Abstract
Objective
The purpose of our study was to explore maternal and fetal outcomes in the second and third trimester in women with uterine malformations.
Study design
This was a retrospective population-based cohort study including women with a diagnosis of uterine malformation arised from workup for infertility or recurrent pregnancy loss, was accidental during pregnancy, or was noticed at the time of cesarean delivery.
Results
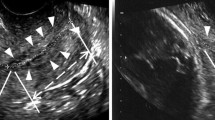
A total of 280,721 pregnancies met the inclusion criteria and were divided into two study groups: (1) pregnancies in women with uterine malformations (n = 1099); and (2) controls (n = 279,662). The rate of women presenting uterine malformations was 0.39%. The prevalence of cervical os insufficiency was significantly higher in women with a uterine malformation than in the control group (3.6 vs. 0.4%, p < 0.001). A multivariate analysis, performed to evaluate risk factors for cervical insufficiency in women with uterine malformations. Mullerian anomalies (OR 6.19, 95% CI 4.41–8.70, p < 0.001), maternal age (OR 1.05, 95% CI 1.04–1.06, p < 0.001), recurrent abortions (OR 12.93, 95% CI 11.43–14.62, p < 0.001), and ethnicity (OR 2.86, 95% CI 2.454–3.34, p < 0.001) were found to be independently associated with the development of cervical insufficiency.
Conclusion
Uterine anomalies have a strong association with cervical insufficiency. Women with uterine anomalies have an increased risk to develop pregnancy complications that arise from a loss in cervical function during the midtrimester or early third trimester.

Reproduced with permission from [24]
Similar content being viewed by others
References
Iams JD, Johnson FF, Sonek J et al (1995) Cervical competence as a continuum: a study of ultrasonographic cervical length and obstetric performance. Am J Obstet Gynecol 172(4 Pt 1):1097–1103 Discussion 1104–1096
Rafaeli-Yehudai T, Kessous R, Aricha-Tamir B et al (2014) The effect of cervical cerclage on pregnancy outcomes in women following conization. J Matern Fetal Neonatal Med 27(15):1594–1597
Romero R, Espinoza J, Kusanovic JP et al (2006) The preterm parturition syndrome. BJOG 113(Suppl 3):17–42
Reichman D, Laufer MR, Robinson BK (2009) Pregnancy outcomes in unicornuate uteri: a review. Fertil Steril 91(5):1886–1894
Mastrolia SA, Baumfeld Y, Hershkovitz R, et al. (2016) Bicornuate uterus is an independent risk factor for cervical os insufficiency: a retrospective population based cohort study. J Matern Fetal Neonatal Med 30(22):2705–2710
Raga F, Bauset C, Remohi J et al (1997) Reproductive impact of congenital Müllerian anomalies. Hum Reprod 12(10):2277–2281
Sadek SM, Ahmad RA, Soliman BS (2015) Three dimensional color Doppler transvaginal ultrasound morphologic features of uterine septum and residual cavity in women with reproductive failure. Middle East Fertility Soc J 20:21–26
Rock JA, Schlaff WD (1985) The obstetric consequences of uterovaginal anomalies. Fertil Steril 43(5):681–692
Stray-Pedersen B, Stray-Pedersen S (1984) Etiologic factors and subsequent reproductive performance in 195 couples with a prior history of habitual abortion. Am J Obstet Gynecol 148(2):140–146
Sanfilippo JS, Wakim NG, Schikler KN, Yussman MA (1986) Endometriosis in association with uterine anomaly. Am J Obstet Gynecol 154(1):39–43
Green LK, Harris RE (1976) Uterine anomalies. Frequency of diagnosis and associated obstetric complications. Obstet Gynecol 47(4):427–429
Acién P (1993) Reproductive performance of women with uterine malformations. Hum Reprod 8(1):122–126
Acién P (1997) Incidence of Müllerian defects in fertile and infertile women. Hum Reprod 12(7):1372–1376
Strassmann EO (1966) Fertility and unification of double uterus. Fertil Steril 17(2):165–176
Lin PC, Bhatnagar KP, Nettleton GS, Nakajima ST (2002) Female genital anomalies affecting reproduction. Fertil Steril 78(5):899–915
Lin PC (2004) Reproductive outcomes in women with uterine anomalies. J Womens Health (Larchmt) 13(1):33–39
Propst AM, Hill JA (2000) Anatomic factors associated with recurrent pregnancy loss. Semin Reprod Med 18(4):341–350
Jurkovic D, Geipel A, Gruboeck K et al (1995) Three-dimensional ultrasound for the assessment of uterine anatomy and detection of congenital anomalies: a comparison with hysterosalpingography and two-dimensional sonography. Ultrasound Obstet Gynecol 5(4):233–237
Saravelos SH, Cocksedge KA, Li TC (2008) Prevalence and diagnosis of congenital uterine anomalies in women with reproductive failure: a critical appraisal. Hum Reprod Update 14(5):415–429
Statistics TCBo. Israel in Figures 2013. http://www.cbs.gov.il/www/publications/isr_in_n13e.pdf. Accessed 25 May 2015
ACOG practice bulletin (2002) Diagnosis and management of preeclampsia and eclampsia. Number 33, January 2002. Obstet Gynecol 99(1):159–167
White P (1949) Pregnancy complicating diabetes. Am J Med 7(5):609–616
Leiberman JR, Fraser D, Weitzman S, Glezerman M (1993) Birthweight curves in southern Israel populations. Isr J Med Sci 29(4):198–203
The American Fertility Society (1988) The American Fertility Society classifications of adnexal adhesions, distal tubal occlusion, tubal occlusion secondary to tubal ligation, tubal pregnancies, müllerian anomalies and intrauterine adhesions. Fertil Steril 49(6):944–955
Gynecologists ACoOa (2009) ACOG Practice Bulletin No. 106: Intrapartum fetal heart rate monitoring: nomenclature, interpretation, and general management principles. Obstet Gynecol 14(1):192–202
The American College of Obstetricians and Gynecologists. Task Force on Neonatal Encephalopathy and Cerebral Palsy, the American Academy of Pediatrics. Neonatal encephalopathy and cerebral palsy: defining the pathogenesis and physiopathology. Washington (DC): American College of Obstetricians and Gynecologists; 2003: 1–85
Romero R, Gonzalez R, Sepulveda W et al (1992) Infection and labor. VIII. Microbial invasion of the amniotic cavity in patients with suspected cervical incompetence: prevalence and clinical significance. Am J Obstet Gynecol 167(4 Pt 1):1086–1091
Leible S, Muñoz H, Walton R et al (1998) Uterine artery blood flow velocity waveforms in pregnant women with müllerian duct anomaly: a biologic model for uteroplacental insufficiency. Am J Obstet Gynecol 178(5):1048–1053
Akar ME, Bayar D, Yildiz S, Ozel M, Yilmaz Z (2005) Reproductive outcome of women with unicornuate uterus. Aust N Z J Obstet Gynaecol 45(2):148–150
Golan A, Langer R, Wexler S et al (1990) Cervical cerclage–its role in the pregnant anomalous uterus. Int J Fertil 35(3):164–170
Żyła MM, Wilczyński J, Nowakowska-Głąb A, Maniecka-Bryła I, Nowakowska D (2015) Pregnancy and delivery in women with uterine malformations. Adv Clin Exp Med 24(5):873–879
Tulandi T, Arronet GH, McInnes RA (1980) Arcuate and bicornuate uterine anomalies and infertility. Fertil Steril 34(4):362–364
Rackow BW, Arici A (2007) Reproductive performance of women with müllerian anomalies. Curr Opin Obstet Gynecol 19(3):229–237
Tomazevic T, Ban-Frangez H, Ribic-Pucelj M, Premru-Srsen T, Verdenik I (2007) Small uterine septum is an important risk variable for preterm birth. Eur J Obstet Gynecol Reprod Biol 135(2):154–157
Chan YY, Jayaprakasan K, Tan A et al (2011) Reproductive outcomes in women with congenital uterine anomalies: a systematic review. Ultrasound Obstet Gynecol 38(4):371–382
Hua M, Odibo AO, Longman RE et al (2011) Congenital uterine anomalies and adverse pregnancy outcomes. Am J Obstet Gynecol 205(6):558.e1–558.e5
Stein AL, March CM (1990) Pregnancy outcome in women with müllerian duct anomalies. J Reprod Med 35(4):411–414
Craig CJ (1973) Congenital abnormalities of the uterus and foetal wastage. S Afr Med J 47(42):2000–2005
Zupi E, Solima E, Marconi D, Valli E, Romanini C (1996) Uterine anomalies prevalence and reproductive outcome in women undergoing diagnostic hysteroscopy. Gynaecol Endosc 5:147–150
Zlopasa G, Skrablin S, Kalafatić D, Banović V, Lesin J (2007) Uterine anomalies and pregnancy outcome following resectoscope metroplasty. Int J Gynaecol Obstet 98(2):129–133
Zhang Y, Zhao YY, Qiao J (2010) Obstetric outcome of women with uterine anomalies in China. Chin Med J (Engl) 123(4):418–422
Shuiqing M, Xuming B, Jinghe L (2002) Pregnancy and its outcome in women with malformed uterus. Chin Med Sci J 17(4):242–245
Fox NS, Roman AS, Stern EM et al (2014) Type of congenital uterine anomaly and adverse pregnancy outcomes. J Matern Fetal Neonatal Med 27(9):949–953
Jayaprakasan K, Chan YY, Sur S et al (2011) Prevalence of uterine anomalies and their impact on early pregnancy in women conceiving after assisted reproduction treatment. Ultrasound Obstet Gynecol 37(6):727–732
Maneschi F, Zupi E, Marconi D et al (1995) Hysteroscopically detected asymptomatic müllerian anomalies. Prevalence and reproductive implications. J Reprod Med 40(10):684–688
Sørensen SS, Trauelsen AG (1987) Obstetric implications of minor müllerian anomalies in oligomenorrheic women. Am J Obstet Gynecol 156(5):1112–1118
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflict of interest to declare.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Mastrolia, S.A., Baumfeld, Y., Hershkovitz, R. et al. Independent association between uterine malformations and cervical insufficiency: a retrospective population-based cohort study. Arch Gynecol Obstet 297, 919–926 (2018). https://doi.org/10.1007/s00404-018-4663-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-018-4663-2