Abstract
Purpose
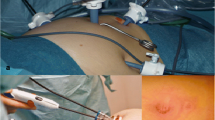
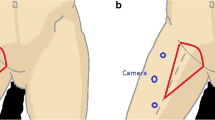
Laparoendoscopic single-site surgery (LESS), a promising innovation in minimally invasive surgery, has been used in treating gynecologic oncology diseases. There have been no reports in the literature regarding LESS for inguinal lymphadenectomy (LESS-IL) in gynecologic conditions. We aimed to evaluate the feasibility, safety, and outcomes of LESS-IL.
Methods
Six patients with vulvar or vaginal cancer underwent LESS-IL from July 2018 to March 2019. Data regarding the intraoperative and postoperative outcomes were analyzed.
Results
All patients successfully underwent a bilateral LESS-IL without conversion. LESS pelvic lymphadenectomy via an umbilical incision was also performed in a patient with vaginal cancer. The median operation time for the single-port laparoendoscopic inguinal lymphadenectomies was 105 min (range 70–134), with a median estimated blood loss of 108 ml (range 40–170). Median time of hospitalization was 7.5 days (range 5–10). A median of 11 (6–15) lymph nodes were dissected in a unilateral groin. The suction drains were removed after a median duration of 5 days (range 3–7). There were no skin-related or lymph-related postoperative complications. At a median follow-up period of 9 months, all the patients were alive and no recurrence was found.
Conclusion
LESS-IL is a feasible and safe technique for the surgical management of gynecologic cancers.


Similar content being viewed by others
References
Jakub JW, Reintgen DS, Shivers S, Pendas S (2007) Regional node dissection for melanoma: techniques and indication. Surg Oncol Clin N Am 16(1):247–261
Roiner M, Maurer O, Lebentrau S, Gilfrich C, Schafer C, Haberl C et al (2018) Management of penile cancer patients: new aspects of a rare tumour entity. Aktuelle Urol 49(3):242–249
Woelber L, Kock L, Gieseking F, Petersen C, Trillsch F, Choschzick M et al (2011) Clinical management of primary vulvar cancer. Eur J Cancer 47(15):2315–2321
Gaarenstroom KN, Kenter GG, Trimbos JB, Agous I, Amant F, Peters AA et al (2003) Postoperative complications after vulvectomy and inguinofemoral lymphadenectomy using separate groin incisions. Int J Gynecol Cancer 13(4):522–527
Goker A, Guvenal T, Yanikkerem E, Turhan A, Koyuncu FM (2011) Quality of life in women with gynecologic cancer in Turkey. Asian Pac J Cancer Prev 12(11):3121–3128
Rouzier R, Haddad B, Dubernard G, Dubois P, Paniel BJ (2003) Inguinofemoral dissection for carcinoma of the vulva: effect of modifications of extent and technique on morbidity and survival. J Am Coll Surg 196(3):442–450
Cirik DA, Karalok A, Ureyen I, Tasci T, Kalyoncu R, Turkmen O et al (2015) Early and late complications after inguinofemoral lymphadenectomy for vulvar cancer. Asian Pac J Cancer Prev 16(13):5175–5179
Le A, Xiong J, Wang Z, Dai XY, Xiao TH, Zhuo R et al (2018) Endoscopy-assisted inguinal lymphadenectomy in vulvar cancer. Arch Gynecol Obstet 297(5):1277–1283
Postlewait LM, Farley CR, Diller ML, Martin B, Hart Squires M III, Russell MC et al (2017) A minimally invasive approach for inguinal lymphadenectomy in melanoma and genitourinary malignancy: long-term outcomes in an attempted randomized control trial. Ann Surg Oncol 24(11):3237–3244
Fagotti A, Boruta DM 2nd, Scambia G, Fanfani F, Paglia A, Escobar PF (2012) First 100 early endometrial cancer cases treated with laparoendoscopic single-site surgery: a multicentric retrospective study. Am J Obstet Gynecol 206(4):353.e351–356
Buenafe AAE, Lee-Ong AC (2017) Laparoendoscopic single-site surgery in inguinal hernia repair. Asian J Endosc Surg 10(3):244–251
Nomura T, Takei K, Abe S, Fukuda Y, Yamanaka N, Sejiyama S et al (2017) Patient-reported postoperative pain, body image, and cosmetic satisfaction after transumbilical laparoendoscopic single-site adrenalectomy. Asian J Endosc Surg 10(3):289–294
Paek J, Nam EJ, Kim YT, Kim SW (2011) Overcoming technical difficulties with single-port access laparoscopic surgery in gynecology: using conventional laparoscopic instruments. J Laparoendosc Adv Surg Tech A 21(2):137–141
Tobias-Machado M, Correa WF, Reis LO, Starling ES, de Castro NO, Juliano RV et al (2011) Single-site video endoscopic inguinal lymphadenectomy: initial report. J Endourol 25(4):607–610
Yuan JB, Chen MF, Qi L, Li Y, Li YL, Chen C et al (2015) Preservation of the saphenous vein during laparoendoscopic single-site inguinal lymphadenectomy: comparison with the conventional laparoscopic technique. BJU Int 115(4):613–618
(2009) Current FIGO staging for cancer of the vagina, fallopian tube, ovary, and gestational trophoblastic neoplasia. Int J Gynaecol Obstet 105(1):3–4
Pecorelli S (2009) Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet 105(2):103–104
Adams TS, Cuello MA (2018) Cancer of the vagina. Int J Gynaecol Obstet 143(Suppl 2):14–21
Rogers LJ, Cuello MA (2018) Cancer of the vulva. Int J Gynaecol Obstet 143(Suppl 2):4–13
Serpell JW, Carne PW, Bailey M (2003) Radical lymph node dissection for melanoma. ANZ J Surg 73(5):294–299
Walker KF, Day H, Abu J, Nunns D, Williamson K, Duncan T (2011) Do surgical techniques used in groin lymphadenectomy for vulval cancer affect morbidity rates? Int J Gynecol Cancer 21(8):1495–1499
Coblentz TR, Theodorescu D (2002) Morbidity of modified prophylactic inguinal lymphadenectomy for squamous cell carcinoma of the penis. J Urol 168(4 Pt 1):1386–1389
Pouwer AW, Hinten F, van der Velden J, Smolders RGV, Slangen BFM, Zijlmans H et al (2017) Volume-controlled versus short drainage after inguinofemoral lymphadenectomy in vulvar cancer patients: a Dutch nationwide prospective study. Gynecol Oncol 146(3):580–587
Pontre J, Harding J, Chivers P, Loughlin L, Leung Y, Salfinger SG et al (2018) Do groin drains reduce postoperative morbidity in women undergoing inguinofemoral lymphadenectomy for vulvar cancer? Int J Gynecol Cancer 28(1):183–187
van Beekhuizen HJ, Auzin M, van den Einden LC, de Hullu JA, van der Velden J, Wildhagen MF et al (2014) Lymph node count at inguinofemoral lymphadenectomy and groin recurrences in vulvar cancer. Int J Gynecol Cancer 24(4):773–778
Butler JS, Milliken DA, Dina R, Eccles SA, Maghami SG, Jameson C et al (2010) Isolated groin recurrence in vulval squamous cell cancer (VSCC). The importance of node count. Eur J Gynaecol Oncol 31(5):510–513
Baiocchi G, Cestari FM, Rocha RM, Faloppa CC, Kumagai LY, Fukazawa EM et al (2013) Does the count after inguinofemoral lymphadenectomy in vulvar cancer correlate with outcome? Eur J Surg Oncol 39(4):339–343
Diehl A, Volland R, Kirn V, Thangarajah F, Eichler C, Einzmann T et al (2016) The number of removed lymph nodes by inguinofemoral lymphadenectomy: impact on recurrence rates in patients with vulva carcinoma. Arch Gynecol Obstet 294(1):131–136
Polterauer S, Schwameis R, Grimm C, Hillemanns P, Juckstock J, Hilpert F et al (2019) Lymph node ratio in inguinal lymphadenectomy for squamous cell vulvar cancer: results from the AGO-CaRE-1 study. Gynecol Oncol 153(2):286–291
Funding
This work was supported by National Natural Science Foundation of China (no. 81673130).
Author information
Authors and Affiliations
Contributions
JYX: project development, data collection, data analysis, manuscript writing. KD: acquisition of data, data analysis, manuscript writing. XMG: data collection, drafting of manuscript and/or critical revision. BD: acquisition of data, data analysis. XYZ: data analysis, manuscript writing and/or critical revision. MLR: drafting of manuscript and/or critical revision. YS: project development, data collection, approval of final version of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest and nothing to disclose.
Ethical approval
This work was approved by the ethics committee of the affiliated hospital of southeast university (no. 2018ZDSYLL150-P01).
Informed consent
The work was conducted with the patients' informed consent, a signed consent form was obtained from each patient.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xu, J., Duan, K., Guan, X. et al. Laparoendoscopic single-site inguinal lymphadenectomy in gynecology: preliminary experience at a single institution. Arch Gynecol Obstet 302, 497–503 (2020). https://doi.org/10.1007/s00404-020-05649-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05649-5