Abstract
Purpose
Trans-vaginal sacrospinous colpopexy is one of the surgical procedures used to repair varying degrees of vaginal vault and uterovaginal prolapse. The purpose of this study is to analyse the potential risk factors of surgical failure following sacrospinous colpopexy.
Methods
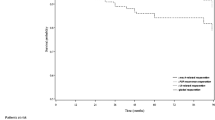
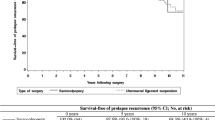
A retrospective study of 114 women who underwent unilateral sacrospinous colpopexy at Jordan University Hospital from January 2005 to January 2008 were included. Patient demographics, clinical characteristics and concomitant pelvic organ prolapse surgery were assessed. The patients were evaluated at 6 weeks, and every 6 months thereafter. Twelve (11 %) had recurrent apical (vaginal cuff) prolapse, 26 (23 %) had recurrent prolapse at any compartment were compared with those who had successful surgery. Univariate and logistic regression analyses were used to assess the independent prognostic values of the variables associated with surgical failure.
Results
After a mean follow-up of 40 months, the statistically significant predictors of surgical failure included the presence of advanced pre-operative stages of prolapse (stages III and IV), the more distally located points Ba, Bp and C and a lack of mesh augmentation of the anterior vaginal wall during surgery (P = 0.01, 0.027, 0.024, 0.034 and 0.006, respectively). However, a history of prior vaginal repair, the more distally located point Ba and a lack of anterior vaginal wall mesh augmentation were defined as independent predictive variables based on logistic regression analyses (P = 0.04, 0.005 and 0.046, respectively).
Conclusions
The presence of advanced anterior vaginal wall prolapse, prior vaginal repair and a lack of mesh augmentation of the anterior compartment are significant risk factors for the surgical failure of sacrospinous suspension surgery.


Similar content being viewed by others
References
Samuelsson EC, Victor FT, Tibblin G, Svardsudd KF (1999) Signs of genital prolapse in a Swedish population of women 20 to 59 years of age and possible related factors. Am J Obstet Gynecol 180:299–305
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
Randall CL, Nichols DH (1971) Surgical treatment of vaginal eversion. Obstet Gynecol 38:327–332
Sze EHM, Karram MM (1997) Transvaginal repair of vault prolapse: a review. Obstet Gynecol 89:466–475
Nichols DH (1982) Sacrospinous fixation for massive eversion of the vagina. Am J Obstet Gynecol 142:901–904
Morley GW, De Lancey JO (1988) Sacrospinous ligament fixation for eversion of the vagina. Am J Obstet Gynecol 158:872–879
Richter K, Albrich W (1981) Long term results following fixation of the vagina on the sacrospinal ligament by the vaginal route (vaginaefixatio sacrospinalis vaginalis). Am J Obstet Gynecol 141:811–816
Bump RC, Mattiasson A, Bø K et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
de Tayrac R, Gervaise A, Chauveaud A, Fernandez H (2005) Tension-free polypropylene mesh for vaginal repair of anterior vaginal wall prolapse. J Reprod Med 50(2):75–80
Miyazaki FS (1987) Miya Hook ligature carrier for sacrospinous ligament suspension. Obstet Gynecol 70:286–288
Maher CF, Qatawneh AM, Baessler K, Schluter PJ (2004) Midline rectovaginal fascial plication for repair of rectocele and obstructed defecation. Obstet Gynecol 104:685–689
Paraiso MF, Ballard LA, Walters MD, Lee JC, Mitchinson AR (1996) Pelvic support defects defects and visceral and sexual function in women treated with sacrospinous ligament suspension and pelvic reconstruction. Am J Obstet Gynecol 175:1423–1430
Maher CF, Murray CJ, Carey MP, Dwyer PL, Ugoni AM (2001) Iliococcygeus or sacrospinous fixation for vaginal vault prolapse. Am J Obstet Gynecol 98:40–44
Hoffman MS, Harris MS, Bouis PJ (1996) Sacrospinous colpopexy in the management of uterovaginal prolapse. J Reprod Med 41:299–303
Holley RL, Varner RE, Gleason BP, Apffel LA, Scott S (1995) Recurrent pelvic support defects after sacrospinous ligament fixation for vaginal vault prolapse. J Am Coll Surg 180:444–448
Heinonen PK (1992) Transvaginal sacrospinous colpopexy for vaginal vault and complete genital prolapse in aged women. Acta Obstet Gynecol Scand 71:377–381
Nieminen K, Huhtala H, Heinonen P (2003) Anatomic and functional assessment and risk factors of recurrent prolapse after vaginal sacrospinous fixation. Acta Obstet Gynecol Scand 82:471–478
Whiteside J, Weber A, Meyn LA, Walters MD (2004) Risk factors for prolapse recurrence after vaginal repair. Am J Obstet Gynecol 191:1533–1538
Diez-Itza I, Azipitarte I, Beccerro A (2007) Risk factors for the recurrence of pelvic organ prolapse after vaginal surgery: a review at 5 years after surgery. Int Urogynecol J Pelvic Floor Dysfunct 18:1317–1324
Lin TY, Su TH, Wang YL, Lee MY, Hsieh CH, Wang KG, Chen GD (2005) Risk factors for failure of transvaginal sacrospinous uterine suspension in the treatment of uterovaginal prolapse. J Formos Med Assoc 104(4):249–253
Chen H-Y, Chiu T-H, Ho M, Hung Y-C (2009) Analysis of risk factors associated with surgical failure of sacrospinous suspension for uterine or vaginal vault prolapse. Int Urogynecol J Pelvic Floor Dysfunct 20:387–391
Benson JT, Lucente V, McClellan E (1996) Vaginal versus abdominal reconstructive surgery for the treatment of pelvic support defects: a prospective randomized study with long-term outcome evaluation. Am J Obstet Gynecol 175:1418–1421
Maher CF, Qatawneh A, Dwyer PL, Carey MP, Cornish A, Schluter P (2004) Abdominal sacral colpopexy for vaginal vault prolapse. A prospective randomized trial. Am J Obstet Gynecol 190:20–26
Maher C, Baessler K, Glazener MC, Adams EJ, Hagen S (2007) Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 18:CD004014
Tsia-Shu L, Kiran A (2011) Combined anterior trans-obturator mesh and sacrospinous ligament fixation in women with severe prolapse—a case series of 30 months follow-up. Int Urogynecol J Pelvic Floor Dysfunct 22:299–306
Clark A, Gregory T, Smith V, Edwards R (2003) Epidemiologic evaluation of reoperation for surgically treated pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol 189:1261–1267
Acknowledgments
The authors would like to thank Jordan University Hospital for supporting this research.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Qatawneh, A., Thekrallah, F., Bata, M. et al. Risk factors of surgical failure following sacrospinous colpopexy for the treatment of uterovaginal prolapse. Arch Gynecol Obstet 287, 1159–1165 (2013). https://doi.org/10.1007/s00404-012-2685-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-012-2685-8