Abstract
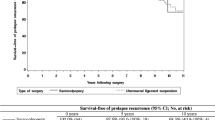
The goal of this study was to analyze the potential risk factors determining surgical failure after sacrospinous suspension for uterine or vaginal vault prolapse. Each woman underwent a detailed history taking and a vaginal examination before treatment. Follow-up evaluations were at immediate post-operation, 1 week, 1 to 3 months, 6 months, 9 months, and annually after the operation. The surgical failure rate (27/168) following sacrospinous suspension was 16.1%. Using multivariable logistic regression, women with the presence of C or D point stage I at immediate post-operation were a significant risk factor for surgical failure after sacrospinous suspension (odds ratio, 35.34; 95% confidence interval, 8.75–162.75; p < 0.001). The success rate during the 18-month follow-up decreased significantly in women with the presence of C or D point stage I at immediate post-operation than stage 0. Although the sample size of women with symptomatic uterine or vaginal vault prolapse is small, impaired correction of anatomic defects is a significant risk factor for surgical failure of sacrospinous suspension.

Similar content being viewed by others
Abbreviations
- POP:
-
pelvic organ prolapse
- ICS:
-
International Continence Society
References
Koduri S, Sand PK (2000) Recent developments in pelvic organ prolapse. Curr Opin Obstet Gynecol 12:399–404
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
Clark AL, Gregory T, Smith VJ, Edwards R (2003) Epidemiologic evaluation of reoperation for surgically treated pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol 189:1261–1267
Richardson AC, Lyon JB, Williams NL (1976) A new look at pelvic relaxation. Am J Obstet Gynecol 126:568–573
Richter K, Albrich W (1981) Long-term results following fixation of the vagina on the sacrospinal ligament by the vaginal route (vaginaefixatio sacrospinalis vaginalis). Am J Obstet Gynecol 141:811–816
Maher CF, Carey MP, Slack MC, Murray CJ, Milligan M, Schluter P (2001) Uterine preservation or hysterectomy at sacrospinous colpopexy for uterovaginal prolapse? Int Urogynecol J Pelvic Floor Dysfunct 12:381–385
Nichols DH (1982) Sacrospinous fixation for massive eversion of the vagina. Am J Obstet Gynecol 142:901–904
Morely GN, DeLancey JO (1988) Sacrospinous ligament fixation for eversion of the vagina. Am J Obstet Gynecol 158:872–879
Cruikshank SH, Cox DW (1990) Sacrospinous ligament fixation at the time of transvaginal hysterectomy. Am J Obstet Gynecol 162:1611–1619
Backer MH (1992) Success with sacrospinous suspension of the prolapsed vaginal result. Surg Gynecol Obstet 175:419–420
Shull BL, Capen CV, Riggs MW, Kuehl TJ (1992) Preoperative and postoperative analysis of site-specific pelvic support defects in 81 women treated with sacrospinous ligament suspension and pelvic reconstruction. Am J Obstet Gynecol 166:1764–1771
Lin TY, Su TH, Wang YL, Lee MY, Hsieh CH, Wang KG et al (2005) Risk factors for failure of transvaginal sacrospinous uterine suspension in the treatment of uterovaginal prolapse. J Formos Med Assoc 104:249–253
Dietz V, de Jong J, Huisman M, Koops SS, Heintz P, Van der Vaart H (2007) The effectiveness of the sacrospinous hysteropexy for the primary treatment of uterovaginal prolapse. Int Urogynecol J Pelvic Floor Dysfunct 18:1271–1276
Krause HG, Goh JTW, Sloane K, Higgs P, Carey MP (2006) Laparoscopic sacral suture hysteropexy for uterine prolapse. Int Urogynecol J Pelvic Floor Dysfunct 17:378–381
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Vierhout ME, Stoutjesdijk J, Spruijt J (2006) A comparison of preoperative and intraoperative evaluation of patients undergoing pelvic reconstructive surgery for pelvic organ prolapse using the pelvic organ prolapse quantification system. Int Urogynecol J Pelvic Floor Dysfunct 17:46–49
Miyazaki FS (1987) Miya Hook ligature carrier for sacrospinous ligament suspension. Obstet Gynecol 70:286–288
Jacquetin B (1998) Using the Endo Stitch forceps via the vagina: purely by palpation? J Gynecol Obstet Biol Reprod (Paris) 27:213–214
Winkler HA, Tomeszko JE, Sand PK (2000) Anterior sacrospinous vaginal vault suspension for prolapse. Obstet Gynecol 95:612–615
Aigmueller T, Riss P, Dungl A, Bauer H (2008) Long-term follow-up after vaginal sacrospinous fixation: patient satisfaction, anatomical results and quality of life. Int Urogynecol J Pelvic Floor Dysfunct 19:965–969
Paraiso MF, Ballard LA, Walters MD, Lee JC, Mitchinson AR (1996) Pelvic support defects and visceral and sexual function in women treated with sacrospinous ligament suspension and pelvic reconstruction. Am J Obstet Gynecol 175:1423–1431
Karram MM, Walters MD (1993) Pelvic organ prolapse: enterocele and vaginal vault prolapse. Mosby, St. Louis, pp 245–252
Goldberg RP, Tomezsko JE, Winkler HA, Koduri S, Culligan PJ, Sand PK (2001) Anterior or posterior sacrospinous vaginal vault suspension: long-term anatomic and functional evaluation. Obstet Gynecol 98:199–204
Acknowledgements
The authors would like to thank the National Science Council of the Republic of China, the China Medical University, and the China Medical University Hospital for financially supporting this research under Contract NSC 96-2815-C-039-035-B, CMU96-035, and DMR-97-076.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, HY., Chiu, TH., Ho, M. et al. Analysis of risk factors associated with surgical failure of sacrospinous suspension for uterine or vaginal vault prolapse. Int Urogynecol J 20, 387–391 (2009). https://doi.org/10.1007/s00192-008-0780-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-008-0780-y