Abstract
One common method for treating recurrent genital herpes outbreaks is 3–5 day episodic therapy with nucleoside analogues. However, since maximum viral replication occurs within 24 h after the onset of symptoms, short-term patient-initiated episodic therapy started at prodromal onset or at the first appearance of lesions in patients without a prodrome may represent an important option. In a recent randomized trial, single-day famciclovir treatment decreased lesion healing time and the duration of pain and other symptoms by approximately 2 days compared to placebo, and prevented progression to a full outbreak in almost one in four patients. Because single-day treatment is more convenient than traditional therapies, it may lead to improved patient compliance and better overall management of recurrent genital herpes outbreaks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recurrent genital herpes outbreaks are predominantly caused by herpes simplex virus type 2 (HSV-2), although the incidence of genital herpes caused by herpes simplex virus type 1 (HSV-1) is rising due to changing attitudes about oral-genital sexual behavior [10]. Approximately one in four adults in the United States is seropositive for HSV-2 [7], an incurable infection that initially enters the body through mucous membranes or abraded skin. Once primary infection has occurred, the virus remains dormant in the dorsal root ganglia, where it can reactivate to cause uncomfortable, recurrent outbreaks [20].
HSV-2 infection is somewhat more prevalent in women than in men [7], and can have a profound psychological impact as well as physical repercussions, resulting in a decrease in measures of quality of life. The fear of spreading the infection can result in lowered self-esteem or sexual desire and, less commonly, social phobia and depression [6]. In addition, patients with genital herpes have a significantly increased risk of acquiring human immunodeficiency virus (HIV) [8].
Episodic treatment for genital herpes
Although there is no cure for HSV-2 infection, patients have two treatment options: treating outbreaks as they occur (episodic therapy), or attempting to prevent future outbreaks (suppressive therapy). Suppression with daily oral antivirals may be most appropriate for patients with frequent or uncomfortable recurrences and to reduce genital herpes transmission to sexual partners [4]. Although suppressive therapy is effective, one quarter to one half of patients on suppressive therapy have at least one recurrence per year [5, 14].
Although episodic treatment has not been proven to reduce the risk of transmission, it still remains an important option for patients who do not want to take daily suppressive therapy, are not concerned about the frequency of recurrences, or are not sexually active. The best method for administering episodic therapy is to make medication readily available to patients to self-administer at the first onset of symptoms or lesions [16]. This type of patient-initiated episodic therapy has been successfully used in previous clinical trials of recurrent genital herpes [13, 15]. The ability to treat recurrences sooner may also help decrease the duration of an outbreak or halt progression to a full outbreak [9, 13, 15, 19]. This expert opinion will examine the results from a recently published clinical trial about patient-initiated, single-day oral antiviral therapy (famciclovir) for recurrent genital herpes [2] and compare its efficacy with data from currently available therapies.
Treatment of recurrent genital herpes with oral antivirals
Patients with recurrent episodes of genital herpes often experience such prodromal symptoms as itching, tingling, burning, and pain, with papules and vesicles typically forming 12–24 h after onset of these symptoms [3]. Maximum HSV-2 concentration and lesion pain usually occur within the first 24 h of onset of these prodromal symptoms [3]. Under the assumption that one can extrapolate from the pathogenesis of herpes labialis [17], it is thought that the most effective way to treat recurrent genital herpes with antiviral therapy would be within the first 24 h after the onset of clinical symptoms, when viral replication is highest [16]. Oral antivirals, acting as nucleoside analogues enter infected cells and bind to viral thymidine kinase, resulting in their phosphorylation. After the antivirals are further phosphorylated by cellular enzymes, they compete with nucleosides to bind to the viral DNA polymerase, resulting in polymerase inactivation and a decrease in viral replication [16].
Although topical acyclovir was initially used to treat recurrent genital herpes, it has since been proven ineffective and is no longer recommended [1, 12]. Today, the most commonly prescribed drugs are the oral antivirals acyclovir, valacyclovir, and famciclovir. Acyclovir is approved for 5-day episodic treatment, although a 2-day regimen has been shown to be effective [13, 19]. Acyclovir is effective, but its poor bioavailability requires more frequent dosing. Valacyclovir, a prodrug of acyclovir, has a higher bioavailability than acyclovir and has been approved for 3-day episodic treatment [9, 14]. Famciclovir, a prodrug of penciclovir, is currently indicated for 5-day treatment [11, 15]. The high bioavailability of famciclovir (77%) and the rapid onset of viral replication in recurrent genital herpes suggested that this medication would be efficacious in an even shorter single-day treatment regimen.
Data from single-day famciclovir clinical trial
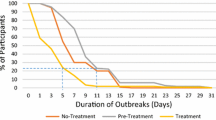
A clinical trial was performed to assess whether single-day famciclovir was effective in treating recurrent genital herpes in immunocompetent individuals [2]. The 329 study participants experiencing a recurrence of genital herpes were predominately female (71%) and 48% had had more than six recurrences in the preceding year. Participants were given a single day of famciclovir 1,000 mg bid or matching placebo and were instructed to take the medication within 6 h of the onset of prodromal symptoms and/or genital herpes lesions during their next recurrence. The trial results showed that a single-day regimen of famciclovir significantly decreased lesion-healing time and significantly reduced time to resolution of all symptoms by 2 days, as compared to placebo. Famciclovir also halted the progression to a full genital herpes outbreak in almost one in four patients. Adverse events were of mild-to-moderate intensity and were similar to the adverse events experienced by the placebo group.
Although no head-to-head studies have been conducted between single-day famciclovir and other oral antivirals, patients who received single-day famciclovir experienced effects similar to those seen in previous clinical trials of traditional longer-term therapies (Table 1) [2, 9, 13, 15, 18, 19]. Single-day therapy appears to inhibit viral replication enough to significantly reduce both symptoms and the tissue damage characteristic of a full outbreak, preventing progression to a full recurrence in some cases.
Conclusion
The rapid onset of viral replication in recurrent genital herpes suggests that a shorter course of therapy would be as efficacious as traditional treatments. Patient-initiated single-day therapy could prove helpful for obstetricians/gynecologists who treat patients with genital herpes, as it may provide a more convenient option for treating the disease, and could help to promote patient compliance. High bioavailability, ease of use, and the added benefit of preventing progression to a full genital herpes outbreak in some patients make famciclovir an excellent candidate for single-day patient-initiated episodic therapy.
References
ACOG Committee on Practice Bulletins—Gynecology (2004) Obstet Gynecol 104(5 pt 1):1111–1118
Aoki FY, Tyring S, Mitoma-Diaz F, Gross G, Gao J, Hamed K (2006) Single-day, patient-initiated famciclovir therapy for recurrent genital herpes: a randomized, double blind, placebo-controlled trial. Clin Infect Dis 42:8–13
Brown ZA, Kern ER, Spruance SL, Overall JC Jr (1979) Clinical and virologic course of herpes simplex genitalis. West J Med 130:414–421
Corey L, Wald A, Patel R, Sacks SL, Tyring SK, Warren T, et al (2004) Once-daily valacyclovir to reduce the risk of transmission of genital herpes. N Engl J Med 350:11–20
Diaz-Mitoma F, Sibbald G, Shafran SD, Boon R, Saltzman RL (1998) Oral famciclovir for the suppression of recurrent genital herpes: a randomized controlled trial. JAMA 280:887–892
Drob S, Loemer M, Lifshutz H (1985) Genital herpes: the psychological consequences. Br J Med Psychol 58(Pt 4):307–315
Fleming DT, McQuillan GM, Johnson RE, et al (1997) Herpes simplex virus type 2 in the United States, 1976–1994. N Engl J Med 337:1105–1111
Freeman EE, Weiss HA, Glynn JR, Cross PL, Whitworth JA, Hayes RJ (2006) Herpes simplex virus 2 infection increases HIV acquisition in men and women: systematic review and meta-analysis of longitudinal studies. AIDS 20:73–83
Leone PA, Trottier S, Miller JM (2002) Valacyclovir for episodic treatment of genital herpes: a shorter 3-day treatment course compared with 5-day treatment. Clin Infect Dis 34:958–962
Malkin JE (2004) Epidemiology of genital herpes simplex virus infection in developed countries. Herpes 11(suppl 1):2A–23A
Pue MA, Benet MA (1993) Pharmacokinetics of famciclovir in man. Antivir Chem Chemother 4(suppl 1):47–55
Reichman RC, Badger GJ, Guinan ME, Nahmias AJ, Keeney RE, Davis LG, et al (1983) Topically administered acyclovir in the treatment of recurrent herpes simplex genitalis: a controlled trial. J Infect Dis 147:336–340
Reichman RC, Badger GJ, Mertz GJ, Corey L, Richman DD, Connor JD, et al (1984) Treatment of recurrent genital herpes simplex infections with oral acyclovir. A controlled trial. JAMA 251:2103–2107
Reitano M, Tyring S, Lang W, Thoming C, Worm AM, Borelli S, et al (1998) Valaciclovir for the suppression of recurrent genital herpes simplex virus infection: a large-scale dose range-finding study. J Infect Dis 178:603–610
Sacks SL, Aoki FY, Diaz-Mitoma F, Sellors J, Shafran SD (1996) Patient-initiated, twice-daily oral famciclovir for early recurrent genital herpes. JAMA 276:44–49
Spruance SL (1995) Herpes simplex labialis. In: Sacks SL, Straus SE, Whitley RJ, et al (eds) Clinical management of herpes viruses. IOS Press, Amsterdam, pp 3–42
Spruance SL, Wenerstrom G (1984) Pathogenesis of recurrent herpes simplex labialis. IV. Maturation of lesions within 8 hours after onset and implications for antiviral treatment. Oral Surg Oral Med Oral Pathol 58:667–671
Tyring SK, Douglas JM Jr, Corey L, Spruance SL, Esmann J (1998) A randomized, placebo-controlled comparison of oral valacyclovir and acyclovir in immunocompetent patients with recurrent genital herpes infections. The Valaciclovir International Study Group. Arch Dermatol 134:185–191
Wald A, Carrell D, Remington M, Kexel E, Zeh J, Corey L (2002) Two-day regimen of acyclovir for treatment of recurrent genital herpes simplex virus type 2 infection. Clin Infect Dis 34:944–948
Whitley RJ, Kimberlin DW, Roizman B (1998) Herpes simplex viruses. Clin Infect Dis 26:541–555
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Tyring, S., Richwald, G. & Hamed, K. Single-day therapy: an expert opinion on a recent development for the episodic treatment of recurrent genital herpes. Arch Gynecol Obstet 275, 1–3 (2007). https://doi.org/10.1007/s00404-006-0234-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-006-0234-z