Abstract
Purpose
To assess the following in singleton pregnant women: (1) associations between first trimester iron deficiency and obstetric and perinatal outcomes, (2) overall first trimester iron status and (3) post-treatment iron status after intensified iron supplementation.
Methods
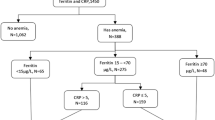
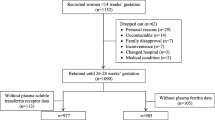
A prospective cohort study was conducted with linkage of first trimester hemoglobin and plasma ferritin with obstetric and perinatal data from a hospital database. Blood sample data were obtained from a Danish University Hospital. The cohort was divided into groups according to ferritin and hemoglobin: (1) iron-deficient anemic (ferritin < 30 ng/mL and Hb < 110 g/L), (2) iron-deficient non-anemic (ferritin < 30 ng/mL and Hb ≥ 110 g/L), and (3) iron-replete non-anemic (ferritin 30–200 ng/mL and Hb ≥ 110 g/L). Obstetric and perinatal outcomes in each iron-deficient group were compared to the iron-replete non-anemic group using multivariable logistic regression. The effect of 4 weeks intensified iron supplementation on hemoglobin and ferritin was assessed by groupwise comparisons.
Results
The cohort comprised 5763 singleton pregnant women, of which 14.2% had non-anemic iron deficiency, and 1.2% had iron-deficiency anemia. Compared to iron-replete non-anemic women, iron-deficient anemic women had a higher risk of gestational diabetes (aOR 3.8, 95% CI 1.4–9.0), and iron-deficient non-anemic women had a higher risk of stillbirth (aOR 4.0, 95% CI 1.0–14.3). In group 1 and 2, 81.5% and 67.7% remained iron-deficient after intensified iron supplementation.
Conclusion
Iron-deficiency anemia was associated with gestational diabetes, and non-anemic iron deficiency with stillbirth, although risk estimates were imprecise due to few events. Iron deficiency was present in 15.4% and often persisted despite 4 weeks intensified iron supplementation.


Similar content being viewed by others
Availability of data and material
Requests on data access can be made through contact with the corresponding author. Data may be accessed upon reasonable request and after review and approval by the Danish Data Protection Agency and the Danish Patient Safety Authority.
Code availability
The code (R) will be available from the corresponding author upon reasonable request.
References
World Health Organization (2015) The global prevalence of anaemia in 2011. WHO, Geneva
World Health Organization (2001) Iron deficiency anaemia assessment, prevention, and control a guide for programme managers. WHO, Geneva
Daru J, Allotey J, Peña-Rosas JP, Khan KS (2017) Serum ferritin thresholds for the diagnosis of iron deficiency in pregnancy: a systematic review. Transfus Med 27:167–174. https://doi.org/10.1111/tme.12408
Georgieff MK (2020) Iron deficiency in pregnancy. Am J Obstet Gynecol 223:516–524. https://doi.org/10.1016/j.ajog.2020.03.006
Bothwell TH (2000) Iron requirements in pregnancy and strategies to meet them. Am J Clin Nutr 72:257S-264S. https://doi.org/10.1093/ajcn/72.1.257S
Dewey KG, Oaks BM (2017) U-shaped curve for risk associated with maternal hemoglobin, iron status, or iron supplementation. Am J Clin Nutr 106:1694S-1702S. https://doi.org/10.3945/ajcn.117.156075
Zhou LM, Yang WW, Hua JZ et al (1998) Relation of hemoglobin measured at different times in pregnancy to preterm birth and low birth weight in Shanghai, China. Am J Epidemiol 148:998–1006. https://doi.org/10.1093/oxfordjournals.aje.a009577
Scholl TO (2005) Iron status during pregnancy: setting the stage for mother and infant. Am J Clin Nutr 81:1218S-1222S. https://doi.org/10.1093/ajcn/81.5.1218
Levy A, Fraser D, Katz M et al (2005) Maternal anemia during pregnancy is an independent risk factor for low birthweight and preterm delivery. Eur J Obstet Gynecol Reprod Biol 122:182–186. https://doi.org/10.1016/j.ejogrb.2005.02.015
Tzur T, Weintraub AY, Sergienko R, Sheiner E (2012) Can anemia in the first trimester predict obstetrical complications later in pregnancy. J Matern Neonatal Med 25:2454–2457. https://doi.org/10.3109/14767058.2012.703723
Dalhøj J, Wiggers P (1991) Haemoglobinkoncentration og jerndepoter hos kvindelige bloddonorer [Hemoglobin concentration and iron stores in female blood donors]. Ugeskr Laeger 153:643–645
World Health Organization (2020) WHO guideline on use of ferritin concentrations to assess iron status in individuals and populations. WHO, Geneva
Pasricha SR, Colman K, Centeno-Tablante E et al (2018) Revisiting WHO haemoglobin thresholds to define anaemia in clinical medicine and public health. Lancet Haematol 5:e60–e62. https://doi.org/10.1016/S2352-3026(18)30004-8
Milman N, Byg K-E, Bergholt T et al (2006) Body iron and individual iron prophylaxis in pregnancy—should the iron dose be adjusted according to serum ferritin? Ann Hematol 85:567–573. https://doi.org/10.1007/s00277-006-0141-1
Khambalia AZ, Collins CE, Roberts CL et al (2016) Iron deficiency in early pregnancy using serum ferritin and soluble transferrin receptor concentrations are associated with pregnancy and birth outcomes. Eur J Clin Nutr 70:358–363. https://doi.org/10.1038/ejcn.2015.157
Danish Health Authority (2013) Anbefalinger for svangreomsorgen [Recommendations for prenatal care], 2nd edn. Danish Health Authority
Danish Health Authority (2021) Anbefalinger for svangreomsorgen [Recommendations for prenatal care], 3rd edn. Danish Health Authority
Danish Society of Obstetrics and Gynaecology (2016) Anaemi og jernmangel under graviditet og i puerperium [Anemia and iron deficiency during pregnancy and in the puerperium]. https://static1.squarespace.com/static/5467abcce4b056d72594db79/t/5714ea13a3360cab668161e3/1460988440726/Guideline+for+anæmi_final.pdf. Accessed 7 Oct 2021
Brixval CS, Thygesen LC, Johansen NR et al (2015) Validity of a hospital-based obstetric register using medical records as reference. Clin Epidemiol 7:509–515. https://doi.org/10.2147/CLEP.S93675
Ekelund CK, Petersen OB, Jørgensen FS et al (2015) The Danish Fetal Medicine Database: establishment, organization and quality assessment of the first trimester screening program for trisomy 21 in Denmark 2008–2012. Acta Obstet Gynecol Scand 94:577–583. https://doi.org/10.1111/aogs.12581
Markova V, Hansen R, Thomsen LL et al (2020) Intravenous iron isomaltoside versus oral iron supplementation for treatment of iron deficiency in pregnancy: protocol for a randomised, comparative, open-label trial. Trials 21:742. https://doi.org/10.1186/s13063-020-04637-z
Maršál K, Persson P-H, Larsen T et al (1996) Intrauterine growth curves based on ultrasonically estimated foetal weights. Acta Paediatr 85:843–848. https://doi.org/10.1111/j.1651-2227.1996.tb14164.x
Brereton M, McCafferty R, Marsden K et al (2016) Recommendation for standardization of haematology reporting units used in the extended blood count. Int J Lab Hematol 38:472–482. https://doi.org/10.1111/ijlh.12563
R Core Team (2019) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Venables WN, Ripley BD (2002) Modern applied statistics with S, 4th edn. Springer, New York
Mei Z, Cogswell ME, Looker AC et al (2011) Assessment of iron status in US pregnant women from the national health and nutrition examination survey (NHANES), 1999–2006. Am J Clin Nutr 93:1312–1320. https://doi.org/10.3945/ajcn.110.007195
Vandevijvere S, Amsalkhir S, Van Oyen H et al (2013) Iron status and its determinants in a nationally representative sample of pregnant women. J Acad Nutr Diet 113:659–666. https://doi.org/10.1016/j.jand.2012.10.021
Auerbach M, Abernathy J, Juul S et al (2021) Prevalence of iron deficiency in first trimester, nonanemic pregnant women. J Matern Fetal Neonatal Med 34:1002–1005. https://doi.org/10.1080/14767058.2019.1619690
Centers for Disease Control and Prevention (1998) Recommendations to prevent and control iron deficiency in the United States. MMWR Recomm Rep 47:1–29
Lee AI, Okam MM (2011) Anemia in pregnancy. Hematol Oncol Clin N Am 25:241–259. https://doi.org/10.1016/j.hoc.2011.02.001
Roy NBA, Pavord S (2018) The management of anaemia and haematinic deficiencies in pregnancy and post-partum. Transfus Med 28:107–116. https://doi.org/10.1111/tme.12532
Breymann C, Honegger C, Hösli I, Surbek D (2017) Diagnosis and treatment of iron-deficiency anaemia in pregnancy and postpartum. Arch Gynecol Obstet 296:1229–1234. https://doi.org/10.1007/s00404-017-4526-2
Muñoz M, Peña-Rosas JP, Robinson S et al (2018) Patient blood management in obstetrics: management of anaemia and haematinic deficiencies in pregnancy and in the post-partum period: NATA consensus statement. Transfus Med 28:22–39. https://doi.org/10.1111/tme.12443
Ribot B, Aranda N, Viteri F et al (2012) Depleted iron stores without anaemia early in pregnancy carries increased risk of lower birthweight even when supplemented daily with moderate iron. Hum Reprod 27:1260–1266. https://doi.org/10.1093/humrep/des026
Murphy JF, Newcombe RG, O’Riordan J et al (1986) Relation of haemoglobin levels in first and second trimesters to outcome of pregnancy. Lancet 327:992–995. https://doi.org/10.1016/S0140-6736(86)91269-9
Tiongco RE, Arceo E, Clemente B, Pineda-Cortel MR (2019) Association of maternal iron deficiency anemia with the risk of gestational diabetes mellitus: a meta-analysis. Arch Gynecol Obstet 299:89–95. https://doi.org/10.1007/s00404-018-4932-0
Bowers KA, Olsen SF, Bao W et al (2016) Plasma concentrations of ferritin in early pregnancy are associated with risk of gestational diabetes mellitus in women in the Danish National Birth Cohort. J Nutr 146:1756–1761. https://doi.org/10.3945/jn.115.227793
Kataria Y, Wu Y, de Horskjær PH et al (2018) Iron status and gestational diabetes-a meta-analysis. Nutrients 10:621. https://doi.org/10.3390/nu10050621
Khambalia AZ, Aimone A, Nagubandi P et al (2016) High maternal iron status, dietary iron intake and iron supplement use in pregnancy and risk of gestational diabetes mellitus: a prospective study and systematic review. Diabet Med 33:1211–1221. https://doi.org/10.1111/dme.13056
Sun C, Wu QJ, Gao SY et al (2020) Association between the ferritin level and risk of gestational diabetes mellitus: a meta-analysis of observational studies. J Diabetes Investig 11:707–718. https://doi.org/10.1111/jdi.13170
Fisher AL, Nemeth E (2017) Iron homeostasis during pregnancy. Am J Clin Nutr 106:1567S-1574S. https://doi.org/10.3945/ajcn.117.155812
Aguree S, Gernand AD (2019) Plasma volume expansion across healthy pregnancy: a systematic review and meta-analysis of longitudinal studies. BMC Pregnancy Childbirth 19:508. https://doi.org/10.1186/s12884-019-2619-6
Means RT (2020) Iron deficiency and iron deficiency anemia: implications and impact in pregnancy, fetal development, and early childhood parameters. Nutrients 12:447. https://doi.org/10.3390/nu12020447
de Haas S, Ghossein-Doha C, van Kuijk SMJ et al (2017) Physiological adaptation of maternal plasma volume during pregnancy: a systematic review and meta-analysis. Ultrasound Obstet Gynecol 49:177–187. https://doi.org/10.1002/uog.17360
Knudsen VK, Hansen HS, Ovesen L et al (2007) Iron supplement use among Danish pregnant women. Public Health Nutr 10:1104–1110. https://doi.org/10.1017/S136898000769956X
Acknowledgements
We acknowledge and are thankful for the data management support from Steen Christian Rasmussen, MSc, MPH.
Funding
This study has been covered solely by internal funding.
Author information
Authors and Affiliations
Contributions
RH, ALS, VMS, CH, LK and AP were involved in the conception and design of the study. RH and VMS carried out data collection. RH and ALS performed data analyses. RH drafted the manuscript. All authors were involved in the interpretation of the data and reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
When the study was conducted, Rebecka Hansen and Veronika Markova Sommer were investigators and Charlotte Holm primary investigator for a clinical trial sponsored by Pharmacosmos A/S. As investigators, Rebecka Hansen and Veronika Markova Sommer had salary costs funded by Pharmacosmos A/S. Rebecka Hansen and Charlotte Holm have served on advisory boards for Pharmacosmos A/S. However, Pharmacosmos A/S did not play any role or had any influence on this cohort study. Only the named authors had influence on the study design, conduct, analysis, interpretation and the manuscript. The authors have no additional conflicts of interest to declare.
Ethics approval
The study was approved by the Danish Data Protection Agency (J. No.: AHH-2017-031, I-suite number: 05349) and the Danish Patient Safety Authority (J. No.: 3-3013-2410/1). According to Danish legislation, informed written consent from patients is not required for this specific type of study. The reporting of the study adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hansen, R., Spangmose, A.L., Sommer, V.M. et al. Maternal first trimester iron status and its association with obstetric and perinatal outcomes. Arch Gynecol Obstet 306, 1359–1371 (2022). https://doi.org/10.1007/s00404-022-06401-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06401-x