Abstract
Objective:
To assess the efficacy of doubling the 30 mg dose of iron in women with iron deficiency anemia (IDA) in singleton pregnancies.
Study Design:
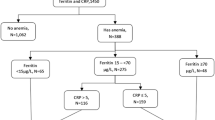
Prospective randomized controlled trial. Iron-deficient women were randomized during the second trimester to receive one or two capsules of daily iron supplement, containing 34 mg of ferrous sulfate, from 17 weeks until 6 weeks postpartum. The primary outcome was hemoglobin (Hgb) at 35 weeks. Secondary outcomes included ferritin at 35 weeks, Hgb during pregnancy and postpartum, birth weights, preterm birth rate, gastrointestinal side effects, intravenous iron administration and compliance.
Results:
In all, 160 women were randomized to receive one capsule and 164 received two capsules. Both groups had similar Hgb (10.1 g dl−1) and ferritin (9.3 and 9.4 ng l−1) at allocation. Hgb concentration in both groups was similar at 35 weeks (10.8 g dl−1). There were no significant differences in any of the secondary outcomes.
Conclusion:
In IDA pregnant women, a single dose of iron is as effective as a double dose.

Similar content being viewed by others
References
Bothwell T . Iron requirements in pregnancy and strategies to meet them. Am J Clin Nutr 2000; 72 (1 Suppl): 257S–264S.
World Health Organization (WHO) The Global Prevalence of Anaemia in 2011. WHO: Geneva, 2015.
Levy A, Fraser D, Katz M, Mazor M, Sheiner E . Maternal anemia during pregnancy is an independent risk factor for low birthweight and preterm delivery. Eur J Obstet Gynecol Reprod Biol 2005; 122 (2): 182–186.
Lozoff B, Georgieff MK . Iron deficiency and brain development. Semin Pediatr Neurol 2006; 13 (3): 158–165.
Cantor AG, Bougatsos C, Dana T, Blazina I, McDonagh M . Routine iron supplementation and screening for iron deficiency anemia in pregnancy: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med 2015; 162 (8): 566–576.
Milman N . Anemia—still a major health problem in many parts of the world!. Ann Hematol 2011; 90 (4): 369–377.
Norwegian Board of Health. Guidelines for maternal welfare in primary health care. Veiledningsserie 1995; 5: 48–50.
Milman N, Byg KE, Bergholt T, Eriksen L, Hvas AM . Body iron and individual iron prophylaxis in pregnancy-should the iron dose be adjusted according to serum ferritin? Ann Hematol 2006; 85 (9): 567–573.
Thomas CE, Guillet R, Queenan RA, Cooper EM, Kent TR, Pressman EK et al. Vitamin D status is inversely associated with anemia and serum erythropoietin during pregnancy. Am J Clin Nutr 2015; 102 (5): 1088–1095.
American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 95: anemia in pregnancy. Obstet Gynecol 2008; 112 (1): 201–207.
Guideline: Intermittent Iron and Folic Acid Supplementation in Menstruating Women WHO Guidelines Approved by the Guidelines Review Committee. World Health Organization: Geneva, 2011.
Hanieh S, Ha TT, Simpson JA, Casey GJ, Khuong NC, Thoang DD et al. The effect of intermittent antenatal iron supplementation on maternal and infant outcomes in rural Viet Nam: a cluster randomised trial. PLoS Med 2013; 10 (6): e1001470.
Adighian F, Haydeh Samiei H, Alaoddolehei H, Kalantari N . Efficacy of daily versus intermittent administration of iron supplementation in anemia or blood indices during pregnancy. Caspian J Intern Med 2013; 4 (1): 569–573.
Roberfroid D, Huybregts L, Habicht JP, Lanou H, Henry MC, Meda N et alMISAME Study Group. MISAME Study Group. Randomized controlled trial of 2 prenatal iron supplements: is there a dose-response relation with maternal Hgb? Am J Clin Nutr 2011; 93 (5): 1012–1018.
Moretti D, Goede JS, Zeder C, Jiskra M, Chatzinakou V, Tjalsma H et al. Oral iron supplements increase hepcidin and decrease iron absorption from daily or twice-daily doses in iron-depleted young women. Blood 2015; 126 (17): 1981–1989.
Rimon E, Kagansky N, Kagansky M, Mechnick L, Mashiah T, Namir M et al. Are we giving too much iron? Low-dose iron therapy is effective in octogenarians. Am J Med 2005; (10) 118: 1142–1147.
Siega-Riz AM, Hartzema AG, Turnbull C, Thorp J, McDonald T, Cogswell ME . The effects of prophylactic iron given in prenatal supplements on iron status and birth outcomes: a randomized controlled trial. Am J Obstet Gynecol 2006; 194 (2): 512–519.
Ramakrishnan U, González-Cossío T, Neufeld LM, Rivera J, Martorell R . Multiple micronutrient supplementation during pregnancy does not lead to greater infant birth size than does iron-only supplementation: a randomized controlled trial in a semirural community in Mexico. Am J Clin Nutr 2003; 77 (3): 720–725.
Gupta P, Ray M, Dua T, Radhakrishnan G, Kumar R, Sachdev HP . Multimicronutrient supplementation for undernourished pregnant women and the birth size of their offspring: a double-blind, randomized, placebo-controlled trial. Arch Pediatr Adolesc Med 2007; 161 (1): 58–64.
Christian P, Shrestha J, LeClerq SC, Khatry SK, Jiang T, Wagner T et al. Supplementation with micronutrients in addition to iron and folic acid does not further improve the hematologic status of pregnant women in rural Nepal. J Nutr 2003; 133 (11): 3492–3498.
Bánhidy F, Acs N, Puhó EH, Czeizel AE . Iron deficiency anemia: pregnancy outcomes with or without iron supplementation. Nutrition 2011; 27 (1): 65–72.
Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, Requejo JH et al. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ 2010; 88 (1): 31–38.
Derbyshire E, Davies J, Costarelli V, Dettmar P . Diet, physical inactivity and the prevalence of constipation throughout and after pregnancy. Matern Child Nutr 2006; 2 (3): 127–134.
Tolkien Z, Stecher L, Mander AP, Pereira DI, Powell JJ . Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults: a systematic review and meta-analysis. PLoS ONE 2015; 10 (2): 1–20.
Otten J, Pitzi HJ, Meyers LD (eds). Dietary Reference Intakes: The Essential Guide to Nutrient Requirements. The National Academies Press: Washington DC, 2006.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Shinar, S., Skornick-Rapaport, A. & Maslovitz, S. Iron supplementation in singleton pregnancy: Is there a benefit to doubling the dose of elemental iron in iron-deficient pregnant women? a randomized controlled trial. J Perinatol 37, 782–786 (2017). https://doi.org/10.1038/jp.2017.43
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2017.43
- Springer Nature America, Inc.