Abstract
Dermatological emergency is defined as any urgent/immediate care. Dermatological conditions compromise about 5–8% of all cases presenting to the emergency department. A grading system can help dermatologist’s and allied medical personnel to triage a patient accordingly. Currently no severity grading for dermatological emergencies is available. All patients seen in OPD for dermatological consultations requiring urgent interventions were included. Detailed history and clinical examination were done. Patients were assessed according to the onset, symptoms, distribution, examination, body surface area percentage and mucosal involvement. The severity was graded separately based on comorbidities and systemic involvement. Grade I was no comorbidity or systemic involvement. Grade II was 1 comorbidity or systemic involvement. Grade III was 2 comorbidities or systemic involvement. Grade IV was > 2 comorbidities or multiorgan involvement. Interesting emergency cases observed in Covid period were noted. There were 202 cases, the most common age group was 19–64 (69.8%). Male (49%) and females (51%) had equal preponderance. Most common emergency was acute urticaria with or without angioedema (25.24%). There were 113 (55.94%) inpatients and 89 (44.05%) were outpatients. Acute on chronic onset (34.5%), pain (41.6%), vesicles (30.1%), erosion (23.9%), ulcers (9.7%) and more than 50% body surface area involvement (64.6%) were seen more in admitted cases. Grade I was most common for both comorbidities and systemic involvement. However, grades II, III and IV were higher in admitted cases for both grading systems. The presence of comorbidities and systemic involvement increases the severity of dermatological emergency. Six patients had relapse. Seven patients had methotrexate toxicity. The proposed grading system based on comorbidities and systemic involvement helps to assess the severity of dermatological emergencies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dermatology is an outpatient speciality. Dermatological conditions compromise about 5–8% of all cases presenting to the emergency department. It is important to recognize conditions requiring inpatient management referral [1].
In dermatology, emergencies are more uncommon than in other branches of medicine; however, emergencies with a high mortality rate negatively affect the quality of life, requiring hospitalization and even stays in intensive care units do occur [2]. Furthermore, healthcare professionals in an emergency or urgent care settings must appropriately triage patients with dermatological findings. A grading system based on comorbidities and systemic involvement can help in early recognition of these conditions and reduce the morbidity and mortality associated with these conditions.
The onset of COVID-19 pandemic has changed the socio-economic structure of the country. The scenario of dermatology consultations has also changed. In India lockdown period extended from March 2020 to May 2021; with unlock being done in a phased manner.
Various dermatological conditions are well associated and show increased trend during COVID-19 pandemic. There has been a change in profile of dermatological cases with hair disorders such as telogen effluvium, alopecia areata being most common. Other conditions that were seen were varicella- zoster infection, vasculitis, pityriasis rosea, urticaria. Psoriasis, hereditary angioedema and urticaria flared up during COVID-19 [3].
The assessment of clinical pattern and severity grading of dermatological emergencies was planned during this COVID-19 pandemic.
Materials and methods
This was an observational study conducted from January 2021 to October 2022 in the Department of Dermatology, Venerology, and Leprosy at a tertiary care centre in South India.
All patients seen in outpatient department, emergency medicine department and referred from other departments for dermatological consultations requiring urgent interventions were included. Patients having factitious complaints or visiting outpatient department, emergency medicine department and referred from other departments for dermatological consultation with casual skin lesions/mucosal lesion which did not require urgent intervention were excluded from the study. Skin injuries occurring due to burns, animal bites or accidents were excluded.
A detailed history and clinical examination of all patients was done and recorded with all demographic details. The patients were assessed according to the onset whether acute or exacerbation of a chronic condition; presence of pruritis, pain was recorded. Whether the lesions were localized or generalized, and the presence of wheal, vesicles, erosions and ulcer was recorded. Involvement of body surface area (BSA) percentage was noted. Following which a clinical pattern was identified according to the above factors [4, 5].
The emergency dermatological conditions were graded based on presence of comorbidities (Table 1) and systemic involvement (Table 2) to assess the severity.
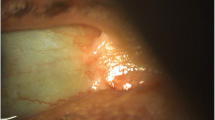
Interesting cases and relapsed cases were documented (Fig. 1).
Interesting dermatological emergencies observed. a Relapsed case of pemphigus vulgaris. b Relapsed case of bullous pemphigoid. c Relapsed case of psoriatic erythroderma. d Acute exacerbation of Psoriasis vulgaris. e Acute onset Leukocytoclastic vasculitis. f Toxic epidermal necrolysis. g Multiple ulcers with secondary infection in Pyoderma gangrenosum. h Oral involvement in Methotrexate toxicity
Result
There was a total of 202 cases enrolled in our study. There were 113 (55.94%) inpatients and 89 (44.05%) outpatients. The age ranged from 5 months to 95 years with majority of the cases belonged to age group 19–64 years (69.8% N = 141). Mean age was 42.85 (SD ± 20.189). Ninety-nine were male and 103 were female.
The most common disease noted was acute urticaria in 51 (24.24%) patients and it was associated with angioedema in 18 patients. This was followed by cutaneous adverse drug reactions (N = 47), vesiculobullous diseases (N = 22), vasculitis (N = 22), infections (N = 18) and erythroderma (N = 16). In pediatric age group, acute urticaria with or without angioedema was most common (N = 12, 48%). In adults drug reactions were most common (N = 35, 24.8%). In geriatric age group vesiculobullous was most common (N = 9, 25%) (Table 3).
In cases of acute urticaria, 21 (41.17%) were of drug induced, 4 (7.84%) of food induced, 3 (5.88%) of hair dye induced, 4 (7.84%) of infection induced, 2 (3.92%) of insect bite and 17 (33.3%) were idiopathic. Due to covid vaccine, 2 cases of acute urticaria and 1 case of leukocytoclastic vasculitis were seen in our study. One patient was suspected of Covid induced sweet’s syndrome. Antibiotics were the category of drug associated with highest frequency of cutaneous adverse drug reaction (N = 16, 23.5%). There were 7 cases due to methotrexate. Multiple drugs were implicated in 12 cases. There were 3 cases due to covid vaccine. Diagnosis of DRESS was confirmed by RegiSCAR criteria for 7 suspected patients. Diagnosis of DRESS was possible in 2 (28.5%) patients, probable in 4 (57.1%) and definite in 1 patient. Out of the 5 cases of TEN, most common score (N = 2) was 3 indicating a 35% mortality. Highest score was 4.
In conditions presenting with erythroderma, both psoriasis and contact dermatitis was seen in 6 (37.5%) patients each, drug induced erythroderma in 3 (18.75%) and 1 (6.25%) was idiopathic. There were 6 patients who got admitted twice during the study period. Three cases were due to erythroderma secondary to psoriasis, contact dermatitis and drug induced each, 1 case of bullous pemphigoid, 1 case of pemphigus vulgaris and 1 case of generalized bullous fixed drug eruption.
On comparing inpatients and outpatients, a higher incidence of acute on chronic onset of lesions (34.5%), pain (41.6%), vesicles (30.1%), erosion (23.9%), ulcer 11 (9.7%) and more than 50% BSA (64.6%) was seen in admitted cases. This was statistically significant. Incidence of wheal (46.1%) was higher in outpatients, which was statistically significant. Generalized lesions (72.6%) and had higher incidence in admitted cases, whereas pruritus’ (78.7%) was more common in outpatients. However, this was not statistically significant. Mucosal involvement was seen in 41.6% patients (Table 4).
On severity grading for comorbidities, most common was grade I (N = 121, 59.9%). Grades II, III and IV were higher in admitted cases. This was statistically significant (p < 0.005) (Table 5).
On severity grading for systemic involvement grade I had the highest number of cases (N = 170, 84.2%). Grades II, III and IV were higher in admitted cases. This was statistically significant (p < 0.005) (Table 6).
On comparing severity grading between comorbidities and systemic involvement, no association was found between the two groups (p = 0.422).
Mortality rate was 1.98% in our study.
Discussion
Dermatological cases are mostly managed on outpatient basis. There are certain conditions such as severe cutaneous adverse drug reactions, immunobullous disorders, angioedema/urticaria, erythroderma, and necrotizing fasciitis which require urgent intervention [5]. Dermatologists face a variety of difficulties in the current scenario, including HIV coinfection, geriatric patients with comorbidities, immunosuppressive medications, and organ transplantation among dermatological patients presenting in an emergency. It presents a fresh set of challenges for clinical care and assessment [6]. The most common age group (19–64 years) was comparable to previous studies [4]. There was slight female preponderance. This contrasted with other studies where male predominance was noted [4, 5, 7].
Acute urticaria with or without angioedema was the commonest, followed by severe cutaneous adverse drug reactions, vesiculobullous diseases and vasculitis. This was similar to study by Modi et al. [4] where 16 different conditions were included among which acute urticaria with or without angioedema was commonest. Acute urticaria with or without angioedema was most common in pediatric age group. In adult age group drug reactions were most common. Whereas vesiculobullous followed by erythroderma were more common in elderly. Drugs were the most common cause of acute urticaria with or without angioedema. We observed psoriasis and contact dermatitis followed by drugs as the common causes for erythroderma.
Antibiotics followed by NSAID were the most common cause of drug reactions. Fixed drug eruption was the most common cause of drug reaction after acute urticaria. This was in contrast to other studies [4,5,6]. People sought consultations from general physicians, pharmacies and online during covid period. They used multiple over the counter drugs which could indicate the higher incidence of fixed drug eruption in our study. Adverse effects due to covid vaccine were an interesting finding in our study.
The higher incidence of methotrexate toxicity seen in seven patients in our series was alarming. Previous studies [4,5,6] on dermatological emergencies have not reported. Our study was done during covid period when self-medication was common, and patients could not come for follow-up due to lockdown restriction guidelines. Few patients were already taking cytotoxic drugs such as methotrexate or were started on it for the first time during Covid period and continued it for long-term basis without consulting their physician. One patient had presumed that taking drug daily would show better response. This indicates the lack of counseling during Covid period.
Six patients got admitted twice during the study period which was an interesting observation in our study however, other similar studies on dermatological emergencies [4,5,6] have not observed it (Table 7). Cesar et al. reported relapse of 27 (26.2%) cases of erythroderma, out of which 18 had psoriasis, 6 had eczema and 3 cases with CTCL. No cases of drug related erythroderma were seen [8]. In a study by Tan et al. relapse rate for erythroderma was reported at 17.8% at 1 year [9].
Six parameters were considered to define the clinical profile of the patients [4, 5]. Inpatients had higher incidence of acute on chronic onset, pain, vesicles, erosion, ulcers and more than 50% BSA involvement. However, acute onset, pruritus, wheals were more common in outpatients. This was similar to study by Samudrala et al. where erosion and ulcer were higher in admitted cases and acute onset was more common in non-admitted cases [5]. BSA > 50% mucosal involvement in our study was comparable to study done by Modi et al. [4].
Dermatological emergencies have been classified as primary and secondary as described by Modi et al. This broadly divides dermatological emergencies having primary cutaneous involvement or secondary to medical/surgical emergencies [4]. However, grading for severity of dermatological emergencies cannot be done. A grading system can help dermatologist’s and allied medical personnel to triage a patient accordingly. This could help plan urgent management required for the patient. In our study assessment/grading of severity in emergency dermatology conditions was done based on comorbidities and systemic manifestations.
Comorbidities were seen in 81 cases which included Diabetes mellitus (12.37%), hypertension (6.43%), diabetes mellitus with hypertension (16.3%), seizure disorder, hypothyroidism, gout, non-Hodgkin’s lymphoma. The presence of comorbidities increases the severity of dermatological emergency. Early examination, identification, and assessment of comorbidities by doing baseline investigation and interventions by other specialties helps us to diagnose and manage the comorbidity accordingly. Systemic involvement included gastro-hepatic, respiratory, renal, and cardiovascular system. There was significant association between systemic involvement and admitted cases. The data reflect that severity of systemic involvement increases the likelihood of admissions. To minimize systemic involvement, a detailed systemic examination and investigations is important to identify and prevent further progression of the disease.
The most common was Grade I in both the groups where there was no comorbidity and systemic involvement. There was also no association between the grading of comorbidities and systemic manifestations. Grade IV systemic involvement only indicates increased risk of mortality. We were able to evaluate the various comorbidities and systems involved in our study, however complete investigation and long-term follow-up with larger population is needed.
The four mortality cases included were pemphigus vulgaris, necrotizing fasciitis, microvascular occlusion syndrome and cellulitis with fixed drug eruption. All the cases had multiorgan failure with grade IV systemic involvement. These cases had long-term systemic involvement and presented late to us. This has not been commented on by previous similar studies [4,5,6].
Ambiguity in determining the dermatological emergencies. Severity grading was done only at baseline visit. Baseline investigations were not done in some of the patients.
Onset, symptom, distribution, cutaneous presentation, BSA and mucosal involvement are the clinical variables that can be used to determine the clinical profile of patients presenting with dermatological emergencies. The proposed severity grading of dermatological emergencies can help triage patients and plan urgent interventions.
Data Availability
The data that support the findings of this study are available from the corresponding author upon request. To maintain patient confidentiality, it has not been made accesible to the public.
References
Jack AR, Spence AA, Nichols BJ, Chong S, Williams DT, Swadron SP, Peng DH (2011) Cutaneous conditions leading to dermatology consultations in the emergency department. West J Emerg Med 12(4):551–555. https://doi.org/10.5811/westjem.2010.4.1653
Ozer I, Ataseven A, Temiz SA (2020) Dermatologic emergencies. Selcuk Tip Derg. 2:157–167. https://doi.org/10.30733/std.2020.01115
Falodun O, Ogunbiyi A (2010) Dermatological emergencies: current trends in management. Ann Ibadan Postgrad Med. https://doi.org/10.4314/AIPM.V4I2.55216
Modi KR, Patel NM, Solanki A, Barot J (2018) Evaluation of emergency dermatological conditions: a prospective study. Indian J Emerg Med 4:147–154. https://doi.org/10.21088/ijem.2395.311X.4318.6
Samudrala S, Dandakeri S, Bhat RM (2018) Clinical profile of dermatological emergencies and intensive care unit admissions in a tertiary care center—an Indian perspective. Int J Dermatol 57(5):575–579. https://doi.org/10.1111/ijd.13957
Mitra D, Chopra A, Saraswat N, Agarwal R, Kumar S (2019) An observational study to describe the clinical pattern of dermatological emergencies from emergency department and intensive care unit: our experience from a tertiary care hospital in Northern India. Indian Dermatol Online J 10(2):144–148. https://doi.org/10.4103/idoj.IDOJ_318_18
Arabi YE, Hali F, Skali HD, Chiheb S (2022) Dermatological emergencies: a Moroccan retrospective case series over a period of two years. Pan Afr Med J 41:348. https://doi.org/10.11604/pamj.2022.41.348.28801
César A, Cruz M, Mota A, Azevedo F (2016) Erythroderma. A clinical and etiological study of 103 patients. J Dermatol Case Rep 10(1):1–9. https://doi.org/10.3315/jdcr.2016.1222
Tan GF, Kong YL, Tan AS, Tey HL (2014) Causes and features of erythroderma. Ann Acad Med Singap 43(8):391–394
Acknowledgements
We are thankful to Dr. Lancy D’souza, Reader in Psychology, Maharaja’s College, University of Mysore, Karnataka for the statistical analysis of the data. We acknowledge JSS Academy of Higher Education (JSS AHER) for their constant academic encouragement and constructive suggestions in completing this project.
Funding
Nil.
Author information
Authors and Affiliations
Contributions
Concept and design of work done by Dr. Kanthraj GR and Dr. Ranugha PSS. Drafting of work, acquisition and interpretation of data done by Dr. Anushka Kedia and Dr. Chethana SG. Revision of content done by Dr. Kanthraj GR and Dr. Ranugha PSS. All authors reviewed the manuscript and approved it.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The author(s) declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kedia, A., Ranugha, P.S.S., Chethana, G.S. et al. Severity grading of dermatological emergencies based on comorbidities and systemic involvement: An observational study. Arch Dermatol Res 315, 2333–2338 (2023). https://doi.org/10.1007/s00403-023-02615-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-023-02615-4