Abstract
Background
Introduction: There is clear evidence that fetuses with intrauterine growth restriction (IUGR) do not receive the minimum evidence-based care during their antenatal management.
Objective
Considering that optimal management of IUGR may reduce neonatal morbi-mortality in IUGR, the objective of the present study was to evaluate the impact of antenatal management of IUGR according to the recommendations of the French college of gynecologists and obstetricians (CNGOF) on the neonatal prognosis of IUGR fetuses.
Study design
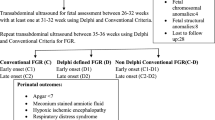
From a historical cohort of 31,052 children, born at the Femme Mère Enfant hospital (Lyon, France) between January 1, 2011 and December 31, 2017, we selected the population of IUGR fetuses. The minimum evidence-based care (MEC) in the antenatal management of fetuses with IUGR was defined according to the CNGOF recommendations and neonatal prognosis of early and late IUGR fetuses were assessed based on the whether or not they received MEC. The neonatal prognosis was defined according to a composite criterion that included neonatal morbidity and mortality.
Results
A total of 1020 fetuses with IUGR were studied. The application of MEC showed an improvement in the neonatal prognosis of early-onset IUGR (p = 0.003), and an improvement in the neonatal prognosis of IUGR born before 32 weeks (p = 0.030). Multivariate analysis confirmed the results showing an increase in neonatal morbi-mortality in early-onset IUGR in the absence of MEC with OR 1.79 (95% CI 1.01–3.19).
Conclusion
Diagnosed IUGR with MEC had a better neonatal prognosis when born before 32 weeks. Regardless of the birth term, MEC improved the neonatal prognosis of fetuses with early IUGR. Improvement in the rate of MEC during antenatal management has a significant impact on neonatal prognosis.
Similar content being viewed by others
References
McCowan LM, Figueras F, Anderson NH (2018) Evidence-based national guidelines for the management of suspected fetal growth restriction: comparison, consensus, and controversy. Am J Obstet Gynecol 218:S855–S868
Baschat AA (2018) Planning management and delivery of the growth-restricted fetus. Best Pract Res Clin Obstet Gynaecol 49:53–65
Savchev S, Sanz-Cortes M, Cruz-Martinez R et al (2013) Neurodevelopmental outcome of full-term small-for-gestational-age infants with normal placental function. Ultrasound Obstet Gynecol 42:201–206
Katanoda K, Noda M, Goto A et al (2017) Impact of birth weight on adult-onset diabetes mellitus in relation to current body mass index: The Japan Nurses’ Health Study. J Epidemiol 27:428–434
Lindström L, Wikström A-K, Bergman E, Lundgren M (2017) Born small for gestational age and poor school performance—how small is too small? Horm Res Paediatr 88:215–223
Senat M-V, Tsatsaris V (2013) Prenatal management of isolated IUGR. J Gynecol Obstet Biol Reprod (Paris) 42:941–965
Vayssière C, Sentilhes L, Ego A et al (2015) Fetal growth restriction and intra-uterine growth restriction: guidelines for clinical practice from the French College of Gynaecologists and Obstetricians. Eur J Obstet Gynecol Reprod Biol 193:10–18
McCowan LME et al (2010) Risk factors for small-for-gestational-age infants by customised birthweight centiles: data from an international prospective cohort study. BJOG 117:1599–1607
Lindqvist PG, Molin J (2005) Does antenatal identification of small-for-gestational age fetuses significantly improve their outcome? Ultrasound Obstet Gynecol 25:258–264
Gardosi J, Madurasinghe V, Williams M et al (2013) Maternal and fetal risk factors for stillbirth: population based study. BMJ 346:f108
Ayoubi ME, Jarreau P-H, Reempts PV et al (2016) Does the antenatal detection of fetal growth restriction (FGR) have a prognostic value for mortality and short-term morbidity for very preterm infants? Results from the MOSAIC cohort. J Matern Fetal Neonatal Med 29:596–601
Zeitlin J, Manktelow BN, Piedvache A et al (2016) Use of evidence based practices to improve survival without severe morbidity for very preterm infants: results from the EPICE population based cohort. BMJ 354:i2976
Beune IM, Bloomfield FH, Ganzevoort W et al (2018) Consensus based definition of growth restriction in the newborn. J Pediatr 196:71-76.e1
Gordijn SJ, Beune IM, Thilaganathan B et al (2016) Consensus definition of fetal growth restriction: a Delphi procedure. Ultrasound Obstet Gynecol 48:333–339
Gordijn SJ, Beune IM, Ganzevoort W (2018) Building consensus and standards in fetal growth restriction studies. Best Pract Res Clin Obstet Gynaecol 49:117–126
Mamelle N, Cochet V, Claris O (2001) Definition of fetal growth restriction according to constitutional growth potential. Neonatology 80:277–285
Mamelle N, Munoz F, Grandjean H (1996) Fetal growth from the AUDIPOG study. I. Establishment of reference curves. J Gynecol Obstet Biol Reprod (Paris) 25:61–70
Massoud M, Duyme M, Fontanges M et al (2016) Chart for estimation of fetal weight 2014 by the French College of Fetal Sonography (CFEF). J Gynecol Obstet Biol Reprod (Paris) 45:80–85
Robinson HP, Sweet EM, Adam AH (1979) The accuracy of radiological estimates of gestational age using early fetal crown-rump length measurements by ultrasound as a basis for comparison. Br J Obstet Gynaecol 86:525–528
Yoon BH, Syn HC, Kim SW (1992) The efficacy of Doppler umbilical artery velocimetry in identifying fetal acidosis. A comparison with fetal biophysical profile. J Ultrasound Med 11:1–6
Frey HA, Odibo AO, Dicke JM et al (2014) Stillbirth risk among fetuses with ultrasound-detected isolated congenital anomalies. Obstet Gynecol 124:91–98
Baschat AA (2010) Fetal growth restriction—from observation to intervention. J Perinat Med 38:239–246
Baschat AA, Gembruch U, Harman CR (2001) The sequence of changes in Doppler and biophysical parameters as severe fetal growth restriction worsens. Ultrasound Obstet Gynecol 18:571–577
Ganzevoort W, Mensing Van Charante N, Thilaganathan B et al (2017) How to monitor pregnancies complicated by fetal growth restriction and delivery before 32 weeks: post-hoc analysis of TRUFFLE study. Ultrasound Obstet Gynecol 49:769–777
Lees CC, Marlow N, van Wassenaer-Leemhuis A et al (2015) 2 year neurodevelopmental and intermediate perinatal outcomes in infants with very preterm fetal growth restriction (TRUFFLE): a randomised trial. Lancet 385:2162–2172
Temming LA, Dicke JM, Stout MJ et al (2017) Early second-trimester fetal growth restriction and adverse perinatal outcomes. Obstet Gynecol 130:865–869
Parra-Saavedra M, Crovetto F, Triunfo S et al (2014) Association of Doppler parameters with placental signs of underperfusion in late-onset small-for-gestational-age pregnancies. Ultrasound Obstet Gynecol 44:330–337
Crimmins S, Desai A, Block-Abraham D et al (2014) A comparison of Doppler and biophysical findings between liveborn and stillborn growth-restricted fetuses. Am J Obstet Gynecol 211:669.e1–10
Oros D, Figueras F, Cruz-Martinez R et al (2011) Longitudinal changes in uterine, umbilical and fetal cerebral Doppler indices in late-onset small-for-gestational age fetuses. Ultrasound Obstet Gynecol 37:191–195
Flamant C, Gascoin G (2013) Short-term outcome and small for gestational age newborn management. J Gynecol Obstet Biol Reprod (Paris) 42:985–995
Gascoin G, Flamant C (2013) Long-term outcome in context of intra uterine growth restriction and/or small for gestational age newborns. J Gynecol Obstet Biol Reprod (Paris) 42:911–920
Gaccioli F, Aye ILMH, Sovio U et al (2018) Screening for fetal growth restriction using fetal biometry combined with maternal biomarkers. Am J Obstet Gynecol 218:S725–S737
Atallah A, Butin M, Moret S et al (2021) Standardized healthcare pathway in intrauterine growth restriction and minimum evidence-based care. J Gynecol Obstet Hum Reprod 50(1):101998
Atallah A, Butin M, Moret S et al (2021) Impact of the healthcare pathway on the rate of obstetrical interventions in small for gestational age fetuses (IATROPAG Study). Gynecol Obstet Fertil Senol 49(9):665–671
Author information
Authors and Affiliations
Contributions
AA: Conceptualization, Methodology, Writing—Original Draft, MB: Writing—Review and Editing. SM: Formal analysis. OC: Writing—Review and Editing, Supervision. MM: Review and Editing. PG: Writing—Review and Editing, Supervision. MD-D: Conceptualization, Methodology, Writing—Review and Editing.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and the national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethical approval was given by the Ethics committee of Hospices Civils de Lyon, Pr Jean François GUERIN (n° 20-90).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Atallah, A., Butin, M., Moret, S. et al. Minimum evidence-based care in intrauterine growth-restricted fetuses and neonatal prognosis. Arch Gynecol Obstet 305, 1159–1168 (2022). https://doi.org/10.1007/s00404-021-06231-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-021-06231-3