Abstract
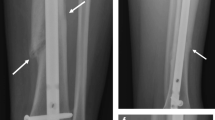
The present study was undertaken to assess the effects of the rigidity of nails on the healing of fractures as evaluated by mechanical strength and rate of bone mineralisation. Ten rats supplied biomechanical data at the start of the experiment and another 100 rats were randomly assigned to 5 groups. In 20 rats no intervention was performed, and they served as a reference group of normal values. Thus, 80 rats underwent a standardised partial osteotomy in the left femur diaphysis prior to manual fracture, reaming and intramedullary nailing. One group received rigid steel nails (group 1) and another, cannulated steel nails (group 2). Group 3 received semi-rigid titanium nails and group 4, soft polyethylene nails. Ten rats in each group were evaluated at 6 and 12 weeks after fracture, and radiographs and callus diameter measurements were performed. Dual-energy X-ray absorptiometry (DEXA) of the bones was performed, and the degree of mineralisation in the callus segment, distal diaphysis and total femur was calculated by the scanner. Subsequently, the bones were tested mechanically by a three-point bending test in a Mini Bionix (MTS) testing system. Radiographs revealed clearly visible fractures at 6 weeks in the intervention groups. At 12 weeks there were no signs of bridging callus in group 4, while the other groups presented scarcely visible osteotomies. The callus area in group 4 was significantly larger at both 6 and 12 weeks than in groups 1–3. In these groups there was a significant decrease in callus area between 6 and 12 weeks. Both maximum bending load, bending rigidity and fracture energy increased significantly in groups 1–3 between 6 and 12 weeks, while bending load and fracture energy increased in group 4. At 6 weeks no significant differences were detected between groups 1–3 in mechanical strength. Group 4 had a significantly reduced maximum bending load and fracture energy at 6 and 12 weeks as well as bending rigidity at 12 weeks. At 12 weeks group 3 had a significantly increased maximum bending load and fracture energy compared with groups 1 and 2. Bone mineral count (BMC) in the callus region in group 4 was significantly reduced at both 6 and 12 weeks. BMC in the callus showed no significant differences between groups 1–3, either at 6 or at 12 weeks. BMC in the distal diaphysis was significantly reduced in groups 1 and 4 compared with group 2 at 12 weeks. Bone mineral density (BMD) in the callus region revealed no significant differences between groups 1–3 at 6 weeks, while at 12 weeks BMD was higher in group 3 than in group 1. BMD in the callus region and total femur in group 4 was significantly reduced at 6 weeks. This study demonstrates that diaphyseal fractures treated with titanium nails with a bending rigidity similar to the intact femur have a higher maximum bending load and fracture energy at 12 weeks than both rigidly or softly nailed fractures. BMD in the callus region was also highest after titanium nailing at 12 weeks. BMD in the distal diaphysis and total femur indicates that the degree of stiffness of the nails have little influence on total bone mineralisation at 12 weeks.
Similar content being viewed by others
Author information
Authors and Affiliations
Additional information
Received: 29 December 1997
Rights and permissions
About this article
Cite this article
Utvåg, S., Reikerås, O. Effects of nail rigidity on fracture healing . Arch Orth Traum Surg 118, 7–13 (1998). https://doi.org/10.1007/s004020050301
Issue Date:
DOI: https://doi.org/10.1007/s004020050301