Abstract
Verruca vulgaris is always stubborn to treat. We applied a new combined therapy of local recombinant human interferon alpha 1b (rhIFNα1b) injection plus acupuncture on verruca vulgaris recently to evaluate the efficacy and safety of the combined therapy. The retrospective study was conducted in The First Hospital of China Medical University from 2018 to 2020. Patients with verruca vulgaris were included. Combined therapy with local rhIFNα1b injection plus acupuncture was set as treatment group, rhIFNα1b injection and carbon dioxide (CO2) laser were set as control groups. A total of 2415 patients were included in the study. The cure rates were 81.85%, 85.93%, and 100% in combined group, rhIFNα1b group, and CO2 laser group, separately. All lesions cured in combined group were located on hands or feet, while majority of lesions cured in other groups were located on other sites. For patients with medium/big single lesion or 6–9 lesions, less treatment times were needed in combined group than rhIFNα1b group. For patients with small single, two to five or more than ten lesions, the treatment times of combined group and rhIFNα1b group were comparable. All patients complained of pain in varying degrees when local injection or laser irradiation. Compared with CO2 laser group, more fever, less swelling or scar was reported in combined group. In conclusion, combined therapy of local rhIFNα1b plus acupuncture was beneficial for verruca vulgaris with limited adverse effects. The therapy was more acceptable by younger female patients with verruca vulgaris.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Verruca vulgaris, also named as common wart, is a benign skin disorder infected by human papillomavirus (HPV). It is charactered by acanthosis, papillomatous hyperplasia, hyperkeratosis, and parakeratosis in epidermis. The population prevalence rate ranges from 7 to 10% worldwide [1]. Verruca vulgaris usually locates on hands or feet, but sometimes on arms or legs. Various modalities have been applied for verruca vulgaris, such as ablation of warts (cryosurgery, laser, electrodesiccation, salicylic acid, silver nitrate, imiquimod, and trichloroacetic acid), interruption of the organic process (podophyllotoxin, intralesional bleomycin, and 5-fluorouracil), and surgical excision. However, most of the therapies are invasive, painful or inclined to relapse [2]. Therefore, more alternative modalities are urgently needed.
Interferon (IFN) is an important protein discovered in 1957 [3]. It is beneficial to anti-virus and immune regulation [4]. There are three types of IFNs, including Type I (IFNα, IFNβ), Type II (IFNγ), and Type III (IFNλ). IFNα arises from plasmacytoid dendritic cells, it upregulates genes involved in immune processes by recognizing microbial nucleic acids/immune complexes and binding to Type I IFN receptor, thus restricts viral replication and enhances B cell responses [5]. IFNα1b has been applied to some viral diseases and malignant tumors. It ameliorates symptoms of neonatal respiratory syncytial virus pneumonia with minimal adverse effects [6] and prolongs survival time of patients with unresectable metastatic melanoma [7]. Combined therapy of arbidol and IFNα1b decreases the severity of moderate COVID-19 pneumonia [8]. Recombinant human IFNα1b (rhIFNα1b) is a kind of genetic engineering IFN. Early use of rhIFNα1b in hospitalized infants with lower respiratory tract infections (viral pneumonia, wheezy bronchitis, or bronchiolitis) could prevent subsequent wheezing [4]. rhIFNα1b gradually regressed lesions of a patient diagnosed as subcutaneous panniculitis-like T cell lymphoma without relapsing in the 10-month follow-up [9]. In general, IFNα1b is injected subcutaneously or intramuscularly. To obtain higher local concentration, intralesional injection has also been tried. Zeng et al. reported a successful case of cutaneous pseudolymphoma on the nose with combination of intralesional IFNα1b and compound betamethasone [10].
Acupuncture is a traditional Chinese therapy with a long history of more than 3000 years. It is effective for numerous disorders, such as inflammation, pain [11], and psychosocial abnormalities (anxiety, depression) [12]. Acupuncture is a relatively safe complementary and alternative nonpharmacological therapy [13]. The potential mechanisms might be stimulating meridians of human body, regulating blood circulation and improving immune function [14]. Recently, it has been applied to several dermatoses, such as psoriasis, atopic dermatitis, urticaria, and pruritus [15, 16]. Ursini et al. reported that a chronic HPV wart patient with HIV infection who was resistant to cryotherapy was cured after 58 sessions of systemic acupuncture over 19 months [17]. To our knowledge, no intralesional acupuncture application has been reported in dermatoses till now.
In the past 3 years, we innovatively applied a combined therapy of local intralesional rhIFNα1b followed by acupuncture to patients with verruca vulgaris and obtained satisfied effects. Herein, we retrospectively reported the efficacy and safety of the combined therapy.
Methods
Patients with verruca vulgaris treated at outpatient clinic of Department of Dermatology, The First Hospital of China Medical University from January 1, 2018 to December 31, 2020 were included in the present retrospective study. Patients treated with combined therapy of local intralesional rhIFNα1b (Tri-Prime Gene, Beijing, China) followed by intralesional acupuncture was set as treatment group, those with local intralesional rhIFNα1b or carbon dioxide (CO2) laser were set as control groups, separately. For the combined group and rhIFNα1b group, rhIFNα1b was injected intralesionally for each lesion. Subsequently, acupuncture needles were injected into the bottom of the biggest one or two lesions (20 needles/lesion), and were extracted 30 min later. The procedure was repeated at an interval of 7–10 days. Oral immune modulator (pidotimod, thymosin or transfer factor), or topical imiquimod cream was additionally added according to individual conditions. Oral immune modulators were taken for 1–3 months according to the drug instructions, whereas imiquimod was topically applied on the lesions every other day till the lesions were disappeared. For CO2 group, CO2 laser was applied to all lesions as described previously [18].
Location, number, and size of the lesions, age and gender of the patients, and treatment sessions were collected. Digital photographs were taken with a camera at focal distance of 1.5 m (Canon 60D, Japan) every time before treatment until the lesions were disappeared and 1, 2, 3 months after the last treatment. Two blinded dermatologists individually evaluated the clinical improvements. Cure was defined as “all lesions were disappeared”. Cure rate was calculated by dividing the number of cured patients with that of all patients in the specific group. Any adverse effect during or after treatment, such as fever, swelling, hyperpigmentation, scar or infection, was reported by the patients and recorded by the dermatologists. The recurrence rate was evaluated 3 months after the last treatment.
All data were analyzed by GraphPad Prism version 9.0.0 (GraphPad Software, San Diego, California, USA). Chi-squared test and one-way ANOVA were performed to compare the differences between different groups. P < 0.05 was considered as statistically significant.
Results
A total of 2415 patients with average age of 30.62 ± 14.34 years were included in the study. Cured patients in combined group (28.87 ± 12.40 years) was younger than those in CO2 laser group (34.93 ± 16.00 years) (P < 0.05), but comparable with rhIFNα1b group (27.72 ± 14.16 years) (P > 0.05, Table 1). The cure rates were 81.85% (929/1135), 85.93% (464/540), and 100% (740/740) in combined group, rhIFNα1b group, and CO2 laser group, separately. The lesions of 781, 1109, 243 patients were, respectively, located on hands, feet, and other sites (arms and legs) in the three groups. Lesions cured by combined group were all located on hands or feet, while majority of lesions cured by other methods were located on arms or legs (P < 0.05, Table 1). For gender comparison, there was no statistical significance between combined group and rhIFNα1b group (P > 0.05), but more male patients were seen in CO2 laser group (P < 0.05).
Sessions of single lesion
There were 929, 464, and 740 patients with single lesion included in the present study in combined group (Figs. 1, 2), rhIFNα1b group (Fig. 3), and CO2 laser group (Fig. 4), separately.
For small lesions (diameter < 5 mm), there was no statistical difference in sessions between combined group (4.40 ± 3.94 sessions) and rhIFNα1b group (4.61 ± 2.37 sessions) (P > 0.05). The sessions of both groups were more than those of CO2 laser group (1 session) (P < 0.05). For subgroup analyses in combined group, no statistical difference between rhIFNα1b + acupuncture only group and rhIFNα1b + acupuncture + imiquimod group was found. For subgroup analyses in rhIFNα1b groups, there were no statistical significances between rhIFNα1b + immune modulator group/rhIFNα1b + imiquimod group and rhIFNα1b group (P > 0.05) (Table 2).
For medium lesions (diameter 6-10 mm), less sessions were needed in the combined group (5.94 ± 3.38 times) than those in rhIFNα1b group (9.90 ± 3.86 times) (P < 0.05). The sessions in both groups were more than those of CO2 laser group (1.10 ± 0.30) (P < 0.05). There was no statistical difference in combined group for subgroup analyses (rhIFNα1b + acupuncture only group vs. rhIFNα1b + acupuncture + immune modulator group, rhIFNα1b + acupuncture only group vs. rhIFNα1b + acupuncture + imiquimod group) (P > 0.05). For rhIFNα1b subgroups, the sessions in rhIFNα1b only group (10.06 ± 3.32) were more than those in rhIFNα1b + immune modulator group (5.75 ± 1.63) (P < 0.0001), while there was no statistical difference between rhIFNα1b only group and rhIFNα1b + imiquimod group (11.40 ± 4.13) (P > 0.05) (Table 2).
For big lesions (diameter > 11 mm), less sessions in combined group (8.94 ± 4.42 times) were needed than those in rhIFNα1b group (12.33 ± 4.71 times, P < 0.05). The sessions of both groups were more than those in CO2 laser group (1.23 ± 0.42 times) (P < 0.05). For rhIFNα1b subgroups, there was no statistical difference between rhIFNα1b only group (10.83 ± 3.07) and rhIFNα1b + imiquimod group (13.83 ± 5.52) (P > 0.05) (Table 2).
Sessions of plural lesions
There were 468, 268, and 161 patients with plural lesions included in the present study in combined group, rhIFNα1b group, and CO2 laser group, separately.
For patients with 2–5 lesions, there was no statistical difference in sessions between combined group (6.25 ± 3.64 times) and rhIFNα1b group (6.66 ± 3.60 times) (P > 0.05). The sessions in both groups were more than those of CO2 laser group (1.08 ± 0.27 times) (P < 0.05). For subgroup analyses in combined group, there were no statistical significances between rhIFNα1b + acupuncture only group and rhIFNα1b + acupuncture + oral immune modulator group, as well as between rhIFNα1b + acupuncture only group and rhIFNα1b + acupuncture + imiquimod group. For subgroup analyses in rhIFNα1b subgroups, no statistical significances were seen between rhIFNα1b only group and rhIFNα1b + immune modulator group, as well as between rhIFNα1b only group and rhIFNα1b + imiquimod group (P > 0.05).
For patients with 6–9 lesions, less sessions in combined group (6.73 ± 3.70 times) were needed than those in rhIFNα1b group (9.44 ± 4.95 times, P < 0.05). There were no statistical significances between combined subgroups (rhIFNα1b + acupuncture only group vs. rhIFNα1b + acupuncture + immune modulator group, rhIFNα1b + acupuncture only group vs. rhIFNα1b + acupuncture + imiquimod group), as well as rhIFNα1b subgroups (rhIFNα1b only group vs. rhIFNα1b + immune modulator, rhIFNα1b only group vs. rhIFNα1b + imiquimod group) (P > 0.05).
For patients with more than ten lesions, there was no statistical difference in sessions between combined group (10.67 ± 4.52 times) and rhIFNα1b group (10.87 ± 3.48 times) (P > 0.05). There were no statistical significances between combined subgroups (rhIFNα1b + acupuncture only group vs. rhIFNα1b + acupuncture + immune modulator group, rhIFNα1b + acupuncture only group vs. rhIFNα1b + acupuncture + imiquimod group), so did rhIFNα1b subgroups (rhIFNα1b only group vs. rhIFNα1b + imiquimod group) (P > 0.05) (Table 2).
Adverse effects
All of the patients complained of varying degrees of pain in local injection or laser ablation. More patients in combined group (75.03%, 697/929) and rhIFNα1b group (75.65%, 351/464) suffered from mild fever than those in CO2 laser group (0%, 740) (P < 0.05). The fever recovered in 1 or 2 days without any treatment. Less patients in combined group complained of swelling (13.02%, 121/929 vs. 100%, 740/740) and scar (1.61%, 15/929 vs. 22.97%, 170/740) than those of CO2 laser group (P < 0.05). No statistical differences were found in hyperpigmentation and infection between combined group and control groups. The recovery time of CO2 laser lasted for 2 weeks.
Recurrence rate
The recurrence rates at 3 months after the last treatment were 14.17% (121/854), 17.01% (85/498), and 25.89% (145/560) in combined group, rhIFNα1b group, and CO2 laser group, separately.
Discussion
In the present study, we first applied combined therapy of intralesional rhIFNα1b injection and local acupuncture on verruca vulgaris, and got excited efficacy. For single lesion, the sessions varied according to the size of the lesions. The sessions between combined group and rhIFNα1b group were comparable if the lesion was small, whereas the sessions of combined group were less than those of rhIFNα1b group if the lesion diameter was bigger than 6 mm. The results illustrated that intralesional rhIFNα1b injection was a good modality for small single verruca vulgaris, and additional local acupuncture decreased sessions for medium and big lesions. Less sessions represented more convenient and easier to be accepted by the patients. For plural lesions, sessions increased according to the number of the lesions. When there were 6–9 lesions, the sessions of the combined group were less than those of rhIFNα1b group. But no statistical differences were found between the combined group and rhIFNα1b group with two to five or more than ten lesions. Traditional modalities, such as cryosurgery, electrodesiccation, bleomycin, 5-fluorouracil, and surgical excision, were applied on all lesions, but acupuncture in the present study was applied on the biggest one or two lesions, indicating a simpler modality for the present combined therapy.
As shown in the present study, the cure rates and side effects (swelling and scar) of both rhIFNα1b + acupuncture group and rhIFNα1b group were lower than those of CO2 group. Therefore, the combined therapy might be accepted by more young female patients because of cosmetic reasons. Moreover, the cure rate of rhIFNα1b + acupuncture group was a little lower than that of rhIFNα1b group, but additional local acupuncture decreased sessions of medium and big lesions. The recurrence rate after 3 months in combined group and rhIFNα1b group was lower than that in CO2 laser group, indicating that the combined therapy of rhIFNα1b and acupuncture was an alternative therapy for verruca vulgaris.
In the past, oral immune modulator and topical imiquimod were considered as traditional modalities for verruca vulgaris. However, the modalities cost such a long time and were inconvenient for patients. Some of the patients gave up because of the troublesome procedure. In our study, the combined therapy was applied at an interval of 7–10 days in hospital, which improved the compliances of patients. Moreover, oral immune modulator and local imiquimod did not reduce the sessions of the combined therapy or rhIFNα1b under most conditions, illustrating limited efficacies of oral immune modulators and local imiquimod on verruca vulgaris.
Some potential mechanisms might participate in the combined therapy. First, verruca vulgaris is infected by HPV, which infects keratinocytes and induces minimal inflammation without lysing infected cells. Moreover, HPV decreases the maturation and antigen presentation function of the antigen presenting immune cells (Langerhans cells) [19], inhibits Type I IFN signaling pathway and results in the transcription of IFN-stimulated genes with the function of anti-virus [20]. IFN induces the production of anti-viral proteins against viral protein translation and transcription, regulates immune function by TH1 and macrophage/natural killer cell, increases antigen expression of HPV on infected cells, changes the fluidity of cell membrane by decreasing viral replication and inhibits differentiation of HPV-infected cells by decreasing HPV reproduction rate [21]. rhIFNα1b is a human original regulatory cytokine of Type I IFN family with excellent anti-viral activity, anti-proliferation, and immunomodulation [22]. It eliminates virus by blocking viral replication and enhancing innate immune response [23]. Second, intralesional acupuncture blocks the microcirculation at the bottom of the warts, thus induces shrinkage of the lesions. The combined therapy acuminates eliminating of the warts.
Conclusion
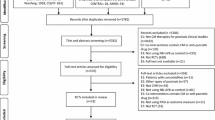
The combined therapy of local applied rhIFNα1b and acupuncture was beneficial for verruca vulgaris. However, there were some limitations. First, the retrospective study was only from one hospital, that random clinical trials (RCTs) from multiple centers would be more persuasive. Second, no long follow-up was reported in the present study; thus, the recurrence rate was incomparable. Therefore, more RCTs with long follow-up should be taken in the future to confirm the results.
References
Veitch D, Kravvas G, Al-Niaimi F (2017) Pulsed dye laser therapy in the treatment of warts: a review of the literature. Dermatol Surg 43:485–493. https://doi.org/10.1097/DSS.0000000000001023
Singh Mehta KI, Mahajan VK, Chauhan PS, Chauhan S, Sharma V, Rawat R (2019) Evaluation of efficacy and safety of intralesional bleomycin in the treatment of common warts: results of a pilot study. Indian J Dermatol Venereol Leprol 85:397–404. https://doi.org/10.4103/ijdvl.IJDVL_519_17
Isaacs A, Lindenmann J (1957) Virus interference. I. The interferon. Proc R Soc Lond B Biol Sci 147:258–267. https://doi.org/10.1098/rspb.1957.0048
Yang L, Zhang G, Huang L, Ren X, Su Y, Wang C, Shi Y, Li L, Shan H, Chen J, Xiong J, Xue X, Song S, Zhao L, An S, Yu H, Cao H, Zhao L, Li M, Sheng X, Wang Y (2021) The effect of recombinant human interferon alpha1b treatment of infants hospitalized with lower respiratory tract infection on subsequent wheezing. J Pediatr 97:617–622. https://doi.org/10.1016/j.jped.2020.12.005
Stockfelt M, Lundell AC, Hetland ML, Ostergaard M, Uhlig T, Heiberg MS, Haavardsholm EA, Nurmohamed MT, Lampa J, Nordstrom D, Petersen KH, Gudbjornsson B, Grondal G, Aldridge J, Andersson K, Blennow K, Zetterberg H, van Vollenhoven R, Rudin A (2021) Plasma interferon-alpha is associated with double-positivity for autoantibodies but is not a predictor of remission in early rheumatoid arthritis-a spin-off study of the NORD-STAR randomized clinical trial. Arthritis Res Ther 23:189. https://doi.org/10.1186/s13075-021-02556-1
He L, Yang L, Zhang H, Luo Q (2020) Efficacy and safety of interferon on neonates with respiratory syncytial virus pneumonia. Exp Ther Med 20:220. https://doi.org/10.3892/etm.2020.9350
Shi Q, Liu L, Zhang W, Zhao Y, Liu Y, Zhu G, Guo W, Zhao T, Zhao J, Wang L, Li C, Gao T (2021) Interferon-alpha1b for the treatment of metastatic melanoma: results of a retrospective study. Anticancer Drugs 32:1105–1110. https://doi.org/10.1097/CAD.0000000000001120
Yin P, Meng J, Chen J, Gao J, Wang D, Liu S, Guo Q, Zhu M, Zhang G, Liu Y, Li Y, Zhang G (2021) Antiviral drugs arbidol and interferon alpha-1b contribute to reducing the severity of COVID-19 patients: a retrospective cohort study. Virol J 18:142. https://doi.org/10.1186/s12985-021-01617-w
Sun D, Zheng S, Hong YX, Chen HD, Gao XH (2021) Subcutaneous panniculitis-like T cell lymphoma presented as erythema nodosum: A case report. Dermatol Ther 34:e14572. https://doi.org/10.1111/dth.14572
Zeng SH, Chen SY, Tang XY, Wang L (2020) A case of cutaneous pseudolymphoma with a distinctive appearance treated successfully by intralesional interferon alpha-1b and corticosteroids. Dermatol Ther 33:e13410. https://doi.org/10.1111/dth.13410
Yu ML, Wei RD, Zhang T, Wang JM, Cheng Y, Qin FF, Fu SP, Lu ZG, Lu SF (2020) Electroacupuncture relieves pain and attenuates inflammation progression through inducing IL-10 production in CFA-induced mice. Inflammation 43:1233–1245. https://doi.org/10.1007/s10753-020-01203-2
Du J, Tao J, Xu M, Wang R, Lin L, Huang X, Li Q, Lu X (2021) The effects of acupuncture for patients with psoriasis: Study protocol for a randomized controlled trial. Medicine 100:e26042. https://doi.org/10.1097/MD.0000000000026042
Bai H, Xu S, Wu Q, Xu S, Sun K, Wu J, Xia X, Liu Y, Zhang H, Lu S (2020) Clinical events associated with acupuncture intervention for the treatment of chronic inflammation associated disorders. Mediators Inflamm 2020:2675785. https://doi.org/10.1155/2020/2675785
Liu FG, Tan AH, Peng CQ, Tan YX, Yao MC (2021) Efficacy and safety of scalp acupuncture for insomnia: a systematic review and meta-analysis. Evid Based Complement Alternat Med 2021:6621993. https://doi.org/10.1155/2021/6621993
Cheng X, Lai J, Zhang Y, Lin L, Xu D, Zhong Z, Wu Q, Liu J (2021) Efficacy and safety of fire acupuncture for psoriasis vulgaris: a protocol of systematic review and meta-analysis of randomized clinical trials. Medicine 100:e25038. https://doi.org/10.1097/MD.0000000000025038
Ma C, Sivamani RK (2015) Acupuncture as a treatment modality in dermatology: a systematic review. J Altern Complement Med 21:520–529. https://doi.org/10.1089/acm.2014.0274
Ursini T, Polilli E, Congedo G, Tontodonati M, Di Masi F, Mazzotta E, Parruti G, Pippa L (2011) Complete healing of a giant wart in a severely immune-compromised patient with HIV infection treated with acupuncture. Case Rep Dermatol 3:175–180. https://doi.org/10.1159/000331427
Boroujeni NH, Handjani F, Saki N (2020) CO2 laser treatment for plantar warts in children: a case series. Dermatol Ther 33:e13414. https://doi.org/10.1111/dth.13414
Yuan J, Ni G, Wang T, Mounsey K, Cavezza S, Pan X, Liu X (2018) Genital warts treatment: beyond imiquimod. Hum Vaccin Immunother 14:1815–1819. https://doi.org/10.1080/21645515.2018.1445947
Song JY, Han JH, Song Y, Lee JH, Choi SY, Park YM (2021) Epigallocatechin-3-gallate can prevent type 2 human papillomavirus E7 from suppressing interferon-stimulated genes. Int J Mol Sci 22:2418. https://doi.org/10.3390/ijms22052418
Czelusta AJ, Evans T, Arany I, Tyring SK (1999) A guide to immunotherapy of genital warts: focus on interferon and imiquimod. BioDrugs 11:319–332. https://doi.org/10.2165/00063030-199911050-00004
Fox LE, Locke MC, Lenschow DJ (2020) Context is key: delineating the unique functions of IFNalpha and IFNbeta in disease. Front Immunol 11:606874. https://doi.org/10.3389/fimmu.2020.606874
Lin F, Shen K (2020) Type I interferon: from innate response to treatment for COVID-19. Pediatr Investig 4:275–280. https://doi.org/10.1002/ped4.12226
Funding
This work was supported by the National Natural Science Foundation of China (No. 82103758, 81903198).
Author information
Authors and Affiliations
Contributions
LiangHong Chen, BiHuan Xiao and JingYu Wang wrote the main manuscript text, Yan Wu, Yan Sun and XingHua Gao edited the manuscript, Shuai Qiao and Qian An prepared figures 1-4. All authors reviewed and approved the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that he they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, L., Wu, Y., Sun, Y. et al. Combined therapy of local recombinant human interferon α1b injection and acupuncture on verruca vulgaris: a retrospective study. Arch Dermatol Res 315, 2365–2373 (2023). https://doi.org/10.1007/s00403-023-02627-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-023-02627-0