Abstract
Purpose
As data on this topic are sparse and contradictory, we aimed to ascertain the opinions of the members of the German Society of Gynecologic Endoscopy (AGE) regarding the use of robotic surgery in the treatment of ovarian malignancies.
Methods
In 2015, an anonymous questionnaire was sent to AGE members to assess their views on the treatment of ovarian malignancies by robotic surgery according to T stage and the current treatment practices in their facilities.
Results
Of the 228 respondents, 132 (58%) were fellows or attending physicians and 156 (68%) worked at university hospitals or tertiary referral centers. Most [n = 218 (96%)] respondents reported treating < 10% of their patients using robotic surgery. Respondents felt that T1 and borderline ovarian tumors, but not T2 (51%) or T3/4 (76%) tumors, should and could be treated by robot surgery. 162 (71%) respondents considered the currently available data on this subject to be insufficient, and 42% indicated their willingness to participate in clinical studies on the applicability of robotic surgery to the treatment of T1/2 ovarian tumors.
Conclusion
The majority of AGE members surveyed considered robotic surgery to be an option for the treatment of T1 ovarian malignancies and borderline ovarian tumors. However, prospective randomized studies are needed to determine the relevance of robotic surgery in this context.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With approximately 7250 newly diagnosed cases per year, ovarian cancer is among the most frequently occurring cancers among women in Germany and the second leading cause of death from gynecological malignancies worldwide [1, 2]. Despite the optimization of chemotherapeutic regimens and the development of new therapies, surgery (using optimal procedures) remains the core element of ovarian cancer treatment. Survival rates depend directly on the extent of debulking, notably on the achievement of complete cytoreduction (R0 resection), and on the amount of tumor remaining in the abdomen postoperatively [3, 4].
Laparotomy has been the gold standard for the surgical treatment of gynecological malignancies. With constant progress in laparoscopy and robotic surgery in past decades and the widespread use of minimally invasive surgery (MIS) for the treatment of benign gynecological diseases, the focus has shifted gradually to the use of robotic surgery for the treatment of gynecological malignancies [5]. The benefits of MIS include reduced postoperative pain intensity, wound infection rates, length of hospitalization, and procedure-associated morbidity, as well as the possibility of immediate adjuvant therapy initiation. These advantages have led to the gradual implementation of laparoscopy and robotic surgery as alternatives to open surgery for the treatment of certain gynecologic malignancies [6]. Major concerns about MIS use in the gynecological context, however, are related to the ability to achieve sufficient oncological safety; they include the risks of intraoperative tumor rupture, port site metastasis, and peritoneal dissemination of tumor cells, as well as the questionable efficacy of surgical staging, which have prevented an implementation of laparoscopy and robotic surgery for the treatment of ovarian cancer [7,8,9].
The German S3 guidelines for diagnosis, treatment, and surveillance of ovarian malignancies recommend the use of MIS only in clinical trials, as few data regarding the oncological safety of these procedures are available and potential risks are not sufficiently recognized [10]. Internationally, some institutions have made efforts to implement MIS for the treatment of early-stage ovarian cancer, staging of advanced disease, and assessment of the neoadjuvant treatment response, and reported a comparable outcome of MIS in terms of feasibility and surgical parameters as against open surgery [11,12,13]. The role of MIS in the treatment of ovarian malignancies, however, remains controversial. This survey was conducted to assess the opinions of members of the German Society of Gynecologic Endoscopy (AGE) regarding the use of robotic surgery for the treatment of ovarian neoplasias and borderline tumors according to T stage, and to obtain information about current treatment practices in these members’ institutions.
Methods
The present survey was the second part of a two-part study of the use of MIS in the treatment of ovarian neoplasia. The first survey examined the use of laparoscopy in the treatment of ovarian malignancies, and has been reported on elsewhere [14].
Before starting the study, AGE created a task force for questionnaire design, survey implementation, and data analysis. The study design was approved by the executive board of AGE [14]. According to the local ethics committee regulations (Saarland institutional review board) no ethical approval was needed for this survey. Informed consent for publication was obtained from all survey participants.
From February to October 2015, an anonymous online survey was sent to AGE members via email, and posted on the homepage of the AGE website. Two email reminders were sent during this period. The online survey was accessed via the Google Drive online survey system (Google Ireland Limited, Dublin, Ireland). After the data collection period, a research associate at the Department of Gynecology and Obstetrics, Saarland University Hospital, Homburg, entered the data without respondent-identifying information into an Excel (version 2010; Microsoft Corporation, Redmond, WA, USA) database.
The first part of the questionnaire solicited demographic and workplace information, such as respondents’ age, sex, and education level, as well as the hospital level and annual ovarian cancer surgery volume and respondents’ possible concerns regarding the oncological safety and precision of MIS for ovarian cancer in general. Those results have been published within the first manuscript on laparoscopic treatment of ovarian malignancies [14]. The second part solicited respondents’ opinions about the use of robotic surgery in the treatment of ovarian malignancies and borderline ovarian tumors, as well as information on current ovarian neoplasia treatment practices in their facilities. Respondents were asked about their opinions about the use of robotic surgery for ovarian neoplasia according to the T stage following the TNM classification for malignant tumors [15]. The next part of the survey solicited respondents’ opinions about currently available data on the use of robotic surgery in the treatment of ovarian neoplasia, and inquired about their willingness to participate in clinical trials on this topic. For the calculation of descriptive statistics, the data were transferred to SPSS (version 19; SPSS Inc., Chicago, IL, USA). Categorical data are reported as frequencies with percentages.
Results
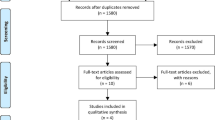
In total, 235 physicians who were AGE members (18% of those contacted) took part in the online survey. Seven incomplete questionnaires were excluded, leaving 228 completed questionnaires that were included in the final analysis.
Respondent and practice characteristics
The sample comprised 128 (56%) male and 100 (44%) female gynecologists with a mean age of 36 (range, 26–62) years. 66 (29%) respondents were residents, 40 (18%) were fellows, 92 (40%) were attending physicians, and 30 (13%) were department heads. Almost half [n = 108 (47%)] of the respondents worked at university hospitals, 48 (21%) worked at clinics providing maximum or standard care, and 24 (11%) had private gynecological practices. One hundred twelve (49%) respondents indicated that they performed operations to treat ovarian malignancies and 172 (75%) indicated that they assisted with such interventions. 77 (34%) respondents reported that < 20 such operations were performed per year in their facilities, 106 (46%) reported 20–50 interventions per year, and 45 (20%) reported 50–100 interventions per year. Most [n = 218 (96%)] respondents indicated that robotic surgery was used in 0–10% of all ovarian cancer cases at their facilities (Table 1).
Current practice and perceived applicability of robotic surgery
42 (18%), 24 (10%), and 30 (13%) respondents reported that T1a, T1b, and T1c tumors, respectively, were treated with robotic surgery at their facilities; 164 (72%), 204 (90%), and 198 (87%) respondents reported no such practice for T1a–c tumors, respectively. 22 (10%) respondents reported using robotic surgery to treat T1a tumors in clinical trials; no respondent reported such use for T1b or T1c tumors. 14 (6%) respondents reported T2 tumor treatment with robotic surgery, and 214 (94%) respondents reported no such practice. Similarly, 216 (95%) respondents reported no use of robotic surgery to treat T3/4 ovarian tumors, and 12 (5%) respondents reported using such treatment only in clinical trials (Table 2).
Reported concerns about the oncological safety of MIS in general were the inaccuracy of abdominal staging (30%) and the risks of ovarian tumor rupture (27%), intra-abdominal tumor cell spread (18%), and port-site metastasis (14%) [14]. 24 (11%) respondents indicated that they saw no disadvantage of the use of MIS relative to open surgery (Table 1) [14].
Approximately half of the respondents indicated that robotic surgery should or could be used to treat T1a [n = 136 (60%)], T1b [n = 108 (47%)], and T1c [n = 104 (46%)] tumors; 52 (22%), 60 (26%), and 57 (25%) respondents indicated that robotic surgery should be used to treat these respective tumor types only in clinical trials, and 40 (18%), 60 (26%), and 67 (29%) respondents, respectively, indicated that robotic surgery should not be used to treat these tumors. 56 (25%) respondents indicated that T2 tumors should or could be treated with robotic surgery, 54 (24%) considered this application to be appropriate only in clinical trials, and 118 (51%) indicated that robotic surgery should not be used to treat T2 tumors. No respondent believed that robotic surgery should be used to treat T3/4 tumors, 21 (9%) respondents indicated that this technique could be used for these tumors, 35 (15%) accepted such use only in clinical trials, and 172 (76%) indicated that robotic surgery should not be used in such cases (Table 3).
Perspectives on available data and clinical trial participation
One hundred sixty-two (71%) respondents considered the currently available data on the use of robotic surgery to treat ovarian cancer to be insufficient, and 66 (29%) respondents could not provide any information. 98 (43%) and 50 (22%) of respondents respectively felt that further research on the use of robotic surgery to treat T1/2 and T3/4 ovarian cancer was needed. 95 (42%) respondents indicated that they were willing to participate in clinical trials investigating the robotic surgical treatment of T1/2 carcinomas; as optimal study designs, 128 (56%) respondents suggested a prospective randomized study, 68 (30%) suggested a meta-analysis, and 32 (14%) suggested a retrospective study. 50 (22%) respondents indicated that they would not participate in clinical trials on the use of robotic surgery in the treatment of T3/4 ovarian tumors, 53 (23%) respondents indicated that they would participate in such trials; and 50 (22%) could not provide any information; for research on this topic, 108 (47%) respondents suggested a prospective randomized study, 66 (29%) a meta-analysis, and 54 (24%) a retrospective study, respectively (Table 4).
Robotic surgery for borderline ovarian tumors
In total, 158 (69%) respondents stated that borderline ovarian tumors would not be treated with robotic surgery in their practices, 45 (20%) respondents treated such tumors with robotic surgery at their facilities and 25 (11%) respondents reported the use of such treatment in clinical trials. 160 (70%) respondents stated that borderline ovarian tumors should or could be treated with robotic surgery, and 34 (15%) respondents each did and did not favor such treatment within the framework of clinical studies. 126 (55%) respondents indicated that the treatment of borderline ovarian tumors by robotic surgery required further evaluation, 49 (22%) were opposed to new studies on the subject, and 53 (23%) could not provide any information. Similar numbers of respondents reported that they would [n = 93 (41%)] and would not [n = 102 (45%)] participate in clinical trials on robotic surgical therapy for borderline ovarian tumors; as study designs, 34 (15%) respondents suggested a retrospective study, 54 (24%) a meta-analysis, and 140 (61%) a prospective randomized controlled study, respectively (Table 5).
Discussion
The aim of the present study was to examine the opinion of the AGE members regarding the use of robotic surgery in the treatment of ovarian neoplasia and to survey the current application of robotic surgery in their respective facilities. This survey showed that the use of robotic surgery in the treatment of ovarian tumors was not prevalent in the facilities of responding AGE members; 28% of respondents indicated that T1a tumors were treated by robotic surgery, including in clinical studies, and the proportion declined with increasing tumor stage to 5% for T3/4 tumors in clinical trials alone. Thirty-one percent of respondents reported the use of robotic surgery to treat borderline ovarian tumors, of which 11% reported this application only in clinical trials. In contrast, AGE members favored the use of robotic surgery, especially for T1a–c tumors (60% for T1a and declining thereafter) and borderline tumors (70%).
These opinions coincide with findings from retrospective case–control studies conducted in Italy and China, which confirmed that the adequacy and reliability of robotic surgery for the treatment of early-stage ovarian cancer, in terms of surgical outcome and oncological safety, were equivalent to those of conventional laparotomy, although sample sizes were small (7–33 patients) [16,17,18]. Other groups have proposed the use of robotic surgery at least for the staging of early ovarian cancer in selected patient groups, and as a possible alternative to laparoscopy when performed by gynecologists with surgical experience [19, 20].
The literature contains contradictory information about differences in the outcomes of robotic surgery and conventional laparoscopy. In a prospective randomized study of endometrial cancer treatment, Mäenpää et al. [21] showed that surgical outcomes were equivalent, although robot-assisted surgery reduced the operating time and rate of conversion to laparotomy relative to conventional laparoscopy. In contrast, El Khouly et al. [22] observed equivalent technical efficiency of the two techniques, but shorter operating times for conventional laparoscopy performed to remove adnexal findings the same technical efficiency.
Nezhat et al. [23] compared perioperative outcome and complication rates between laparotomy, laparoscopy and robotic surgery in the treatment of ovarian, tube and peritoneal cancer in their study. In contrast to the opinion of AGE members obtained in the present study, Nezhat et al., concluded in their retrospective study that laparoscopy and robotic surgery are not inferior to laparotomy in early and advanced stages with regard to perioperative outcome, and appear therefore as an acceptable alternative in the therapy of selected patients. In agreement with AGE members, other authors have expressed clear reservations about the use of robotic surgery for the treatment of T3/4 tumors [16,17,18].
Divergent perspectives on the safety of robotic surgery in the treatment of ovarian neoplasia, about which up to 30% of participants in the present study expressed concern, have been discussed in the literature. For example, some groups have argued that tumor capsule rupture is relevant for overall survival, whereas others have stated that intraoperative rupture does not shorten the progression-free survival time [24,25,26]. In a review, Minig et al. [20] expressed no concern about the use of robotic surgery in terms of inaccurate peritoneal staging, at least in the early stages of ovarian cancer, as long as the staging is performed by experienced surgeons in appropriate centers; they noted that further studies of the application of robotic surgery in advanced ovarian cancer staging are needed. With regard to intra-abdominal tumor cell carryover, animal experiments have shown the increased production of interleukins and growth factors in the presence of pneumoperitoneum, and in vitro experiments have shown increased ovarian carcinoma cell line growth rates after exposure to carbon dioxide [27, 28]. However, in vivo studies showed no increase in the frequency of recurrence after MIS compared with open surgery [29,30,31]. Seror et al. [32] found no metastasis in trocar site areas at a median of 504 days after the robotic surgical treatment of ovarian, endometrial, and cervical carcinomas. Another group reported a low rate (1.41%) of port-site metastasis after the use of robotic surgery to treat gynecological malignancies, which coincided with the rate of metastasis in the puncture canal after traditional laparoscopy (1.96%) [9, 33]. These rates are also comparable to those of recurrence in the scar area after conventional laparotomy [34]. Whether the instruments used in robotic surgery modify the risk of metastasis at trocar puncture sites has not been clarified sufficiently; further clinical studies are required [33].
The discrepancy between the currently limited use of robotic surgery in the treatment of ovarian malignancies (even T1a tumors) and AGE members' opinions about the applicability of this technique can be attributed to the limitations of robotic surgery in general, which have hampered the spread of this technique in Germany. The main limitations are the greater cost of equipment acquisition and maintenance relative to that for conventional laparoscopy, and the associated lack of equipment available for treatment and research [35]. In addition, medical staff and surgeons require special training before they can routinely handle surgical robots [36]. According to the Deutsche Ärztezeitung, 135 DaVinci® systems (Intuitive Surgical, Inc., Sunnyvale, CA, USA) were in clinical use in Germany in 2019, although (co-)use by gynecologists was not reported specifically [37]. Traditionally, urology is considered to be a pioneering discipline in the use of robotic surgery [38]. The members of AGE, a specialist society that concentrates on conventional laparoscopic operations and is composed mainly of surgeons versed in this technique, may lack robotic surgical expertise, contributing to their reluctance to use robotic surgery.
Advantages of robotic surgery over conventional laparotomy that are shared with those of conventional laparoscopy are reduced blood loss, operation time, postoperative pain, and hospitalization [39]. Advantages of robotic surgery over conventional laparoscopy are the more ergonomic working position and reduced fatigue rate for surgeons, free mobility of the instruments in seven degrees of freedom, and digital networking of surgical robots [40].
The current S3 guidelines for ovarian malignancies do not mention robotic surgery, and recommend laparoscopic staging only in the research context, due to the lack of sufficient high-quality evidence [10]. This coincides with AGE members’ perspectives that further studies of robotic surgery in the gynecological context are needed, and their willingness to participate in such studies. It also corresponds to the state of the literature. For example, Yim et al. [41] found in a review that the majority of studies of the use of robotic surgery for the treatment of gynecological malignancies were retrospective or descriptive. Thus, prospective randomized studies of the application of this technique, at least to T1/2 ovarian tumors, appear to be needed [42].
The United States’ National Comprehensive Cancer Network guidelines mention only the use of conventional laparoscopy by experienced surgeons for the primary treatment of T1a–c tumors; they recommend the use of a minimally invasive access route for intermittent tumor debulking, with possible intraoperative conversion to open surgery via an abdominal incision [43]. This less cautious approach to the use of MIS for ovarian cancer treatment, which is based on greater experience and more widespread practice, is also reflected in the current literature from the United States. Two retrospective studies showed that robotic surgery was equivalent to conventional laparotomy. Feuer et al. [44] described equivalent tumor reduction (73% and 50%) and 1-year recurrence and survival rates (97% and 90%), regardless of tumor stage. Magrina et al. [45] observed no difference in overall survival after conventional laparoscopy (75%), robotic surgery (67%), and laparotomy (66%). However, these studies were conducted with very small patient cohorts (n = 89 and 75, respectively) and only 1-year follow-up periods.
In surveys, members of the Society of Gynecologic Oncology (SGO) reported positive attitudes toward and current implementation of robotic surgery in practice [46, 47]. The data revealed the increased use of robotic surgery to treat uterine malignancies and ovarian cancer (especially in the early stages). In one survey, 66% of respondents wished to increase the use of robotic surgery in the future [46]. In the other survey, 97% of respondents reported the use of robotic surgery, especially for the treatment of cervical and endometrial cancers [47]. In agreement with the AGE respondents, the SGO respondents favored additional research on the use of robotic surgery to treat ovarian tumors [46]. The more widespread use of robotic surgery in the Anglo-American region than in Germany may be due, among other factors, to differences in the remuneration system. In 2019, for example, a large portion of radical hysterectomies was performed robotically [37].
Limitations of the present study include the low response rate and the selection bias generated by surveying exclusively (laparoscopy-favoring) AGE members. Future surveys on the use of robotic surgery for ovarian tumor treatment should be conducted with larger and more diverse groups. Another limiting factor was the lack of reliable data on surgical robot use in German gynecological hospitals, which prevented, for example, determination of the ratio of respondents using robotic surgery to the number of robots present in their facilities. The collection of precise data on the quantity and distribution of surgical robots in Germany is crucial for subsequent surveys. A limitation of the present work is the imprecision of the question about the concerns regarding the oncologic safety of robotic surgery as, this question related to MIC in general and did not distinguish between robotic and laparoscopic surgery. Interpreting the results, we must consider the fact that the survey was carried out in 2015. Given the rapid progress in the surgical field, especially in terms of the use of MIS, a limitation of the present study could be the modified opinion of the AGE members regarding the use of robotic surgery in 2020.
Conclusion
The present survey should give an impression of the current tendencies of German AGE members (albeit in a laparoscopic oriented group) and the current practice in German hospitals. Prospective randomized studies on the therapy of T1/2 ovarian tumors as well as borderline tumors of the ovary should be implemented according to the results of this survey.
Giving the current evidence, robotic surgery for the treatment of ovarian malignancies should only be performed on selected patients within clinical studies.
Availability of data and material
The dataset used and analyzed during the current study is available from the corresponding author on reasonable request.
Change history
17 July 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00404-021-06136-1
References
Siegel RL, Miller KD, Jemal A (2016) Cancer statistics. CA Cancer J Clin 66:7–30. https://doi.org/10.3322/caac.21442
Robert Koch-Institut (Hrsg) und die Gesellschaft der epidemiologischen Krebsregister in Deutschland e.V. (Hrsg) (2020) Krebs in Deutschland 2015/2016. 12. Ausgabe. Im Internet: www.krebsdaten.de/Krebs/DE/Content/Publikationen/Krebs_in_Deutschland/kid_2019/krebs_in_deutschland_2019.pdf?__blob=publicationFile. Accessed 06 Jan 2020. https://doi.org/10.25646/5977
Bristow RE, Tomacruz SR, Armstrong DK et al (2002) Survival effect of maximal cytoreductive surgery for advanced ovarian carcinoma during the platinum era: a meta-analysis. J Clin Oncol 20:1248–1259. https://doi.org/10.1200/JCO.2002.20.5.1248
Elattar A, Bryant A, Winter-Roach BA et al (2011) Optimal primary surgical treatment for advanced epithelial ovarian cancer. Cochrane Database Syst Rev 10:CD007565. https://doi.org/10.1002/14651858.CD007565.pub2
Cho JE, Liu C, Gossner G et al (2009) Laparoscopy and gynecologic oncology. Clin Obstet Gynelcol 52:313–326. https://doi.org/10.1097/GRF.0b013e3181b088d2
Jernigan AM, Auer M, Fader AN et al (2012) Minimally invasive surgery in gynecologic oncology: a review of modalities and the literature. Womens Health (Lond) 8:239–250. https://doi.org/10.2217/whe.12.13
Park HJ, Kim DW, Yim GW et al (2013) Staging laparoscopy for the management of early stage ovarian cancer: a meta-analysis. Am J Obstet Gynecol 209(58):e1-8. https://doi.org/10.1016/j.ajog.2013.04.013
Sjovall K, Nilsson B, Einhorn N (1994) Different types of rupture of the tumor capsule and the impact of survival in early ovarian carcinoma. Int J Gynecol Cancer 4:333–336. https://doi.org/10.1046/j.1525-1438.1994.04050333.x
Zivanovic O, Sonoda Y, Diaz JP et al (2008) The rate of port-site metastases after 2251 laparoscopic procedures in women with underlying malignant disease. Gynecol Oncol 111:431–437. https://doi.org/10.1016/j.ygyno.2008.08.024
Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF (2020) Leitlinienprogramm Onkologie S3-Leitlinie Diagnostik, Therapie und Nachsorge maligner Ovarialtumoren, Langversion 1.0, Version 4.01- November 2019. Im Internet: www.leitlinienprogramm-onkologie.de/fileadmin/user_upload/Downloads/Leitlinien/Ovarialkarzinom/Version_4/LL_Ovarialkarzinom_Langversion_4.01.pdf. Accessed 06 Jan 2020
Fagotti A, Fanfani F, Vizzielli G et al (2010) Should laparoscopy be included in the work-up of advanced ovarian cancer patients attempting interval debulking surgery? Gynecol Oncol 116:72–77. https://doi.org/10.1016/j.ygyno.2009.09.015
Fagotti A, Perelli F, Pedone L et al (2016) Current recommendations for minimally invasive surgical staging in ovarian cancer. Curr Treat Options Oncol 17:3. https://doi.org/10.1007/s11864-015-0379-8
Park JY, Kim DY, Suh DS et al (2008) Comparison of laparoscopy and laparotomy in surgical staging of early-stage ovarian and fallopian tubal cancer. Ann Surg Oncol 15:2012–2019. https://doi.org/10.1245/s10434-008-9893-2
Radosa JC, Radosa MP, Schweitzer PA et al (2018) Report of the survey on current opinions and practice of German Society for Gynecologic Endoscopy (AGE) members regarding the laparoscopic treatment of ovarian malignancies. Arch Gynecol Obstet 297:1255–1264. https://doi.org/10.1007/s00404-018-4709-5
Brierley J, Gospodarowicz MK, Wittekind C (2017) TNM classification of malignant tumours, 8th edn. Wiley, Chichester, West Sussex, Hoboken. https://doi.org/10.1002/9780471420194
Lucidi A, Chiantera V, Gallotta V et al (2017) Role of robotic surgery in ovarian malignancy. Best Pract Res Clin Obstet Gynaecol 45:74–82. https://doi.org/10.1016/j.bpobgyn.2017.05.005
Bellia A, Vitale SG, Laganà AS et al (2016) Feasibility and surgical outcomes of conventional and robot-assisted laparoscopy for early-stage ovarian cancer: a retrospective, multicenter analysis. Arch Gynecol Obstet 294:615–622. https://doi.org/10.1007/s00404-016-4087-9
Yao Y, Li X, Yang Y et al (2015) Robotic surgery in the management of early ovarian malignancy tumors. Zhonghua Fu Chan Ke Za Zhi 50:603–607
Gallotta V, Cicero C, Conte C et al (2017) Robotic versus laparoscopic staging for early ovarian cancer: a case-matched control study. J Minim Invasive Gynecol 24:293–298. https://doi.org/10.1016/j.jmig.2016.11.004
Minig L, Padilla Iserte P, Zorrero C et al (2016) Robotic surgery in women with ovarian cancer: surgical technique and evidence of clinical outcomes. J Minim Invasive Gynecol 23:309–316. https://doi.org/10.1016/j.jmig.2015.10.014
Mäenpää MM, Nieminen K, Tomás El et al (2016) Robotic-assisted vs traditional laparoscopic surgery for endometrial cancer: a randomized controlled trial. Am J Obstet Gynecol 215:588.e1-588.e7. https://doi.org/10.1016/j.ajog.2016.06.005
El Khouly NI, Barr RL, Kim BB et al (2014) Comparison of robotic-assisted and conventional laparoscopy in the management of adnexal masses. J Minim Invasive Gynecol 21:1071–1074. https://doi.org/10.1016/j.jmig.2014.05.007
Nezhat FR, Finger TN, Vetere P et al (2014) Comparison of perioperative outcomes and complication rates between conventional versus robotic-assisted laparoscopy in the evaluation and management of early, advanced, and recurrent stage ovarian, fallopian tube, and primary peritoneal cancer. Int J Gynecol Cancer 24:600–607. https://doi.org/10.1097/IGC.0000000000000096
de la Cuesta SR, Goff BA, Fuller AF Jr et al (1994) Prognostic importance of intraoperative rupture of malignant ovarian epithelial neoplasms. Obstet Gynecol 84:1–7
Bakkum-Gamez JN, Richardson DL, Seamon LG et al (2009) Influence of intraoperative capsule rupture on outcomes in stage I epithelial ovarian cancer. Obstet Gynecol 113:11–17. https://doi.org/10.1097/AOG.0b013e3181917a0c
Kim HS, Ahn JH, Chung HH et al (2013) Impact of intraoperative rupture of the ovarian capsule on prognosis in patients with early-stage epithelial ovarian cancer: a meta-analysis. Eur J Surg Oncol 39:279–289. https://doi.org/10.1016/j.ejso.2012.12.003
Wildbrett P, Oh A, Naundorf D et al (2003) Impact of laparoscopic gases on peritoneal microenvironment and essential parameters of cell function. Surg Endosc 17:78–82
Smidt VJ, Singh DM, Hurteau JA et al (2001) Effect of carbon dioxide on human ovarian carcinoma cell growth. Am J Obstet Gynecol 185:1314–1317
Lee M, Kim SW, Paek J et al (2011) Comparisons of surgical outcomes, complications, and costs between laparotomy and laparoscopy in early-stage ovarian cancer. Int Gynecol Cancer 21:251–256. https://doi.org/10.1097/IGC.0b013e318208c71c
Ghezzi F, Malzoni M, Vizza E et al (2012) Laparoscopic staging of early ovarian cancer: results of a multi-institutional cohort study. Ann Surg Oncol 19:1589–1594. https://doi.org/10.1245/s10434-011-2138-9
Possover M, Krause N, Plaul K et al (1998) Laparoscopic para-aortic and pelvic lymphadenectomy: experience with 150 patients and review of the literature. Gynecol Oncol 71:19–28
Seror J, Bats AS, Bensaïd C et al (2015) Risk of port site metastases in pelvic cancers after robotic surgery. Eur J Surg Oncol 41:599–603. https://doi.org/10.1016/j.ejso.2015.01.003
Rindos N, Curry CL, Tabbarah R et al (2014) Port-site metastases after robotic surgery for gynecologic malignancy. J Soc Lap Surg 18:66–70. https://doi.org/10.4293/108680813X13693422519271
Ramirez PT, Wolf JK, Levenback C (2003) Laparoscopic port-site metastases: etiology and prevention. Gynecol Oncol 91:179–189
Kristensen SE, Mosgaard BJ, Rosendahl M et al (2017) Robot-assisted surgery in gynecological oncology: current status and controversies on patient benefits, cost and surgeon conditions - a systematic review. Acta Obstet Gynecol Scand 963:274–285. https://doi.org/10.1111/aogs.13084
Alkatout I, Mettler L, Maass N et al (2016) Robotic surgery in gynecology. J Turk Ger Gynecol Assoc 17:224–232. https://doi.org/10.5152/jtgga.2016.16187
https://www.aerztezeitung.de/Medizin/Zitterfreies-Operieren-mit-dem-Roboter-253634.html. Accessed 6 Jan 2020
Challacombe BJ, Khan MS, Murphy D et al (2006) The history of robotics in urology. World J Urol 24:120–127. https://doi.org/10.1007/s00345-006-0067-1
Chen CH, Chiu LH, Chen HH et al (2016) Comparison of robotic approach, laparoscopic approach and laparotomy in treating epithelial ovarian cancer. Int J Med Robot 12:268–275. https://doi.org/10.1002/rcs.1655
Alkatout I, Holthaus B, Wedel T et al (2018) Entwicklung der minimal-invasiven Chirurgie in der Gynäkologie und Überwindung assoziativer Herausforderungen. Gynäkologe 51:737–743. https://doi.org/10.1007/s00129-018-4292-7
Yim GW, Kim YT (2012) Robotic surgery in gynecologic cancer. Curr Opin Obstet Gynecol 24:14–23. https://doi.org/10.1097/GCO.0b013e32834daebc
Zanagnolo V, Garbi A, Achilarre MT et al (2017) Robot-assisted surgery in gynecologic cancers. J Minim Invasive Gynecol 24:379–396. https://doi.org/10.1016/j.jmig.2017.01.006
Armstrong DK, Alvarez RD, Bakkum-Gamez JN (2019) NCCN guidelines insights: Ovarian Cancer, Version 1. 2019. J Natl Compr Canc Netw 17:896–909. https://doi.org/10.6004/jnccn.2019.0039
Feuer GA, Lakhi N, Barker J (2013) Perioperative and clinical outcomes in the management of epithelial ovarian cancer using a robotic or abdominal approach. Gynecol Oncol 131:520–524. https://doi.org/10.1016/j.ygyno.2013.09.022
Magrina JF, Zanagnolo V, Noble BN (2011) Robotic approach for ovarian cancer: perioperative and survival results and comparison with laparoscopy and laparotomy. Gynecol Oncol 121:100–105. https://doi.org/10.1016/j.ygyno.2010.11.045
Mabrouk M, Frumovitz M, Greer M et al (2009) Trends in laparoscopic and robotic surgery among gynecologic oncologists: a survey update. Gynecol Oncol 112:501–505. https://doi.org/10.1016/j.ygyno.2008.11.037
Conrad LB, Ramirez PT, Burke W et al (2015) Role of minimally invasive surgery in gynecologic oncology: An updated survey of members of the society of gynecologic oncology. Int J Gynecol Cancer 25:1121–1127. https://doi.org/10.1097/IGC.0000000000000450
Funding
Open Access funding enabled and organized by Projekt DEAL. The study has been sponsored by the German Society for Gynecologic Endoscopy (AGE) (Grant no. 01/15).
Author information
Authors and Affiliations
Contributions
JSMZ: data analysis, data management, manuscript writing, and manuscript editing. JCR: project development, data collection, data analysis, and manuscript editing. MPR: project development, and data analysis. PS: manuscript editing. PAS: data management, and data analysis. EFS: project development and manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest statement
The authors declare no conflict of interest regarding the submitted work. Regarding interactions outside the submitted work, JCR has received travel grants from Medac GmbH (Wedel, Germany), Gedeon Richter (Budapest, Hungary), and Celgene (Summit, USA), Daiichi Sankyo (Tokio, Japan), Pfizer (New York City, USA) and was an honorary speaker for Pfizer (New York City, USA) in the past. EFS is receiving grants from the University of Saarland, Storz, and Erbe; personal fees and other compensation from Roche (Basel, Switzerland), Pfizer (New York City, USA), Celgene (Summit USA), Amgen (Thousand Oaks, USA), and Astra Zeneca (Cambridge, GB); other fees from Johnson & Johnson (New Brunswick, USA), Novartis (Basel, Switzerland), Tesaro (Waltham, USA), Medac GmbH (Wedel, Germany), MSD (Kenilworth, USA), Vifor (Sankt Gallen, Switzerland), Gedeon Richter (Budapest, Hungary), Takeda (Tokyo, Japan), and AGE (Buchholz, Germany) outside the submitted work.
Ethics approval
According to the local ethics committee regulations (Saarland institutional review board), no ethical approval was needed for this survey.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to a retrospective Open Access order.
Rights and permissions
This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zimmermann, J.S.M., Radosa, J.C., Radosa, M.P. et al. Survey of current practices and opinions of German Society of Gynecologic Endoscopy members regarding the treatment of ovarian neoplasia by robotic surgery. Arch Gynecol Obstet 303, 1305–1313 (2021). https://doi.org/10.1007/s00404-020-05876-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05876-w