Abstract
Background
International Federation of Gynecology and Obstetrics (FIGO) grade is a crucial factor in the current system for the risk stratification of endometrial endometrioid carcinoma (EC). The Cancer Genome Atlas (TCGA) demonstrated four molecular prognostic subgroups for EC: POLE (good prognosis), microsatellite-instable (MSI, intermediate prognosis), copy-number-high (CNH, poor prognosis), and copy-number-low (CNL, variable prognosis).
Objective
To assess how the prevalence of the TCGA molecular subgroups changes from low-grade (G1-2) to high-grade (G3) EC, to understand how it may affect the current risk-assessment system.
Methods
A systematic review and meta-analysis was carried out by searching seven electronic databases from January 2013 to September 2019 for studies assessing the TCGA classification G1–2 and G3 EC. Pooled prevalence of the TCGA subgroups was calculated in EC. The association of each subgroup with grade was assessed using odds ratio (OR), with a significant p value < 0.05.
Results
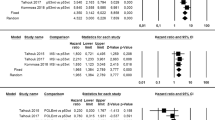
Nine studies with 3185 patients were included. G3 EC showed significantly higher prevalence of the POLE subgroup (12.1% vs 6.2%; OR = 2.13; p = 0.0001), of the MSI subgroup (39.7% vs 24.7%; OR = 2.15; p = 0.0003) and of the CNH subgroup (21.3% vs 4.7%; OR = 5.25; p < 0.00001), and significantly lower prevalence of the CNL subgroup (28% vs 63.5%; OR = 0.2; p < 0.00001) than G1–2 EC.
Conclusion
The prevalence of the TCGA subgroups is not in accordance with the prognostic value of FIGO grade, indicating that the current risk stratification of EC will be heavily affected by molecular signature.



Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A (2015) Cancer statistics, 2015. CA Cancer J Clin. 65:5–29
Raffone A, Travaglino A, Mascolo M et al (2019) TCGA molecular groups of endometrial cancer: pooled data about prognosis. Gynecol Oncol. https://doi.org/10.1016/j.ygyno.2019.08.019(Epub ahead of print)
Gilks CB, Oliva E, Soslow RA (2013) Poor interobserver reproducibility in the diagnosis of high-grade endometrial carcinoma. Am J Surg Pathol 37:874–881
Hoang LN, McConechy MK, Kobel M et al (2013) Histotype-genotype correlation in 36 high-grade endometrial carcinomas. Am J Surg Pathol 37:1421–1432
Talhouk A, McConechy MK, Leung S et al (2015) A clinically applicable molecular-based classification for endometrial cancers. Br J Cancer 113:299–310
Talhouk A, McConechy MK, Leung S et al (2017) Confirmation of ProMisE: a simple, genomics-based clinical classifier for endometrial cancer. Cancer 123(5):802–813
Kommoss S, McConechy MK, Kommoss F et al (2018) Final validation of the ProMisE molecular classifier for endometrial carcinoma in a large population-based case series. Ann Oncol 29(5):1180–1188
Cancer Genome Atlas Research Network et al (2013) Integrated genomic characterization of endometrial carcinoma. Nature 497:67–73
Stelloo E, Bosse T, Nout RA et al (2015) Refining prognosis and identifying targetable pathways for high-risk endometrial cancer; a TransPORTEC initiative. Mod Pathol 28(6):836–844
Stelloo E, Nout RA, Osse EM et al (2016) Improved risk assessment by integrating molecular and clinicopathological factors in early-stage endometrial cancer-combined analysis of the PORTEC cohorts. Clin Cancer Res 22(16):4215–4224
Bosse T, Nout RA, McAlpine JN et al (2018) Molecular classification of grade 3 endometrioid endometrial cancers identifies distinct prognostic subgroups. Am J Surg Pathol 42(5):561–568
Cosgrove CM, Tritchler DL, Cohn DE et al (2018) An NRG oncology/GOG study of molecular classification for risk prediction in endometrioid endometrial cancer. Gynecol Oncol 148(1):174–180
Prendergast EN, Holman LL, Liu AY et al (2019) Comprehensive genomic profiling of recurrent endometrial cancer: implications for selection of systemic therapy. Gynecol Oncol 154(3):461–466
Sherman ME (2000) Theories of endometrial carcinogenesis: a multidisciplinary approach. Mod Pathol 13:295–308
Travaglino A, Raffone A, Saccone G et al (2019) Immunophenotype of atypical polypoid adenomyoma of the uterus: diagnostic value and insight on pathogenesis. Appl Immunohistochem Mol Morphol. https://doi.org/10.1097/PAI.0000000000000780
Raffone A, Travaglino A, Saccone G et al (2019) Should progesterone and estrogens receptors be assessed for predicting the response to conservative treatment of endometrial hyperplasia and cancer? A systematic review and meta-analysis. Acta Obstet Gynecol Scand 98:976–987
Travaglino A, Raffone A, Saccone G et al (2019) PTEN immunohistochemistry in endometrial hyperplasia: which are the optimal criteria for the diagnosis of precancer? APMIS 127:161–169
Raffone A, Travaglino A, Saccone G et al (2019) PTEN expression in endometrial hyperplasia and risk of cancer: a systematic review and meta-analysis. Arch Gynecol Obstet 299:1511–1524
Moher D, Shamseer L, Clarke M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1
Whiting PF, Rutjes AW, Westwood ME et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155(8):529–536
Travaglino A, Raffone A, Saccone G et al (2019) Immunohistochemical predictive markers of response to conservative treatment of endometrial hyperplasia and early endometrial cancer: a systematic review. Acta Obstet Gynecol Scand 98:1086–1099
Raffone A, Travaglino A, Saccone G et al (2019) Diagnostic and prognostic value of ARID1A in endometrial hyperplasia: a novel marker of occult cancer. APMIS 127:597–606
Travaglino A, Raffone A, Saccone G et al (2019) Nuclear expression of β-catenin in endometrial hyperplasia as marker of premalignancy. APMIS. https://doi.org/10.1111/apm.12988(Epub ahead of print)
Travaglino A, Raffone A, Mascolo M et al (2019) Clear cell endometrial carcinoma and the TCGA classification. Histopathology. https://doi.org/10.1111/his.13976(Epub ahead of print)
Travaglino A, Raffone A, Saccone G et al (2019) Significant risk of occult cancer in complex non-atypical endometrial hyperplasia. Arch Gynecol Obstet 300(5):1147–1154
Travaglino A, Raffone A, Mascolo M et al (2019) TCGA molecular subgroups in endometrial undifferentiated/dedifferentiated carcinoma. Pathol Oncol Res. https://doi.org/10.1007/s12253-019-00784-0(Epub ahead of print)
Travaglino A, Raffone A, Saccone G et al (2019) Congruence between 1994 WHO classification of endometrial hyperplasia and endometrial intraepithelial neoplasia system. Am J Clin Pathol. https://doi.org/10.1093/ajcp/aqz132(Epub ahead of print)
Raffone A, Travaglino A, Santoro A et al (2019) Accuracy of one-step nucleic acid amplification in detecting lymph node metastases in endometrial cancer. Pathol Oncol Res. https://doi.org/10.1007/s12253-019-00727-9(Epub ahead of print)
Raffone A, Travaglino A, Saccone G et al (2019) Diabetes mellitus and responsiveness of endometrial hyperplasia and early endometrial cancer to conservative treatment. Gynecol Endocrinol. https://doi.org/10.1080/09513590.2019.1624716(Epub ahead of print)
Raffone A, Travaglino A, Saccone G et al (2019) Diabetes mellitus is associated with occult cancer in endometrial hyperplasia. Pathol Oncol Res. https://doi.org/10.1007/s12253-019-00684-3(Epub ahead of print)
Travaglino A, Raffone A, Saccone G et al (2019) Complexity of glandular architecture should be reconsidered in the classification and management of endometrial hyperplasia. APMIS 127:427–434
Hoang LN, Kinloch MA, Leo JM et al (2017) Interobserver agreement in endometrial carcinoma histotype diagnosis varies depending on the cancer genome atlas (TCGA)-based molecular subgroup. Am J Surg Pathol 41(2):245–252
Karnezis AN, Leung S, Magrill J et al (2017) Evaluation of endometrial carcinoma prognostic immunohistochemistry markers in the context of molecular classification. J Pathol Clin Res 3(4):279–293
Auguste A, Genestie C, De Bruyn M et al (2018) Refinement of high-risk endometrial cancer classification using DNA damage response biomarkers: a TransPORTEC initiative. Mod Pathol 31:1851–1861
Talhouk A, Derocher H, Schmidt P et al (2019) Molecular subtype not immune response drives outcomes in endometrial carcinoma. Clin Cancer Res 25(8):2537–2548
Britton H, Huang L, Lum A et al (2019) Molecular classification defines outcomes and opportunities in young women with endometrial carcinoma. Gynecol Oncol 153:487–495
Colombo N, Creutzberg C, Amant F et al (2016) ESMO-ESGO-ESTRO Consensus Conference on Endometrial Cancer diagnosis treatment and follow-up. Ann Oncol 27:16–41
Wortman BG, Bosse T, Nout RA et al (2018) Molecular-integrated risk profile to determine adjuvant radiotherapy in endometrial cancer: evaluation of the pilot phase of the PORTEC-4a trial. Gynecol Oncol 151:69–75
Moroney MR, Davies KD, Wilberger AC et al (2019) Molecular markers in recurrent stage I, grade 1 endometrioid endometrial cancers. Gynecol Oncol 153:517–520
Murali R, Davidson B, Fadare O et al (2019) High-grade endometrial carcinomas: morphologic and immunohistochemical features, diagnostic challenges and recommendations. Int J Gynecol Pathol 38(Suppl 1):S40–S63
Funding
No financial support was received for this study.
Author information
Authors and Affiliations
Contributions
AT, AR independently assessed electronic search, eligibility of the studies, inclusion criteria, risk of bias, data extraction and data analysis. Disagreements were resolved by discussion with AM, GB, PA, GFZ, LI and FZ. AM, GB and PA contributed to the elaboration of methods for risk of bias assessment, data extraction and analysis. AT, AR, AM, LI and FZ conceived the study; GB, PA, GFZ, LI and FZ worked on the design of the study; AT, AR, AM, GB, PA, GFZ, LI and FZ worked on the manuscript preparation; GFZ, LI and FZ supervised the whole study.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Travaglino, A., Raffone, A., Mollo, A. et al. TCGA molecular subgroups and FIGO grade in endometrial endometrioid carcinoma. Arch Gynecol Obstet 301, 1117–1125 (2020). https://doi.org/10.1007/s00404-020-05531-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05531-4