reasonable request.
References
Budak A, Kanmaz AG (2019) Role of endometrial sampling in cases with asymptomatic cervical polyps. J Gynecol Obstet Hum Reprod 48(3):207–211
Seo N, Tachibana D, Misugi T, Koyama M, Tanaka S (2020) First trimester findings of decidual polyp: caution to avoid polypectomy. Eur J Obstet Gynecol Reprod Biol 249:109–110
Stamatellos I, Stamatopoulos P, Bontis J (2007) The role of hysteroscopy in the current management of the cervical polyps. Arch Gynecol Obstet 276(4):299–303
Riemma G, Schiattarella A, Colacurci N, Vitale SG, Cianci S, Cianci A et al (2020) Pharmacological and non-pharmacological pain relief for office hysteroscopy: an up-to-date review. Climacteric 23(4):376–383
Vitale SG, Haimovich S, Riemma G, Ludwin A, Zizolfi B, De Angelis MC et al (2020) Innovations in hysteroscopic surgery: expanding the meaning of “in-office.” Minim Invasive Ther Allied Technol. https://doi.org/10.1080/13645706.2020.1715437
Vitale SG, Parry JP, Carugno J, Cholkeri-Singh A, Della Corte L, Cianci S et al (2020) Surgical and reproductive outcomes after hysteroscopic removal of retained products of conception: a systematic review and meta-analysis. J Minim Invasive Gynecol. https://doi.org/10.1016/j.jmig.2020.10.028
Stamenov GS, Vitale SG, Della Corte L, Vilos GA, Parvanov DA, Nikolova DN et al (2020) Hysteroscopy and female infertility: a fresh look to a busy corner. Hum Fertility. https://doi.org/10.1080/14647273.2020.1851399
Gokce A, Sukur YE, Ozmen B, Sonmezer M, Berker B, Aytac R et al (2021) The association between operative hysteroscopy prior to assisted reproductive technology and cervical insufficiency in second trimester. Arch Gynecol Obstet 303(5):1347–1352
MacKenzie IZ, Naish C, Rees CM, Manek S (2009) Why remove all cervical polyps and examine them histologically? BJOG 116(8):1127–1129
Karaman E, Akbayir O, Kocaturk Y, Cekic S, Filiz FB, Gulkilik A (2011) Successful treatment of a very rare case: locally treated cervical rhabdomyosarcoma. Arch Gynecol Obstet 284(4):1019–1022
Piriyev E, Mellin W, Romer T (2020) Comparison of aspirating pipettes and hysteroscopy with curettage. Arch Gynecol Obstet 301(6):1485–1492
Levin G, Rottenstreich A (2018) 2nd trimester miscarriage following decidual polypectomy. Eur J Obstet Gynecol Reprod Biol 225:262–263
Romero R, Miranda J, Chaiworapongsa T, Korzeniewski SJ, Chaemsaithong P, Gotsch F et al (2014) Prevalence and clinical significance of sterile intra-amniotic inflammation in patients with preterm labor and intact membranes. Am J Reprod Immunol 72(5):458–474
Hamadeh S, Addas B, Hamadeh N, Rahman J (2018) Conservative management of huge symptomatic endocervical polyp in pregnancy: a case report. Afr J Reprod Health 22(2):88–90
Rottenstreich A, Levin G, Tsur A, Shai D, Meyer R (2021) Chorioamnionitis at latent phase more than doubles the risk for cesarean delivery compared to chorioamnionitis at active phase. Arch Gynecol Obstet 303(4):905–910
Hirayama E, Ebina Y, Kato K, Akabane-Nakagawa K, Okuyama K (2021) Cervical polyps in early pregnancy are a risk factor for late abortion and spontaneous preterm birth: a retrospective cohort study. Int J Gynaecol Obstet. https://doi.org/10.1002/ijgo.13608
Aoki S, Hayashi M, Seki K, Hirahara F (2016) Preterm premature rupture of membrane after polypectomy using an Endoloop polydioxanone suture II(). Clin Case Rep 4(4):331–332
Bornstein J, Bentley J, Bosze P, Girardi F, Haefner H, Menton M et al (2012) 2011 colposcopic terminology of the International Federation for Cervical Pathology and Colposcopy. Obstet Gynecol 120(1):166–172
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62(10):1006–1012
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605
Higgins JPT (2020) Cochrane Collaboration. Cochrane handbook for systematic reviews of interventions, 2nd edn. Wiley-Blackwell, Hoboken
Fukuta K, Yoneda S, Yoneda N, Shiozaki A, Nakashima A, Minamisaka T et al (2020) Risk factors for spontaneous miscarriage above 12 weeks or premature delivery in patients undergoing cervical polypectomy during pregnancy. BMC Pregnancy Childbirth 20(1):27
Tokunaka M, Hasegawa J, Oba T, Nakamura M, Matsuoka R, Ichizuka K et al (2015) Decidual polyps are associated with preterm delivery in cases of attempted uterine cervical polypectomy during the first and second trimester. J Matern Fetal Neonatal Med 28(9):1061–1063
Butt S, Ajibade F, Vijayanand R (2013) Cervical polyps in pregnancy: Is there need for guidelines? BJOG 120:242–243
Yoshida T, Misugi T, Uemura R, Hudaba M, Takase A, Tahara M et al (2019) Analysis of perinatal events complicated with decidual polyp. Placenta 87:68–69
Takahashi Y, Iwagaki S, Itoh M, Nakamura H, Kuwabara K, Hiraku Y et al (2017) Cohort study of the incidence of spontaneous preterm birth and septic abortion referred by pathological examination in Gifu prefecture in Japan. Early Hum Dev 104:33–37
Yoneda N, Yoneda S, Niimi H, Ueno T, Hayashi S, Ito M et al (2016) Polymicrobial Amniotic Fluid Infection with Mycoplasma/Ureaplasma and Other Bacteria Induces Severe Intra-Amniotic Inflammation Associated with Poor Perinatal Prognosis in Preterm Labor. Am J Reprod Immunol 75(2):112–125
Sakai M, Sasaki Y, Yoneda S, Kasahara T, Arai T, Okada M et al (2004) Elevated interleukin-8 in cervical mucus as an indicator for treatment to prevent premature birth and preterm, pre-labor rupture of membranes: a prospective study. Am J Reprod Immunol 51(3):220–225
Kanayama N, Terao T (1991) The relation between granulocyte elastase activity in cervical mucus and gestational cervical polyp. Nihon Sanka Fujinka Gakkai Zasshi 43(1):26–30
Funding
This work did not receive any grant or funding.
Author information
Authors and Affiliations
Contributions
GR: protocol/project development; data analysis; manuscript writing. LDC: data collection; manuscript editing. SGV: data analysis; manuscript writing. SC: data analysis; manuscript editing. MLV: data management; manuscript editing. PG: data management; manuscript editing. LC: protocol/project development; manuscript editing. PDF: protocol/project development; data analysis; manuscript writing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest to disclose regarding this publication.
PROSPERO registration number (date)
CRD42021260847 (July 14, 2021).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Riemma, G., Della Corte, L., Vitale, S.G. et al. Surgical management of endocervical and decidual polyps during pregnancy: systematic review and meta-analysis. Arch Gynecol Obstet 307, 673–680 (2023). https://doi.org/10.1007/s00404-022-06550-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06550-z