Abstract
Background
In 2016, the American College of Obstetricians and Gynecologists recommended antenatal corticosteroids in the late preterm period for women at risk for preterm delivery. Limited real-world evidence exists on neonatal outcomes, particularly for twin gestations, following the guideline change. The study objective is to determine the association of antenatal corticosteroids in late preterm singleton and twin pregnancies with respiratory complications and hypoglycemia in a real-world clinical setting.
Methods
This is a retrospective cohort study comprising late preterm deliveries (4,341 mother–child pairs) within the Mount Sinai Health System, 2012–2018. The exposure of interest is antenatal corticosteroid administration of betamethasone during pregnancy between 34 0/7 and 36 6/7 weeks. Our primary outcomes are neonatal respiratory complications and hypoglycemia. Multivariable logistic regression was used to estimate the association between antenatal corticosteroid exposure and these two outcomes. We stratified the study population by singleton gestations and twins to minimize the potential confounding from different obstetric management between the two groups.
Results
Among a total of 4,341 mother–child pairs (3,309 singleton and 1,032 twin mother–child pairs), 745 mothers received betamethasone, of which 40.94% (305/745) received the full course. Relative to no treatment, a full course of betamethasone was associated with reduced odds of respiratory complications (OR = 0.53, 95% CI:[0.31–0.85], p < 0.01) and increased odds of hypoglycemia (OR = 1.86, 95%CI:[1.34–2.56], p < 0.01) in singletons; however, the association with respiratory complications was not significant in twins (OR = 0.42, 95% CI:[0.11–1.23], p = 0.16), but was associated with increased odds of hypoglycemia (OR = 2.18, 95% CI:[1.12–4.10], p = 0.02).
A partial course of betamethasone (relative to no treatment) was not significantly associated with any of the outcomes, other than respiratory complications in twins (OR = 0.34, 95% CI:[0.12–0.82], p = 0.02).
Conclusions
Exposure to antenatal corticosteroids in singletons and twins is associated with increased odds of hypoglycemia. Among singletons, exposure to the full dosage (i.e. two doses) was associated with decreased odds of respiratory complications but this was only the case for partial dose among twins. Twin gestations were not studied by the Antenatal Late Preterm Steroids trial. Therefore, our study findings will contribute to the paucity of evidence on the benefit of antenatal corticosteroids in this group. Health systems should systematically monitor guideline implementations to improve patient outcomes.
Similar content being viewed by others
Introduction
Antenatal corticosteroid (ACS) use has been widely supported in the United States (US) in pregnancies at risk for early preterm delivery (< 34 gestational weeks) to accelerate fetal lung maturation [1]. Benefits include reduced neonatal morbidity such as respiratory distress syndrome, intraventricular hemorrhage, neonatal intensive care unit (NICU) admission, as well as death [1, 2]. The Antenatal Late Preterm Steroids (ALPS) trial published in 2016 demonstrated that betamethasone use in singleton gestations in late preterm pregnancies (34–36 gestational weeks) at high risk for preterm delivery, significantly reduced the rate of neonatal respiratory complications, but increased the rate of neonatal hypoglycemia [3]. Consequently, since 2016, the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal–Fetal Medicine have recommended ACS for women with a singleton pregnancy between 34 0/7 and 36 6/7 weeks at imminent risk of preterm birth within 7 days [4,5,6].
Obstetric practices, including those at our own institution, increasingly administered betamethasone for women at risk of late preterm delivery, within and outside of the criteria specified in the ALPS trial [7,8,9]. Though administration of ACS for twins and other deviations have been documented, the benefits remain unclear [9, 10]. Twins and singletons may have biological and pharmacokinetic differences [11], so findings from the ALPS trial may not be generalizable to twin gestations [12, 13]. Neonatal hypoglycemia has also been linked to developmental delays [14, 15], but the relationship is not conclusive [16]. Given that approximately 70% of preterm births occur at 34–36 weeks’ gestation representing 7.5% of all births [17], the implementation of late preterm ACS has potentially far-reaching consequences with uncertain long-term benefits, underscoring the importance of demonstrating real-world effects.
It remains unclear whether the administration of ACS in twin gestations confer the same benefits of reduced respiratory morbidity as well as effects of hypoglycemia as seen in singletons. To date, there is limited evidence documenting the benefits of late preterm steroids in twin gestations [18]. Thus, our study aimed to provide real-world evidence to assess the effect of betamethasone, accounting for dose and timing, in late preterm singleton and twin gestations on neonatal respiratory complications and hypoglycemia.
Materials and Methods
Study population
We used deidentified Electronic Medical Record (EMR) data from the Mount Sinai Health System (MSHS) [19]. Patients with late preterm birth (between 34 0/7 and 36 6/7 weeks of pregnancy) who had never received ACS before 34 weeks of the current pregnancy between 2012 and 2018 were considered eligible for the study. Delivery time and the corresponding gestational age were harmonized using standardized delivery summaries completed by the Labor & Delivery department staff at MSHS. We excluded patients who: i) did not have admission time for delivery or gestational age, ii) were pregnant with triplets or higher multiples, iii) did not have complete demographic information, iv) were newborns with the following (serving as a proxy to potential congenital anomalies): postnatal genetic diagnostic tests, metabolic diagnostic tests, and heart surgeries. The inclusion and exclusion criteria are presented in Fig. 1. The study was approved by the Institutional Review Board at the Icahn School of Medicine at Mount Sinai (IRB-21–00,824). Informed consent from patient is not required as the study uses de-identified data under the HIPAA privacy rule.
Exposure
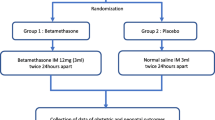
Exposure in the study is defined as receiving at least one dose of ACS between 34 0/0 and 36 6/7 weeks for the first time in the current pregnancy. The protocol for ACS administration at MSHS is a course of two intramuscular injections consisting of 12 mg of betamethasone given 24 h apart. We identified patients who received steroid treatment, as well as the timing and number of doses, using information from RxNorm, a naming system for all medications available in the US market maintained by the US National Library of Medicine (we used the concept unique identifier, RxCUI = 1514, for betamethasone) [20], administration methods, and dosage in the medication records. Receiving at least one dose of ACS was studied to evaluate its overall effectiveness. To assess the dose effect of ACS, we considered whether patients were: i) exposed to the full course of treatment (two doses), ii) exposed only to a partial course (one dose), or iii) never exposed to ACS. We calculated the number of days from receiving the first dose to delivery by coding the value for patients who never received ACS as 0, who received within 24 h prior to delivery as 1, who received 24-48 h prior to delivery as 2 etc., to evaluate the effect of the timing of exposure to ACS.
Outcomes
Our primary outcomes of interest are neonatal respiratory complications and hypoglycemia.
-
i)
Newborns were considered as having respiratory complications if, within 72 h after delivery, they were diagnosed with either respiratory distress syndrome or received treatment for respiratory symptoms, i.e., continuous positive airway pressure, high-flow nasal cannula, and surfactants (Fig. 1a).
-
ii)
Newborns with glucose levels < 40 mg/dL on ≥ 2 occasions within 72 h of birth were considered as having hypoglycemia.
Covariates
Patients’ demographic variables – race and ethnicity, age at delivery, and insurance – were obtained through the EMR. We calculated maternal body mass index (BMI) as weight(kg)/height [2](m [2]) at delivery. Length of pregnancy by week (i.e. gestational age), and mode of delivery were identified using delivery summaries, and ICD9/10 and procedure codes as described in our previous study [21]. Antepartum preeclampsia during pregnancy was determined using electronic phenotyping [22]. Patients receiving medication for gestational diabetes mellitus (insulin, metformin, and glyburide) were included. Birth year (i.e. delivery year), birth weight, sex of newborns, and 5-min Apgar score (using 1-min Apgar score if the 5-min was not available) were also included in the analyses.
Statistical analysis
We used multivariable logistic regression to estimate the association between ACS exposure and respiratory complications and hypoglycemia. In the analysis of respiratory complications and hypoglycemia, we stratified the study population by singleton gestations and twins to minimize the potential confounding from different obstetric management between the two groups. For all the multivariable models, we adjusted for: maternal race/ethnicity, age at delivery, insurance status, BMI at delivery, gestational age at delivery, mode of delivery, antepartum preeclampsia, medication for gestational diabetes, as well as the newborns’ birth year (continuous), birth weight (continuous), sex, and Apgar score (continuous). Statistical analyses were performed using R version 4.0.5 [23].
Results
Characteristics of the study population
Out of 114,312 deliveries identified in MSHS, 4,341 mother–child pairs between 2012 and 2018 were eligible for the study (Fig. 1b). Among the eligible mother–child pairs, there were 3,309 (76.23%) mother–child pairs in singletons and 1,032 (23.77%) mother–child pairs in twins (Fig. 1b). The prevalence of receiving ACS increased over time especially after 2016 (from 2.11% in 2012 to 52.57% in 2018) (Fig. 2a). Of the 745 mother–child pairs who received ACS in the study (631 singletons; 114 twins), only 40.94% completed the full course and 59.06% received one dose within one day of delivery, and none received more than two doses (Fig. 2b, Supplementary Table 1). Characteristics of the study population by betamethasone exposure are summarized in Table 1. Compared to neonates whose mother did not receive ACS, those who had received ACS had a significantly higher percentage of hypoglycemia (20.7% vs. 17.3%, p = 0.03). Proportions of respiratory complications between the two groups were similar. Apart from preeclampsia, maternal BMI at delivery, delivery mode, newborn’s sex, and time from birth to the last record in MSHS, the distributions of most of the covariates were statistically different between the groups with/without receiving antenatal steroid (p < 0.05, Table 1). Descriptive characteristics by outcome status are in Supplementary Tables 2a-b.
Receiving antenatal steroids is associated with reduced odds of neonatal respiratory complications
Multivariable regressions for neonatal respiratory complications are summarized in Fig. 3a-b. We found that any betamethasone use (i.e., at least one dose), had no significant association with respiratory complications in singletons (OR = 0.73, 95% CI:[0.53–1.00], p = 0.06) compared to no betamethasone use, while there was a 64% decrease in odds of respiratory complications in twins (OR = 0.36, 95% CI:[0.16–0.76], p = 0.01).
Association Between Antenatal Corticosteroid (Betamethasone) and Neonatal Respiratory Complications: a shows the results in singletons and b shows the result in twins. Both tables include results of 1) any use of betamethasone, 2) full course (2 doses) of betamethasone vs. no betamethasone, 3) partial course (1 doses) of betamethasone vs. no betamethasone, and 4) days from the first dose of betamethasone to delivery
Additionally, we assessed whether there was an ACS dose effect (i.e., zero vs. one vs. two doses) (Fig. 3a-b). In singletons, those receiving two doses of betamethasone were associated with reduced odds of respiratory complications as compared to those not receiving any, (OR = 0.53, 95% CI:[0.31–0.85], p = 0.01); however, those receiving one dose did not show a significant difference in respiratory complications (OR = 0.88, 95% CI:[0.60–1.28], p = 0.51). Compared to twins not exposed to any ACS, there was no significant difference in respiratory complications in twins receiving two doses of betamethasone (OR = 0.42, 95% CI:[0.11–1.23], p = 0.16); however, receiving one dose was associated with reduced odds of respiratory complications (OR = 0.34, 95% CI:[0.12–0.82], p = 0.02).
We also assessed the association of the timing of ACS administration and respiratory complications. Newborns had lower odds of developing respiratory complications if their mothers received betamethasone earlier in both singletons (OR = 0.87, 95% CI:[0.79–0.96], p = 0.01) and twins (OR = 0.70, 95% CI:[0.47–0.95], p = 0.05) (Fig. 3a-b). The full regression model outputs are in Supplementary Figs. 1–2.
Receiving antenatal steroids is associated with increased odds of neonatal hypoglycemia
In singletons, across all dosing groups betamethasone exposure was associated with increased odds of developing hypoglycemia within 72 h of birth (OR = 1.41, 95% CI:[1.09–1.82], p = 0.01, Fig. 4a). Relative to the group not receiving betamethasone, there was no significant association between hypoglycemia and receiving one dose of betamethasone (OR = 1.10, 95% CI:[0.79–1.51], p = 0.58) (Fig. 4a), although receiving two doses was associated with increased odds (OR = 1.86, 95% CI:[1.34–2.56], p < 0.01) of hypoglycemia.
Association Between Antenatal Corticosteroid (Betamethasone) and Neonatal Hypoglycemia: a shows the results in singletons and b shows the result in twins. Both tables include results of 1) any use of betamethasone, 2) full course (2 doses) of betamethasone vs. no betamethasone, 3) partial course (1 doses) of betamethasone vs. no betamethasone, and 4) days from the first dose of betamethasone to delivery
In twins, being exposed to at least one dose of betamethasone was not significantly associated with hypoglycemia (OR = 1.25, 95% CI:[0.72–2.09], p = 0.41, Fig. 4b). However, receiving two doses was associated with increased odds of having hypoglycemia compared to no betamethasone (OR = 2.18, 95% CI:[1.12–4.10], p = 0.02, Fig. 4b). The association was not statistically significant in twins receiving one dose of betamethasone relative to no doses (OR = 0.62, 95% CI:[0.25–1.34], p = 0.25).
In addition, longer intervals between the first betamethasone administration and delivery were associated with increased odds of hypoglycemia in singletons (OR = 1.06, 95% CI:[1.00–1.12], p = 0.05), but the association in twins was not statistically significant (OR = 0.97, 95% CI:[0.82–1.10], p = 0.72, Fig. 4a-b).
Discussion
Principal Findings
In this late preterm cohort, the use of ACS has been increasing since 2016, in response to ACOG guidelines (Fig. 2a). Patients receiving a full course of ACS i) were less likely to have neonatal respiratory complications but more likely to have hypoglycemia among singletons; ii) had increased odds of hypoglycemia but no significant association with respiratory complications among twins. Although a partial course was associated with reduced respiratory complications among twins, the association with other outcomes was not conclusive.
Results in the Context of What is Known
Among singletons receiving a full course of ACS, our result of decreased respiratory complications is consistent with the ALPS trial, as well as retrospective observational studies [3, 24, 25]. Still, others have found no reduction [26,27,28,29]. It has been suggested that the distribution of pregnancies by gestational age could explain the different findings between studies as ACS may be more effective in reducing respiratory morbidity due to lung immaturity at earlier gestational ages within the late preterm period [25]. Our study includes a gestational age distribution similar to previous studies with adequate representation of both earlier and later gestational ages between 34 and 36 weeks [25, 30, 31]. In terms of hypoglycemia, our findings were largely consistent with what has been found [28, 30,31,32]. Our definition of hypoglycemia was compatible with the ALPS trial. However, different cutoffs in blood glucose levels (e.g. 50 mg/dl [28]) and time after delivery (e.g. within 48 hr [32].) have been reported, making direct comparisons difficult. For twin gestations that received the full course of ACS, our finding is consistent with a study in Israel [12]. However, the gestational age at administration might be more important than ACS exposure in twins [12, 13, 33].
We examined partial dosing and days of ACS administration from delivery. Results indicate that exposure to partial dosing of betamethasone among singletons was not associated with reduced odds of respiratory complications, in contrast to those receiving the full course. Among twins, we found the opposite; the reason for this is unclear but there are potential physiologic and metabolic differences between twin and singleton gestations [11]. Receiving only a partial course of betamethasone compared to none did not increase the odds of hypoglycemia among either singletons or twins, suggestive of a potential dose–effect. While Janssen et al. evaluated number of doses and saw no significant associations with respiratory complications, the variable entered in their model was continuous, making a direct comparison difficult. [25]
Regarding ACS-to-delivery interval, few have examined this; we showed that longer intervals were associated with decreased odds of respiratory complications in both singleton and twin gestations. A retrospective cohort study in Korea in early preterm twins reported that an interval of 2–7 days was associated with decreased odds of respiratory distress syndrome, but not with an interval of fewer than 2 days, when compared to those unexposed to ACS [34]. However, in Janssen et al., reduced odds of respiratory complications was only shown when ACS was administered within 2 days, but not within 7 days of delivery among late preterm newborns. [25] A recent study in the US has shown that newborns who have been exposed to ACS were more likely to have severe hypoglycemia within a one-day interval when compared to unexposed newborns [35].
Strengths and Limitations
The major strength of this study is that it includes a large study cohort with diversity in provider types allowing for the opportunity to evaluate the implementation of ACOG guidelines outside research settings. With “any betamethasone use” as an exposure, we provide an estimation of the overall effectiveness of the new ACOG guidelines in MSHS. We also examined the effects of deviations from what has been studied in the ALPS trial including twin gestations and partial dosing of ACS, which is commonly seen in clinical settings, yet lacks definitive clinical evidence. As we await an ongoing trial evaluating ACS in late preterm twin gestations [18], our study adds to the nascent evidence base for this group. Our study also included patients taking gestational diabetes medication, unlike others [26,27,28]. Until more definitive evidence is available for groups not studied in the ALPS trial, this study supports shared decision-making between patient and provider in discussing potential benefits and unknown long-term outcomes.
We acknowledge several limitations of our study. It is retrospective and subject to inherent ascertainment bias and unmeasured confounding. Additionally, we did not account for glucose levels after 72 h of birth and postnatal management in the study; therefore, we could not distinguish between transient and persistent hypoglycemia. Future research should address this limitation as only ~ 2% in the ALPS cohort had persistent hypoglycemia [36]. We may not have a large enough sample to detect significant associations among the twins exposed to full course of ACS. The structured EMR data used in this study lacked granularity to assess for provider practice differences, length of respiratory support, and adverse events related to hypoglycemia. We also acknowledge that since ICD codes are primarily used for billing purposes, we may not have captured the full relevant cohort of newborns.
Conclusions
ACS administration adherent to ACOG guidelines reflected the findings of the ALPS trial, and was similar for twin gestations. We believe that the study findings based on real-world implementation of clinical guidelines are critical to informing the effect of ACS outside research settings, and health systems should systematically monitor how guidelines are implemented to improve the health of patients.
Availability of data and materials
The clinical data here were used under license from Mount Sinai Data Warehouse in the current study. As a result, this dataset is not publicly available. Qualified researchers affiliated with the Mount Sinai Health Systems may apply for access to these data through the Mount Sinai Health Systems Institutional Review Board. We used R version 4.0.5 to analyze our data, and will release the code under the CC BY-NC-SA 3.0 license (https://creativecommons.org/licenses/by-nc-sa/3.0/).
Abbreviations
- ACOG:
-
American College of Obstetricians and Gynecologists
- ACS:
-
Antenatal corticosteroid
- ALPS:
-
Antenatal Late Preterm Steroids
- BMI:
-
Body mass index
- EMR:
-
Electronic medical record
- MSHS:
-
Mount Sinai Health System
- NICU:
-
Neonatal intensive care unit
References
Gilstrap LC, Christensen R, Clewell WH, et al. Effect of Corticosteroids for Fetal Maturation on Perinatal Outcomes NIH Consensus Development Panel on the Effect of Corticosteroids for Fetal Maturation on Perinatal Outcomes. JAMA. 1995;273(5):413–8. https://doi.org/10.1001/jama.1995.03520290065031.
McGoldrick E, Stewart F, Parker R, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2020;2021(2). https://doi.org/10.1002/14651858.CD004454.pub4
Gyamfi-Bannerman C, Thom EA, Blackwell SC, et al. Antenatal Betamethasone for Women at Risk for Late Preterm Delivery. N Engl J Med. 2016;374(14):1311–20. https://doi.org/10.1056/nejmoa1516783.
4.Committee Opinion No. 713: Antenatal Corticosteroid Therapy for Fetal Maturation. Obstet Gynecol. 2017;130(2):e102-e109.https://doi.org/10.1097/AOG.0000000000002237
Implementation of the use of antenatal corticosteroids in the late preterm birth period in women at risk for preterm delivery. Am J Obstet Gynecol. 2016;215(2):B13-B15. https://doi.org/10.1016/j.ajog.2016.03.013
Reddy UM, Deshmukh U, Dude A, Harper L, Osmundson SS. Society for Maternal-Fetal Medicine Consult Series #58: Use of antenatal corticosteroids for individuals at risk for late preterm delivery. Am J Obstet Gynecol. 2021. https://doi.org/10.1016/j.ajog.2021.07.023 (Published online).
Freret TS, James KE, Melamed A, Gyamfi-Bannerman C, Kaimal AJ, Clapp MA. Late-preterm steroid use among individuals with pregestational diabetes mellitus and with twin gestations. Published onlinehttps://doi.org/10.1016/j.ajog
Kearsey EOR, Been JV, Souter VL, Stock SJ. The impact of the Antenatal Late Preterm Steroids trial on the administration of antenatal corticosteroids. Am J Obstet Gynecol. 2022;227(2):280.e1-280.e15. https://doi.org/10.1016/j.ajog.2022.03.037.
McElwee ER, Wilkinson K, Crowe R, et al. Indication Creep of Antenatal Late Preterm Steroids. Am J Perinatol. 2022;39(11):1159–65. https://doi.org/10.1055/a-1785-9290.
Kamath-Rayne BD, Rozance PJ, Goldenberg RL, Jobe AH. Antenatal corticosteroids beyond 34 weeks gestation: What do we do now? Am J Obstet Gynecol. 2016;215(4):423–30. https://doi.org/10.1016/j.ajog.2016.06.023.
Ballabh P, Lo ES, Kumari J, et al. Pharmacokinetics of betamethasone in twin and singleton pregnancy. Clin Pharmacol Ther. 2002;71(1):39–45. https://doi.org/10.1067/mcp.2002.120250.
Ben-David A, Zlatkin R, Bookstein-Peretz S, Meyer R, Mazaki-Tovi S, Yinon Y. Does antenatal steroids treatment in twin pregnancies prior to late preterm birth reduce neonatal morbidity? Evidence from a retrospective cohort study. Arch Gynecol Obstet. 2020;302(5):1121–6. https://doi.org/10.1007/s00404-020-05709-w.
Martinka D, Barrett J, Mei-dan E, Zaltz A, Melamed N. Respiratory morbidity in late preterm twin infants. Arch Gynecol Obstet. 2019;300(2):337–45. https://doi.org/10.1007/s00404-019-05191-z.
Kerstjens JM, Bocca-Tjeertes IF, de Winter AF, Reijneveld SA, Bos AF. Neonatal morbidities and developmental delay in moderately preterm-born children. Pediatrics. 2012;130(2). https://doi.org/10.1542/peds.2012-0079
Wickström R, Skiöld B, Petersson G, Stephansson O, Altman M. Moderate neonatal hypoglycemia and adverse neurological development at 2–6 years of age. Eur J Epidemiol. 2018;33(10):1011–20. https://doi.org/10.1007/s10654-018-0425-5.
Goode RH, Rettiganti M, Li J, et al. Developmental outcomes of preterm infants with neonatal hypoglycemia. Pediatrics. 2016;138(6). https://doi.org/10.1542/peds.2016-1424
Martin JA, Hamilton BE, Osterman MJK, Driscoll AK. National Vital Statistics Reports Volume 70, Number 2, March 23 Births: Final Data for 2019; 2019. https://www.cdc.gov/nchs/products/index.htm. Accessed 30 Nov 2021.
Hong S, Lee SM, Kwak DW, et al. Effects of antenatal corticosteroids in twin neonates with late preterm birth (ACTWIN [Antenatal Corticosteroids in TWIN late preterm neonates] trial): Study protocol for a randomized controlled trial. BMC Pregnancy Childbirth. 2019;19(1). https://doi.org/10.1186/s12884-019-2235-5
Icahn School of Medicine at Mount Sinai. Mount Sinai Data Warehouse. https://labs.icahn.mssm.edu/msdw/. Accessed 30 Nov 2021.
Nelson SJ, Zeng K, Kilbourne J, Powell T, Moore R. Normalized names for clinical drugs: RxNorm at 6 years. J Am Med Inform Assoc. 2011;18(4):441–8. https://doi.org/10.1136/amiajnl-2011-000116.
Zheutlin AB, Vieira L, Shewcraft RA, et al. Improving postpartum hemorrhage risk prediction using longitudinal electronic medical records. J Am Med Inform Assoc. Published online August 18, 2021. https://doi.org/10.1093/jamia/ocab161
Li S, Wang Z, Vieira LA, et al. Improving Pre-eclampsia Risk Prediction by Modeling Individualized Pregnancy Trajectories Derived from Routinely Collected Electronic Medical Record Data. https://doi.org/10.1101/2021.03.23.21254178
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/. Accessed 30 Nov 2021.
Üstün N, Hocaoğlu M, Turgut A, Arslanoğlu S, Ovalı F. Does antenatal corticosteroid therapy improve neonatal outcomes in late preterm birth? J Matern-Fetal Neonatal Med. 2020. https://doi.org/10.1080/14767058.2020.1808614 (Published online).
Janssen O, Ratner V, Lin J, Fox N, Green R. Respiratory and glycemic control outcomes of late preterm infants after antenatal corticosteroid exposure. J Perinatol. 2021. https://doi.org/10.1038/s41372-021-01162-y (Published online).
Ontela V, Dorairajan G, Bhat VB, Chinnakali P. Effect of antenatal steroids on respiratory morbidity of late preterm newborns: A randomized controlled trial. J Trop Pediatr. 2018;64(6):531–8. https://doi.org/10.1093/tropej/fmy001.
Porto AMF, Coutinho IC, Correia JB, Amorim MMR. Effectiveness of antenatal corticosteroids in reducing respiratory disorders in late preterm infants: Randomised clinical trial. BMJ. 2011;342(7802). https://doi.org/10.1136/bmj.d1696
Badreldin N, Willert GG, Henricks AA, Peaceman A, Caldarelli LA, Yee LM. Implementation of an antenatal late-preterm corticosteroid protocol at a high-volume tertiary care center. Am J Obstet Gynecol MFM. 2020;2(1):100076. https://doi.org/10.1016/j.ajogmf.2019.100076.
Kamath-Rayne BD, Defranco EA, Marcotte MP. Antenatal steroids for treatment of fetal lung immaturity after 34 weeks of gestation: An evaluation of neonatal outcomes. Obstet Gynecol. 2012;119(5):909–16. https://doi.org/10.1097/AOG.0b013e31824ea4b2.
Uquillas KR, Lee RH, Sardesai S, et al. Neonatal hypoglycemia after initiation of late preterm antenatal corticosteroids. J Perinatol. 2020;40(9):1339–48. https://doi.org/10.1038/s41372-020-0589-1.
Alrais MA, Chen HY, Sibai BM, Blackwell SC. Frequency of Neonatal Hypoglycemia After Implementation of Antenatal Late Preterm Steroids Use [19K]. Obstet Gynecol. 2018;131(1):124S-124S. https://doi.org/10.1097/01.AOG.0000533521.16220.7d.
di Pasquo E, Saccone G, Angeli L, et al. Determinants of neonatal hypoglycemia after antenatal administration of corticosteroids (ACS) for lung maturation: Data from two referral centers and review of the literature. Early Hum Dev. 2020;143. https://doi.org/10.1016/j.earlhumdev.2020.104984
Salem SY, Kibel M, Asztalos E, Zaltz A, Barrett J, Melamed N. Neonatal Outcomes of Low-Risk, Late-Preterm Twins Compared with Late-Preterm Singletons. Obstet Gynecol. 2017;130(3):582–90. https://doi.org/10.1097/AOG.0000000000002187.
Kuk JY, An JJ, Cha HH, et al. Optimal time interval between a single course of antenatal corticosteroids and delivery for reduction of respiratory distress syndrome in preterm twins. Am J Obstet Gynecol. 2013;209(3):256.e1-7. https://doi.org/10.1016/j.ajog.2013.06.020.
McElwee ER, Wilkinson K, Crowe R, et al. Latency of late preterm steroid administration to delivery and risk of neonatal hypoglycemia. Am J Obstet Gynecol MFM. 2022;4(5). https://doi.org/10.1016/j.ajogmf.2022.100687
Gyamfi-Bannerman C, Jablonski KA, Blackwell SC, et al. Evaluation of Hypoglycemia in Neonates of Women at Risk for Late Preterm Delivery: An Antenatal Late Preterm Steroids Trial Cohort Study. Am J Perinatol. 2021. https://doi.org/10.1055/s-0041-1729561 (Published online).
Aris IM, Kleinman KP, Belfort MB, Kaimal A, Oken E. A 2017 US reference for singleton birth weight percentiles using obstetric estimates of gestation. Pediatrics. 2019;144(1). https://doi.org/10.1542/peds.2019-0076
Acknowledgements
We thank Mount Sinai Data Warehouse for providing data from Mount Sinai Health System’s electronic medical record system. We also thank the Sema4 IT team for infrastructural and computational support.
Funding
This project was performed in collaboration with Sema4. Sema4 is a company that integrates genetic testing and data analytics to improve diagnosis, treatment, and prevention of disease. The Icahn School of Medicine at Mount Sinai holds equity in this for-profit company.
Author information
Authors and Affiliations
Contributions
LL and LV were involved in concept and design. YK was involved in data acquisition. YK, ZW, SL, and AZ were involved in data cleaning. YK, LV, DT, YL, SG, JS, SD, and ES were involved in interpretation of data. YK was involved in data analysis. YK, LV, YL, and LL were involved in drafting of the manuscript. All authors were involved in critical revision of the manuscript for important intellectual content. LL and ES were involved in supervision. All authors take responsibility for the final, published version and are accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All research was conducted in accordance with the relevant ethical guidelines and regulations at the Icahn School of Medicine at Mount Sinai. The study was approved by the Institutional Review Board at the Icahn School of Medicine at Mount Sinai (IRB-21–00824). Informed consent from patient is not required as the study uses de-identified data under the HIPAA privacy rule.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This study was conducted in New York City, NY, and Stamford, CT.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Vieira, L.A., Kao, YH., Tsevdos, D.S. et al. Late preterm antenatal corticosteroids in singleton and twin gestations: a retrospective cohort study. BMC Pregnancy Childbirth 22, 904 (2022). https://doi.org/10.1186/s12884-022-05262-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-022-05262-1