Abstract
Introduction
Periprosthetic fractures in total hip arthroplasty (THA) have been well described and studied. However, there is a lack of reports on ipsilateral pubic ramus fractures during THA due to the rare occurrence of such fractures and ambiguity of symptoms. With the use of postoperative computed tomography (CT) examinations, we have identified that asymptomatic ipsilateral pubic ramus fractures occur frequently during THA. This study aims to evaluate the incidence, location, clinical outcomes, and risk factors of ipsilateral pubic ramus fractures during THA.
Methods
From May 2022 to March 2023, a single surgeon performed 203 THAs in 183 patients at a single institution. All patients underwent postoperative CT scans three days after THA. The patients with ipsilateral pubic ramus fractures were followed up for a minimum of six months. Basic demographics, osteoporosis, general conditions of the operations, and outcomes of THA were investigated in all patients.
Results
Twenty-two cases (10.8%) of ipsilateral pubic ramus fractures were identified on postoperative CT scans. All fractures were located near the origin of the superior or inferior pubic ramus. Five fractures were detected on simple postoperative radiographs. The fractures did not cause any further complications at a minimum of six-month postoperative follow-up. Univariate and multivariate analyses did not identify any risk factors associated with these fractures.
Conclusions
Although the incidence of ipsilateral pubic ramus fractures during THA is high, treatment is not required as they do not cause any significant clinical symptoms or affect the prognosis of THA. However, the possibility of occurrence of these fractures must be explained to the patients before surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Currently, cementless acetabular components are commonly employed in total hip arthroplasty (THA) procedures, utilizing the under-reaming technique and press-fit impaction [23]. Press-fit impaction of the acetabular component with or without screw fixation has become the most widely used fixation technique [8]. However, during impaction, a periprosthetic pelvic fracture can occur. Fortunately, it has been rarely reported [9]. Simple radiographs alone may not be sufficient to detect a periprosthetic fracture of the pelvis immediately after its occurrence; other modalities, such as computed tomography (CT) or magnetic resonance imaging (MRI), are usually required to confirm the fracture.
As part of another study protocol that obtained postoperative CT images in consecutive primary THAs, we identified postoperative ramus fractures and found that the incidence of these fractures was unexpectedly high.
Previously, the following risk factors for perioperative periprosthetic fractures around the acetabulum were studied: under-reaming or oversizing of the cup, osteoporosis, and a preoperative diagnosis of rheumatoid arthritis [2, 5, 6, 12, 15, 16, 26]. However, little is known about the incidence, risk factors, and outcomes following periprosthetic ramus occult fractures.
Therefore, we aimed to assess (1) the prevalence of occult fractures of the ipsilateral ramus during primary THA, (2) location of these fractures, (3) radiologic and clinical outcomes, and (4) risk factors contributing to these fractures.
Methods
This was a case series study with retrospective review of the medical records upon approval of the Institutional Review Board of our hospital (IRB no.: H-2302-040-1402). The requirement for obtaining informed consent was waived due to the retrospective nature of the study.
Participants
Between May 2022 and March 2023, all 189 patients undergoing 209 primary cementless THAs at our institution were included in the study and they underwent CT scans three days after the index surgery. THAs performed during this time were not excluded from this imaging protocol. Exclusion criteria for patients in this study were prior history of pelvic osteotomy, pelvic trauma, previous joint infection, and usage of the automated surgical impactor. Six patients, in whom an automated surgical impactor was used, were excluded in order to control for variables and reduce bias. A total of 183 individuals with 203 hips were included.
A total of 183 participants (126 females and 57 males), with an average age of 55.5 ± 15.0 years (range, 16–83 years) participated in this study. Their average body mass index (BMI) was 25.4 ± 4.2 Kg/m2 (range, 17.7–37.4 kg/m2).
Preoperative diagnoses included osteonecrosis of the femoral head in 96 hips, primary osteoarthritis or arthritis due to dysplastic hip in 84 hips, sequelae of Perthes’ disease in 12 hips, inflammatory arthritis in 8 hips, and other in 3 hips (Table 1).
Dual-energy X-ray absorptiometry (DXA) was routinely performed in individuals over the age of 50 years.
Operation
A single hip arthroplasty surgeon (JJY) with more than 20 years of experience in a tertiary referral hospital performed all index operations. The surgical procedure for THA was carried out in the lateral decubitus position using the modified direct lateral approach [20]. The patient secured to the table using the lateral hip positioner (Online resource 1) [19]. True hemispheric acetabular component designs were used, such the Bencox Mirabo cup (Corentec, Cheonan, Korea) and G7® (Zimmer Biomet, Warsaw, IN, USA). After under-reaming the acetabulum by 1 mm, the hemispheric cups were inserted using the press-fit technique.
Impaction of the acetabular component was performed two or three times with a surgical mallet (1.8 kg) swung by gripping its neck. Depending on the rigidity of the press-fit, two dome screws or no dome screws were inserted.
The angle of the acetabular cup was set to achieve an inclination of 30–45° and an anteversion of 15–25° [3].
We performed routine total hip arthroplasty without any additional procedures, such as internal fixation of fractures, for all participants.
Postoperative CT scan
We differentiated occult fractures from periprosthetic fractures that were noticed during surgery, and we defined occult fractures as those that were not seen on either intraoperative findings or intraoperative radiographs but could only be checked on the postoperative 3D CT images of the pelvis. Based on where the fractures had occurred, we divided the location of fractures into the following five groups: superior pubic ramus, inferior pubic ramus, both rami, the periacetabulum, and pubic symphyseal area (Fig. 1). We identified the periacetabulum-to-rami boundary as the lateral margin of the obturator foramen. The pubic symphyseal region and rami were defined as being separated by the medial edge.
Functional recovery
Regardless of the fracture, partial weight-bearing with a crutch gait or a walker was recommended for the first 6 weeks after surgery. Subsequently, full weight-bearing was allowed as tolerated. Patients were followed up for 6 weeks, 6 months, 12 months, and then annually after the surgery.
Radiologic outcome and functional outcome
Radiographic evaluations were performed by two independent fellowship-trained orthopedic surgeons who did not participate in the initial arthroplasties (HSK and YSK). In addition to the postoperative CT scans, anteroposterior and cross-table lateral radiographs were obtained at each follow-up, along with the inlet, outlet, and oblique views of the pelvis. Acetabular components were considered loose if there was a change in the alignment by 4° or more or 4 mm [13].
Clinical evaluation was conducted using the modified Harris Hip score (worst score 0, best score 100) [4].
Statistical analysis
Statistical analysis in this study involved comparing continuous variables using the t-test or Mann-Whitney U test and comparing dichotomous variables using the chi-square test or Fisher exact test. Additionally, multivariate logistic regression analysis was used. A significance level of p < 0.05 was used to determine statistical significance. Statistical analyses were performed using IBM SPSS Statistics for Windows, version 25.0 (IBM Corp., Armonk, NY, USA).
Results
Incidence of fractures
Periprosthetic fractures of the acetabulum were not detected during surgery. In postoperative CT scans, the ipsilateral ramus fracture was found in 22 hips (10.8%). All contralateral rami were intact. Before identifying ramus fractures that occurred during THA, there were 12 cases of ramus fractures among 90 THAs. Following awareness of this issue and formulation of this study, 10 fractures were identified in 113 hips. Despite being aware of the possibility of occurrence of ramus fracture, there was no statistically significant difference in the fracture incidence.
Location of fractures
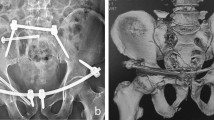
Occult fractures were most frequently found in the superior pubic ramus, accounting for 10 out of 22 hips (45.4%) (Figs. 2 and 3). Fractures of the inferior pubic ramus were observed in 9 hips (40.9%) (Fig. 4), while 1 hip (4.5%) exhibited fractures in both pubic rami. Fractures involving the peri-acetabulum were observed in 2 hips (9.0%), with one hip showing an extension of the fracture into the superior pubic ramus and the other hip showing extension of the fracture into the inferior pubic ramus. No fractures were observed in the pubic symphyseal area (Table 1).
Radiographs showing superior pubic ramus fracture during total hip arthroplasty. (A) Preoperative anteroposterior view. (B) No fracture lines are visible on the postoperative hip anteroposterior radiograph. (C) Magnified view. (D) The postoperative hip computed tomography coronal view shows incomplete fracture lines (arrow) on the left superior pubic ramus
Radiographs showing superior pubic ramus fracture during total hip arthroplasty. (A) Preoperative anteroposterior view. (B) incomplete fracture lines on the left superior pubic ramus are visible on the postoperative hip anteroposterior radiograph. (C) Magnified view. (D) The postoperative hip computed tomography coronal view shows an incomplete fracture line on the left superior pubic ramus
Radiographs showing an inferior pubic ramus fracture during total hip arthroplasty. (A) Preoperative anteroposterior view. (B) Fragmented fractures (arrow) on the right inferior pubic ramus are visible on the postoperative hip anteroposterior radiograph. (C) Magnified view. (D) The postoperative hip computed tomography axial view reveals comminuted fractures on the right inferior pubic ramus
Radiological outcome and clinical outcome
In hips with ramus fractures, the average cup inclination was 34.3°± 4.0° and anteversion was 26.3°±11.3°. On the other hand, cup inclination was 33.9°±4.8° and anteversion was 25.1°±9.5° on average in hips without any fractures with a p-value of 0.775 and 0.590, respectively.
All acetabular cups demonstrated stability with no discernible evidence of cup migration or loosening. Simple radiographs obtained after six months from the index surgery showed no evidence of further displacement or apparent fracture line.
The mean preoperative modified Harris hip score of 51.8 points (range, 47-84 points) improved to 94.6 points (range, 85-100 points) at the time of the postoperative 6-month follow-up in the non-fracture group: 53.1 points (range, 45-70 points) to 93.7 points (range, 82-100 points). Throughout the entire follow-up period, including the immediate postoperative period and up to 6 weeks postoperatively, none of the patients reported abnormal inguinal pain or tenderness. None of the patients required walking support after 6 weeks postoperatively.
Risk factors
After controlling for potentially relevant confounding variables, including sex, age, BMI, size of each cup, cup position, cup design, manufacturer of the implants, or presence of osteoporosis, no identifiable risk factors were found to be associated with an increased risk of occult periprosthetic fracture in the multivariate logistic regression analysis.
Discussion
Periprosthetic acetabular fracture during primary THA is a rare but reported complication. To the best of the author’s knowledge, this is the first report investigating the prevalence and outcomes of ramus fracture during THA. We observed pubic ramus fractures in 22 of 203 primary hips (10.8%) and the fracture occurred on the superior and inferior pubic rami and periacetabular area. None of the patients reported additional pain or tenderness during the entire follow-up period, and all patients achieved bony union. Risk factors associated with periprosthetic rami fractures were not identified.
Femoral fractures have been extensively studied and documented [1, 10, 25]; however, there is a dearth of reports and studies on periprosthetic acetabular fractures. It is challenging to detect fractures of the ramus and acetabulum during THA on plain radiographs due to the complicated morphology of the pelvic bone, its cancellous nature, and broad soft tissue coverage. Hasegawa et al. studied periprosthetic occult fractures around the acetabulum after primary THA and reported 8.4% of occult fractures using perioperative CT scans [11]. In our study, we utilized postoperative CT scans to detect not only occult periacetabular fractures but also fractures in the rami. Fractures in rami were more prevalent than those in the periacetabular area. We postulated that the impulsive force of cup impaction in the superior, medial, and posterior directions transforms into compressive and shear stresses on the rami, which lead to fractures at the weak point of the rami (Fig. 5). The rate of ipsilateral ramus fracture was unexpectedly high. Although surgeries were only conducted by an experienced surgeon who performed more than 200 THA procedures per year, a significant prevalence was identified. There was no statistically significant difference in the prevalence of surgery before and after identifying and attending to the fracture.
In our study, all patients achieved bone ingrowth fixation, and no additional surgical interventions were necessary during the follow-up. All patients were able to ambulate without the assistance of a walking aid. However, it should be noted that postoperative pain following THA may mask any bony pain associated with the periprosthetic ramus fracture. Nonetheless, routine 6-week protective weight-bearing measures and postoperative pain management may be sufficient for adequate bony union of these fractures. Hasegawa et al. have similarly reported that periprosthetic occult fractures of the acetabulum did not require further intervention [11]. Thus, even in the event of perioperative detection of a ramus fracture, patients can be reassured that further intervention may not be necessary [7, 24]. Even if these fractures do not require any special care, the surgeon should be aware that they can occur during THA. Medical disputes or lawsuits may arise if surgeons fail to adequately inform their patients. Before the operation, the surgeon must inform the patient that ramus fractures might occur and educate them that additional care is seldom needed.
On the other hand, delayed periacetabular fractures require a different approach as they result from osteolysis around the acetabular component, which may take some time to develop after primary surgery [21]. Stress fractures of the pubic ramus have been reported in the literature as a complication following THA, which could be successfully managed with protective weight bearing. However, acute fractures due to a fall may require more attention. Radha et al. reported a case of a pubic ramus fracture that occurred seven months after index surgery, leading to instability of the acetabular component. In this case, the instability of the well-fixed acetabular component occurred due to the fact that the pubic ramus fracture extended to the acetabulum, which was not initially detected [21]. However, occult fractures during primary THA did not affect the fixation of the cup in short term observation.
Our findings indicate that bone quality, evaluated by dual-energy X-ray absorptiometry, was not correlated with the occurrence of intraoperative ramus fractures. Osteoporosis was diagnosed in 31.6% of the hips in the fracture group, while 24.0% of the hips in the non-fracture group were diagnosed with osteoporosis. The association between osteoporosis and intraoperative fracture is controversial. Some studies have suggested that sclerotic unyielding under-reamed acetabulum with good bone quality may be a reason for the fracture [22], while others have mentioned that osteoporosis may be a predisposing factor [11]. In our study, no risk factor was identified in the multivariate logistic regression analysis.
The design of the acetabular component may influence the prevalence of occult ramus fractures. Hasegawa et al. reported that among the other possible risk factors, only the use of a peripheral self-locking cup was associated with an increased risk of fractures [11]. In our study, only a hemispherical cup was used. The incidence of fractures may increase when the other types of designs are utilized. The size and position of the acetabular component were not associated with an increased risk of fractures.
We hypothesized that the patient’s position, either lateral decubitus or supine, and the surgical approach, anterolateral, direct lateral, or posterolateral, may affect the occurrence of ramus fracture. Due to the rarity of this fracture, none of the studies have shown an association between the patient’s position and occurrence of the fracture. Most studies reporting on periprosthetic intraoperative fractures were performed using the posterolateral approach with the patient in the lateral decubitus position [11, 14]. In our study, all index surgeries were performed using the direct lateral approach with the patient in the lateral decubitus position. We assumed that the prevalence of ramus fractures would differ among other surgical approaches, such as direct anterior approach with the patient in the supine position due the counter effect of the operating bed against the impaction force [18]. A future systematic review or meta-analysis is warranted.
Moreover, the influence of the surgeon’s impaction force on the prevalence of ramus fractures was also acknowledged in our study. The minimum impaction force required for a press-fit of an acetabular component in primary THA can vary based on several factors, including the size and design of the implant, the quality and thickness of the bone, and the surgical technique used [17]. A sufficient but not overwhelming impaction force should be applied to achieve stable fixation of the implant without causing any damage to the bone or deformation of the implant. It may be possible to avoid iatrogenic fractures by using an automated surgical impactor, but further research is necessary to pinpoint its potential applications.
We acknowledge several limitations of our study. First, this study was a retrospective review, although patients were enrolled longitudinally. Future large-scale, prospective, multi-center cohorts are needed to confirm our findings. Second, our study was conducted in an East Asian country, therefore the proportion of diagnoses requiring total hip arthroplasty may differ from that in Western countries. Additionallythe mean BMI was 25.4 ± 4.2 Kg/m2. Although there was no significant difference in the proportion of diagnosises, the height or BMI between the two groups, our findings could not be generalized to Western countries. Third, there could be the potential of selection bias since all the index surgeries were performed by a single surgeon. However, the surgeon was fellowship-trained hip arthroplasty surgeon who conducted more than 300 total hip arthroplasty procedures annually in tertiary referral hospital.Lastly, the hip positioner might affect the fracture incidence. Mittal et al. reported that there was difference in pelvic stability among different hip positioners. Though this study provides laboratory data, its relevance to actual clinical practice remains uncertain. Nevertheless, the hip positioner utilized in this study is a commonly employed standard positioner, thus it can be regarded as representative of typical condition.
Conclusion
The incidence in this study of ipsilateral ramus fracture during THA was 10.8%. Notwithstanding the fact that the incidence rate was higher than expected, such fractures generally do not cause significant clinical symptoms. Therefore, treatment is not required. Surgeons should be aware of the high occurrence of these fractures and should educate and reassure their patients about the risk of these fractures prior to surgery.
References
Abdel MP, Houdek MT, Watts CD, Lewallen DG, Berry DJ (2016) Epidemiology of periprosthetic femoral fractures in 5417 revision total hip arthroplasties: a 40-year experience. Bone Joint J 98–B(4):468–474
Aslam-Pervez N, Riaz O, Gopal S, Hossain F (2018) Predictors of Intraoperative Fractures during Hemiarthroplasty for the treatment of fragility hip fractures. Clin Orthop Surg 10(1):14–19
Barrack RL, Krempec JA, Clohisy JC et al (2013) Accuracy of acetabular component position in hip arthroplasty. J Bone Joint Surg Am 95(19):1760–1768
Byrd JW, Jones KS (2000) Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy 16(6):578–587
Chitre A, Wynn Jones H, Shah N, Clayson A (2013) Complications of total hip arthroplasty: periprosthetic fractures of the acetabulum. Curr Rev Musculoskelet Med 6(4):357–363
Curtis MJ, Jinnah RH, Wilson VD, Hungerford DS (1992) The initial stability of uncemented acetabular components. J Bone Joint Surg Br 74(3):372–376
Dammerer D, Putzer D, Glodny B et al (2019) Occult intra-operative periprosthetic fractures of the acetabulum may affect implant survival. Int Orthop 43(7):1583–1590
Garcia-Rey E, Garcia-Cimbrelo E, Cruz-Pardos A (2012) Cup press fit in uncemented THA depends on sex, acetabular shape, and surgical technique. Clin Orthop Relat Res 470(11):3014–3023
Haidukewych GJ, Jacofsky DJ, Hanssen AD, Lewallen DG (2006) Intraoperative fractures of the acetabulum during primary total hip arthroplasty. J Bone Joint Surg Am 88(9):1952–1956
Han KS, Kang SR, Yoon SJ (2023) Does the Periprosthetic fracture pattern depend on the stem fixation method in total hip arthroplasty? Clin Orthop Surg 15(1):42–49
Hasegawa K, Kabata T, Kajino Y, Inoue D, Tsuchiya H (2017) Periprosthetic Occult fractures of the Acetabulum Occur frequently during primary THA. Clin Orthop Relat Res 475(2):484–494
Inoue D, Kabata T, Maeda T et al (2015) Usefullness of three-dimensional templating software to quantify the contact state between implant and femur in total hip arthroplasty. Eur J Orthop Surg Traumatol 25(8):1293–1300
Latimer HA, Lachiewicz PF (1996) Porous-coated acetabular components with screw fixation. Five to ten-year results. J Bone Joint Surg Am 78(7):975–981
Li J, Ji Q, Ni M, Zheng Q, Sun J, Zhang G (2020) Management of intraoperative acetabular fracture in primary total hip arthroplasty. BMC Musculoskelet Disord 21(1):383
MacKenzie JR, Callaghan JJ, Pedersen DR, Brown TD (1994) Areas of contact and extent of gaps with implantation of oversized acetabular components in total hip arthroplasty. Clin Orthop Relat Res (298):127–136
Malhotra R, Gupta S, Gupta V, Manhas V (2022) Risk factors and outcomes Associated with Intraoperative Fractures during short-stem total hip arthroplasty for osteonecrosis of the femoral head. Clin Orthop Surg 14(1):41–47
Messer-Hannemann P, Campbell GM, Morlock MM (2019) Deformation of acetabular press-fit cups: influence of design and surgical factors. Clin Biomech (Bristol Avon) 69:96–103
Metzger CM, Farooq H, Hur JO, Hur J (2022) Transitioning from the posterior Approach to the Direct Anterior Approach for Total Hip Arthroplasty. Hip Pelvis 34(4):203–210
Mittal A, Chetty N, Pham T et al (2022) Pelvic stability during simulated total hip arthroplasty motions: comparing different hip positioners. J Orthop 34:398–403
Mulliken BD, Rorabeck CH, Bourne RB, Nayak N (1995) The surgical approach to total hip arthroplasty: complications and utility of a modified direct lateral approach. Iowa Orthop J 15:48–61
Radha S, Shenouda M, Hazlerigg A, Konan S, Hulme A (2013) Fractured inferior pubic ramus with ipsilateral total hip replacement: a case report and review of the literature. Case Rep Orthop, 2013:674732
Sharkey PF, Hozack WJ, Callaghan JJ et al (1999) Acetabular fracture associated with cementless acetabular component insertion: a report of 13 cases. J Arthroplasty 14(4):426–431
Toossi N, Adeli B, Timperley AJ, Haddad FS, Maltenfort M, Parvizi J (2013) Acetabular components in total hip arthroplasty: is there evidence that cementless fixation is better? J Bone Joint Surg Am 95(2):168–174
Yamamuro Y, Kabata T, Kajino Y, Inoue D, Hasegawa K, Tsuchiya H (2022) Does intraoperative periprosthetic occult fracture of the acetabulum affect clinical outcomes after primary total hip arthroplasty? Arch Orthop Trauma Surg 142(11):3497–3504
Yun HH, Lee WS, Shin YB, Yoon TH (2023) Periprosthetic Occult femoral fracture: an unknown side effect of press-fit fixation in primary Cementless Total Hip Arthroplasty. Hip Pelvis 35(2):88–98
Zwartele RE, Witjes S, Doets HC, Stijnen T, Poll RG (2012) Cementless total hip arthroplasty in rheumatoid arthritis: a systematic review of the literature. Arch Orthop Trauma Surg 132(4):535–546
Funding
Open Access funding enabled and organized by Seoul National University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The design and protocol of this prospective study were approved by the institutional review board at the authors’ hospital (H-2302-040-1402).
Conflict of interest
Authors report no financial interest in or arrangement with a company whose product was used in a study or is referred to in this article. There was no financial interest in or arrangement with a competing company, or any other financial connections that might raise the question of bias in the work reported.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was performed in Seoul National University Hospital.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ko, YS., Lee, H.J., Kim, H.S. et al. Ipsilateral pubic ramus fracture during total hip arthroplasty is not rare: does it matter?. Arch Orthop Trauma Surg (2024). https://doi.org/10.1007/s00402-024-05368-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00402-024-05368-5