Abstract
Purpose
Antenatal corticosteroids have been shown to decrease neonatal respiratory morbidity in singleton pregnancies when given during the late-preterm period (340/7–366/7 weeks). Whether these findings also apply to late-preterm twins, who account for approximately one-third of infants born at 340/7–356/7 weeks, is currently unclear. The answer to this question depends, in part, on whether the risk of respiratory morbidity among late-preterm twin infants is similar to that observed in late-preterm singletons. We aimed to assess the rate of respiratory morbidity among late-preterm twin infants using a secondary analysis of prospectively collected data from a large international multicenter trial, and to compare that rate with previous studies that used the same definition of respiratory morbidity.
Study design
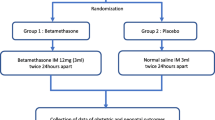
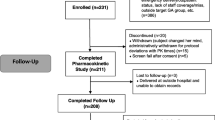
This was a secondary analysis of the twin birth study. In the current study, we limited the analysis to women who gave birth during the late preterm period. The primary outcomes were the same primary composite respiratory morbidity variables that were used in the randomized controlled trial of Gyamfi-Bannerman et al., on the administration of betamethasone during the late preterm period in singletons (ALPS trial). The risk of respiratory morbidity among late preterm twins was stratified by gestational week at birth.
Results
A total of 1163 women who gave birth to 2324 late preterm twin infants met the inclusion criteria. The rates of respiratory morbidity and severe respiratory morbidity were 16.5% and 8.9%, respectively. The risk of respiratory morbidity was highly dependent on gestational week at birth, being more than fourfold for infants born at 340/7–346/7 weeks (aOR 4.30, 95%–CI 3.01–6.14) and more than twofold for infants born at 350/7–356/7 weeks (aOR 2.12, 95%–CI 1.51–2.98) compared with infants born at 360/7–366/7 weeks. The rate of respiratory morbidity and the theoretical number of women needed to be treated with betamethasone to prevent a single case of respiratory morbidity in the current study were similar to those reported in the APLS trial (16.5% vs. 14.4%, p = 0.103, and NNT 31 vs. 34, respectively).
Conclusions
The risk–benefit ratio of betamethasone with regard to neonatal respiratory morbidity in women with twins at risk of late-preterm birth is expected to be similar to that observed in singletons.
Similar content being viewed by others
References
McIntire DD, Leveno KJ (2008) Neonatal mortality and morbidity rates in late preterm births compared with births at term. Obstet Gynecol 111(1):35–41. https://doi.org/10.1097/01.AOG.0000297311.33046.73
Hamilton BE, Martin JA, Osterman MJ, Curtin SC, Matthews TJ (2015) Births: final data for 2014. National vital statistics reports : from the centers for disease control and prevention, National center for health statistics. Natl vital statistics syst 64(12):1–64
Yoder BA, Gordon MC, Barth WH Jr (2008) Late-preterm birth: does the changing obstetric paradigm alter the epidemiology of respiratory complications? Obstet Gynecol 111(4):814–822. https://doi.org/10.1097/AOG.0b013e31816499f4
Consortium on Safe L, Hibbard JU, Wilkins I, Sun L, Gregory K, Haberman S, Hoffman M, Kominiarek MA, Reddy U, Bailit J, Branch DW, Burkman R, Gonzalez Quintero VH, Hatjis CG, Landy H, Ramirez M, VanVeldhuisen P, Troendle J, Zhang J (2010) Respiratory morbidity in late preterm births. JAMA 304(4):419–425. https://doi.org/10.1001/jama.2010.1015
Gyamfi-Bannerman C, Thom EA, Blackwell SC, Tita AT, Reddy UM, Saade GR, Rouse DJ, McKenna DS, Clark EA, Thorp JM Jr, Chien EK, Peaceman AM, Gibbs RS, Swamy GK, Norton ME, Casey BM, Caritis SN, Tolosa JE, Sorokin Y, VanDorsten JP, Jain L, Network NM-FMU (2016) Antenatal betamethasone for women at risk for late preterm delivery. N Engl J Med 374(14):1311–1320. https://doi.org/10.1056/NEJMoa1516783
American College of O, Gynecologists’ Committee on Obstetric P, Society for Maternal-Fetal M (2016) Antenatal corticosteroid therapy for fetal maturation. Obstetrics and gynecology 128(4):e187–e194. https://doi.org/10.1097/aog.0000000000001715 (Committee opinion no.677)
Society for maternal-fetal medicine publications c (2016) Implementation of the use of antenatal corticosteroids in the late preterm birth period in women at risk for preterm delivery. Am J Obstet Gynecol 215(2):B13–B15. https://doi.org/10.1016/j.ajog.2016.03.013
Nowik CM, Davies GA, Smith GN (2017) We should proceed with caution when it comes to antenatal corticosteroids after 34 weeks. J Obstet Gynecol Can 39(1):49–51. https://doi.org/10.1016/j.jogc.2016.05.011
Asztalos EV (2016) Antenatal corticosteroids are currently used excessively and more stringent controls on their use should be established: For: The use of antenatal corticosteroids should be restricted if we are to avoid causing harm. BJOG 123(11):1787. https://doi.org/10.1111/1471-0528.13968
Smith GC (2016) Antenatal betamethasone for women at risk for late preterm delivery. N Engl J Med 375(5):486. https://doi.org/10.1056/NEJMc1605902%23SA3
Jobe AH, Goldenberg RL (2018) Antenatal corticosteroids: an assessment of anticipated benefits and potential risks. Am J Obstet Gynecol 219(1):62–74. https://doi.org/10.1016/j.ajog.2018.04.007
Crowther CA, Harding JE (2016) Antenatal Glucocorticoids for Late Preterm Birth? N Engl J Med 374(14):1376–1377. https://doi.org/10.1056/NEJMe1601867
Refuerzo JS, Momirova V, Peaceman AM, Sciscione A, Rouse DJ, Caritis SN, Spong CY, Varner MW, Malone FD, Iams JD, Mercer BM, Thorp JM Jr, Sorokin Y, Carpenter MW, Lo J, Harper M, Eunice Kennedy Shriver National Institute of Child H, Human Development Maternal-Fetal Medicine Units N (2010) Neonatal outcomes in twin pregnancies delivered moderately preterm, late preterm, and term. Am J Perinatol 27(7):537–542. https://doi.org/10.1055/s-0030-1248940
Simchen MJ, Okrent Smolar AL, Dulitzky M, Sivan E, Morag I (2016) Neonatal morbidities and need for intervention in twins and singletons born at 34–35 weeks of gestation. J Perinat Med 44(8):887–892. https://doi.org/10.1515/jpm-2015-0113
Escobar GJ, McCormick MC, Zupancic JA, Coleman-Phox K, Armstrong MA, Greene JD, Eichenwald EC, Richardson DK (2006) Unstudied infants: outcomes of moderately premature infants in the neonatal intensive care unit. Arch Dis Child Fetal Neonatal Ed 91(4):F238–F244. https://doi.org/10.1136/adc.2005.087031
Raju TN, Higgins RD, Stark AR, Leveno KJ (2006) Optimizing care and outcome for late-preterm (near-term) infants: a summary of the workshop sponsored by the National Institute of Child Health and Human Development. Pediatrics 118(3):1207–1214. https://doi.org/10.1542/peds.2006-0018
Shapiro-Mendoza CK, Tomashek KM, Kotelchuck M, Barfield W, Weiss J, Evans S (2006) Risk factors for neonatal morbidity and mortality among “healthy,” late preterm newborns. Semin Perinatol 30(2):54–60. https://doi.org/10.1053/j.semperi.2006.02.002
Bastek JA, Sammel MD, Pare E, Srinivas SK, Posencheg MA, Elovitz MA (2008) Adverse neonatal outcomes: examining the risks between preterm, late preterm, and term infants. Am J Obstet Gynecol 199(4):367.e1. https://doi.org/10.1016/j.ajog.2008.08.002
Melamed N, Klinger G, Tenenbaum-Gavish K, Herscovici T, Linder N, Hod M, Yogev Y (2009) Short-term neonatal outcome in low-risk, spontaneous, singleton, late preterm deliveries. Obstet Gynecol 114(2 Pt 1):253–260. https://doi.org/10.1097/AOG.0b013e3181af6931
Friedman SA, Schiff E, Kao L, Kuint J, Sibai BM (1997) Do twins mature earlier than singletons? results from a matched cohort study. Am J Obstet Gynecol 176(6):1193–1196 (discussion 1196–1199)
Suzuki S, Inde Y, Miyake H (2010) Comparison of short-term outcomes of late pre-term singletons and dichorionic twins and optimal timing of delivery. J Obstet Gynecol 30(6):574–577. https://doi.org/10.3109/01443615.2010.494207
Wolfe K, Tabangin M, Meinzen-Derr J, Snyder C, Lewis D, DeFranco E (2014) Neonatal morbidity by week of gestational age for twins compared to singletons: a population-based cohort study. Am J Perinatol 31(2):133–138. https://doi.org/10.1055/s-0033-1341572
Ribicic R, Kranjcec I, Borosak J, Tumbri J, Mihovilovic Prajz L, Ribicic T (2016) Perinatal outcome of singleton versus twin late preterm infants: do twins mature faster than singletons? J maternal-fetal & neonatal Med 29(9):1520–1524. https://doi.org/10.3109/14767058.2015.1053449
Salem SY, Kibel M, Asztalos E, Zaltz A, Barrett J, Melamed N (2017) Neonatal Outcomes of Low-Risk, Late-Preterm Twins Compared With Late-Preterm Singletons. Obstet Gynecol 130(3):582–590. https://doi.org/10.1097/AOG.0000000000002187
Barrett JF, Hannah ME, Hutton EK, Willan AR, Allen AC, Armson BA, Gafni A, Joseph KS, Mason D, Ohlsson A, Ross S, Sanchez JJ, Asztalos EV, Twin Birth Study Collaborative G (2013) A randomized trial of planned cesarean or vaginal delivery for twin pregnancy. N Engl J Med 369(14):1295–1305. https://doi.org/10.1056/NEJMoa1214939
Jobe AH, Bancalari E (2001) Bronchopulmonary dysplasia. Am J Respir Crit Care Med 163(7):1723–1729. https://doi.org/10.1164/ajrccm.163.7.2011060
Papile LA, Burstein J, Burstein R, Koffler H (1978) Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1500 gm. Pediatrics 92(4):529–534
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, Brotherton T (1978) Neonatal necrotizing enterocolitis therapeutic decisions based upon clinical staging. Annals of surg 187(1):1–7
Melamed N, Shah J, Yoon EW, Pelausa E, Lee SK, Shah PS, Murphy KE, Canadian Neonatal Network I (2016) The role of antenatal corticosteroids in twin pregnancies complicated by preterm birth. Am J Obstet Gynecol 215(4):482–489. https://doi.org/10.1016/j.ajog.2016.05.037
Bender R (2001) Calculating confidence intervals for the number needed to treat. Control Clin Trials 22(2):102–110
McElrath TF, Norwitz ER, Robinson JN, Tanasijevic MJ, Lieberman ES (2000) Differences in TDx fetal lung maturity assay values between twin and singleton gestations. Am J Obstet Gynecol 182(5):1110–1112
Leveno KJ, Quirk JG, Whalley PJ, Herbert WN, Trubey R (1984) Fetal lung maturation in twin gestation. Am J Obstet Gynecol 148(4):405–411
Kramer MS, Platt RW, Wen SW, Joseph KS, Allen A, Abrahamowicz M, Blondel B, Breart G, Fetal/Infant Health Study Group of the Canadian Perinatal Surveillance S (2001) A new and improved population-based Canadian reference for birth weight for gestational age. Pediatrics 108(2):E35
Funding
Dr. Melamed holds the Waugh Family Chair in Twin Fetal Medicine Research at the Sunnybrook Health Sciences Center and the University of Toronto.
Author information
Authors and Affiliations
Contributions
DM: Protocol/project development, Manuscript writing/editing; JB: Protocol/project development, Manuscript writing/editing, Data collection or management; EM: Manuscript writing/editing; AZ: Manuscript writing/editing; NM: Protocol/project development, Manuscript writing/editing, Data collection or management.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Martinka, D., Barrett, J., Mei-dan, E. et al. Respiratory morbidity in late preterm twin infants. Arch Gynecol Obstet 300, 337–345 (2019). https://doi.org/10.1007/s00404-019-05191-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05191-z