Abstract
Introduction
There is an increasing interest in the use of intra-articular (IA) antibiotic infusion as a stand-alone or adjuvant therapy to standard revision surgery for periprosthetic joint infection (PJI). The objective of this systematic review is to evaluate the evidence with respect to this up-and-coming treatment modality.
Methods
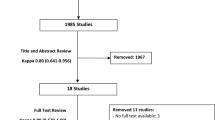
A systematic review of studies published until April 2023 was conducted using PubMed, Embase, MEDLINE and Cochrane databases. Quality assessment was performed with the National Institute of Health quality assessment tool. Inclusion criteria were adult patients (≥ 18 years) with a mean follow-up of ≥ 11 months and a score ≥ 6 on the National Institute of Health quality assessment tool. Primary outcome was eradication of infection.
Results
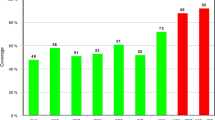
15 articles, encompassing 631 PJIs in 626 patients, were included in the final analysis, all level IV case series. The majority was treated with single-stage revision with adjuvant IA antibiotic infusion (79.1%). The remaining PJIs were treated with stand-alone IA antibiotic infusion (12.2%), DAIR (debridement, antibiotics and implant retention) with adjuvant IA antibiotic infusion (5.7%) or two-stage revision with adjuvant IA antibiotic infusion (3.0%). Mean duration of IA antibiotic infusion was 19 days (range 3–50). An overall failure rate of approximately 11% was found. In total 117 complications occurred, 71 were non-catheter-related and 46 were catheter-related. The most common catheter-related complications were premature loss of the catheter (18/46) and elevated blood urea nitrogen (BUN) and creatinine levels (12/46).
Conclusions
Due to the lack of comparative studies the (added) benefit of IA antibiotic infusion in the treatment of PJI remains uncertain. Based on the current evidence, we would advise against using it as a stand-alone treatment. A prospective randomized controlled trial using a well-described infusion protocol is needed to see if the potential benefits justify the increased costs and potential complications of this treatment modality.


Similar content being viewed by others
References
Bourget-Murray J, Azad M, Gofton W, Abdelbary H, Garceau S, Grammatopoulos G (2023) Is the routine use of local antibiotics in the management of periprosthetic joint infections justified? Hip Int J Clin Exp Res Hip Pathol Therapy 33(1):4–16. https://doi.org/10.1177/11207000221139467
Steadman W, Chapman PR, Schuetz M, Schmutz B, Trampuz A, Tetsworth K (2023) Local antibiotic delivery options in prosthetic joint infection. Antibiot (Basel, Switzerl) 12(4):752. https://doi.org/10.3390/antibiotics12040752
Nelson CL, Evans RP, Blaha JD, Calhoun J, Henry SL, Patzakis MJ (1993) A comparison of gentamicin-impregnated polymethylmethacrylate bead implantation to conventional parenteral antibiotic therapy in infected total hip and knee arthroplasty. Clin Orthop Relat Res 295:96–101
Stockley I, Mockford BJ, Hoad-Reddick A, Norman P (2008) The use of two-stage exchange arthroplasty with depot antibiotics in the absence of long-term antibiotic therapy in infected total hip replacement. J Bone Joint Surg Br 90(2):145–148. https://doi.org/10.1302/0301-620X.90B2.19855
Hart WJ, Jones RS (2006) Two-stage revision of infected total knee replacements using articulating cement spacers and short-term antibiotic therapy. J Bone Joint Surg Br 88(8):1011–1015. https://doi.org/10.1302/0301-620X.88B8.17445
Abosala A, Ali M (2020) The Use of calcium sulphate beads in periprosthetic joint infection, a systematic review. J Bone Joint Infect 5(1):43–49. https://doi.org/10.7150/jbji.41743
Howlin RP, Brayford MJ, Webb JS, Cooper JJ, Aiken SS, Stoodley P (2015) Antibiotic-loaded synthetic calcium sulfate beads for prevention of bacterial colonization and biofilm formation in periprosthetic infections. Antimicrob Agents Chemother 59(1):111–120. https://doi.org/10.1128/AAC.03676-14
Reinisch K, Schläppi M, Meier C, Wahl P (2022) Local antibiotic treatment with calcium sulfate as carrier material improves the outcome of debridement, antibiotics, and implant retention procedures for periprosthetic joint infections after hip arthroplasty—a retrospective study. J Bone Joint Infection 7(1):11–21. https://doi.org/10.5194/jbji-7-11-2022
Anguita-Alonso P, Rouse MS, Piper KE, Jacofsky DJ, Osmon DR, Patel R (2006) Comparative study of antimicrobial release kinetics from polymethylmethacrylate. Clin Orthop Relat Res 445:239–244. https://doi.org/10.1097/01.blo.0000201167.90313.40
McLaren RL, McLaren AC, Vernon BL (2008) Generic tobramycin elutes from bone cement faster than proprietary tobramycin. Clin Orthop Relat Res 466(6):1372–1376. https://doi.org/10.1007/s11999-008-0199-2
Schwarz EM, McLaren AC, Sculco TP, Brause B, Bostrom M, Kates SL, Parvizi J, Alt V, Arnold WV, Carli A, Chen AF, Choe H, Coraça-Huber DC, Cross M, Ghert M, Hickok N, Jennings JA, Joshi M, Metsemakers WJ, Ninomiya M (2021) Adjuvant antibiotic-loaded bone cement: concerns with current use and research to make it work. J Orthopaedic Res 39(2):227–239. https://doi.org/10.1002/jor.24616
van de Belt H, Neut D, Uges DR, Schenk W, van Horn JR, van der Mei HC, Busscher HJ (2000) Surface roughness, porosity and wettability of gentamicin-loaded bone cements and their antibiotic release. Biomaterials 21(19):1981–1987. https://doi.org/10.1016/s0142-9612(00)00082-x
van de Belt H, Neut D, Schenk W, van Horn JR, van der Mei HC, Busscher HJ (2000) Gentamicin release from polymethylmethacrylate bone cements and Staphylococcus aureus biofilm formation. Acta Orthop Scand 71(6):625–629. https://doi.org/10.1080/000164700317362280
Samuel S, Mathew BS, Veeraraghavan B, Fleming DH, Chittaranjan SB, Prakash JA (2012) In vitro study of elution kinetics and bio-activity of meropenem-loaded acrylic bone cement. J Orthopaed Traumatol 13(3):131–136. https://doi.org/10.1007/s10195-012-0191-1
Gasparini G, De Gori M, Calonego G, Della Bora T, Caroleo B, Galasso O (2014) Drug elution from high-dose antibiotic-loaded acrylic cement: a comparative, in vitro study. Orthopedics 37(11):e999–e1005. https://doi.org/10.3928/01477447-20141023-57
Johnson JD, Nessler JM, Horazdovsky RD, Vang S, Thomas AJ, Marston SB (2017) Serum and wound vancomycin levels after intrawound administration in primary total joint arthroplasty. J Arthroplasty 32(3):924–928. https://doi.org/10.1016/j.arth.2015.10.015
Tkhilaishvili T, Winkler T, Müller M, Perka C, Trampuz A (2019) Bacteriophages as adjuvant to antibiotics for the treatment of periprosthetic joint infection caused by multidrug-resistant Pseudomonas aeruginosa. Antimicrob Agents Chemother 64(1):e00924-e1019. https://doi.org/10.1128/AAC.00924-19
Ferry T, Leboucher G, Fevre C, Herry Y, Conrad A, Josse J, Batailler C, Chidiac C, Medina M, Lustig S, Laurent F (2018) Salvage debridement, antibiotics and implant retention (“DAIR”) with local injection of a selected cocktail of bacteriophages: is it an option for an elderly patient with relapsing Staphylococcus aureus Prosthetic-Joint Infection? Open Forum Infect Dis 5(11):269. https://doi.org/10.1093/ofid/ofy269
Ferry T, Batailler C, Souche A, Cassino C, Chidiac C, Perpoint T, le Corvaisier C, Josse J, Gaillard R, Roger J, Kolenda C, Lustig S, Laurent F (2021) Arthroscopic “debridement and implant retention” with local administration of exebacase (Lysin CF-301) followed by suppressive tedizolid as salvage therapy in elderly patients for relapsing multidrug-resistant S. Epidermidis prosthetic knee infection. Front Med 8:550853. https://doi.org/10.3389/fmed.2021.550853
Ferry T, Kolenda C, Batailler C, Gustave CA, Lustig S, Malatray M, Fevre C, Josse J, Petitjean C, Chidiac C, Leboucher G, Laurent F (2020) Phage therapy as adjuvant to conservative surgery and antibiotics to salvage patients with relapsing S. aureus prosthetic knee infection. Front Med 7:570572. https://doi.org/10.3389/fmed.2020.570572
Gibb BP, Hadjiargyrou M (2021) Bacteriophage therapy for bone and joint infections. Bone Joint J 103(2):234–244. https://doi.org/10.1302/0301-620X.103B2.BJJ-2020-0452.R2
Lloyd KC, Stover SM, Pascoe JR, Baggot JD, Kurpershoek C, Hietala S (1988) Plasma and synovial fluid concentrations of gentamicin in horses after intra-articular administration of buffered and unbuffered gentamicin. Am J Vet Res 49(5):644–649
Schneider RK (1988) Treatment of posttraumatic septic arthritis. In: AAEP Proc, vol 44, p 167
Adams SB, Lescun TB (2000) How to treat septic joints with constant intra-articular infusion of gentamicin or amikacin. In: AAEP Proc, vol 46, pp 188–192
Werner LA, Hardy J, Bertone AL (2003) Bone gentamicin concentration after intra-articular injection or regional intravenous perfusion in the horse. Vet Surg 32(6):559–565. https://doi.org/10.1111/j.1532-950x.2003.00559.x
Davenport K, Traina S, Perry C (1991) Treatment of acutely infected arthroplasty with local antibiotics. J Arthroplasty 6(2):179–183. https://doi.org/10.1016/s0883-5403(11)80014-8
Perry CR, Hulsey RE, Mann FA, Miller GA, Pearson RL (1992) Treatment of acutely infected arthroplasties with incision, drainage, and local antibiotics delivered via an implantable pump. Clin Orthop Relat Res 281:216–223
Shaw JA (1995) The use of long-term indwelling catheters for local antibiotic administration into infected joints. J Orthop Tech 3:181–184
Roy ME, Peppers MP, Whiteside LA, Lazear RM (2014) Vancomycin concentration in synovial fluid: direct injection into the knee vs intravenous infusion. J Arthroplasty 29(3):564–568. https://doi.org/10.1016/j.arth.2013.08.017
Zimmerli W, Trampuz A, Ochsner PE (2004) Prosthetic-joint infections. N Engl J Med 351(16):1645–1654. https://doi.org/10.1056/NEJMra040181
Whiteside LA, Peppers M, Nayfeh TA, Roy ME (2011) Methicillin-resistant Staphylococcus aureus in TKA treated with revision and direct intra-articular antibiotic infusion. Clin Orthop Relat Res 469(1):26–33. https://doi.org/10.1007/s11999-010-1313-9
Whiteside LA, Nayfeh TA, LaZear R, Roy ME (2012) Reinfected revised TKA resolves with an aggressive protocol and antibiotic infusion. Clin Orthop Relat Res 470(1):236–243. https://doi.org/10.1007/s11999-011-2087-4
Fukagawa S, Matsuda S, Miura H, Okazaki K, Tashiro Y, Iwamoto Y (2010) High-dose antibiotic infusion for infected knee prosthesis without implant removal. J Orthopaed Sci 15(4):470–476. https://doi.org/10.1007/s00776-010-1487-8
Whiteside LA, Roy ME (2017) One-stage revision with catheter infusion of intraarticular antibiotics successfully treats infected THA. Clin Orthop Relat Res 475(2):419–429. https://doi.org/10.1007/s11999-016-4977-y
Antony SJ, Westbrook RS, Jackson JS, Heydemann JS, Nelson JL (2015) Efficacy of single-stage revision with aggressive debridement using intra-articular antibiotics in the treatment of infected joint prosthesis. Infect Dis 8:17–23. https://doi.org/10.4137/IDRT.S26824
Ji B, Li G, Zhang X, Wang Y, Mu W, Cao L (2020) Effective treatment of single-stage revision using intra-articular antibiotic infusion for culture-negative prosthetic joint infection. Bone Joint J 102(3):336–344. https://doi.org/10.1302/0301-620X.102B3.BJJ-2019-0820.R1
Li Y, Zhang X, Guo X, Wulamu W, Yushan N, Ji B, Cao L (2022) Effective treatment of single-stage revision using intra-articular antibiotic infusion for polymicrobial periprosthetic joint infection. J Arthroplasty 37(1):156–161. https://doi.org/10.1016/j.arth.2021.09.022
Li Y, Zhang X, Ji B, Wulamu W, Yushan N, Guo X, Cao L (2023) One-stage revision using intra-articular carbapenem infusion effectively treats chronic periprosthetic joint infection caused by Gram-negative organisms. Bone Joint J 105(3):284–293. https://doi.org/10.1302/0301-620X.105B3.BJJ-2022-0926.R1
Liu CW, Kuo CL, Chuang SY, Chang JH, Wu CC, Tsai TY, Lin LC (2013) Results of infected total knee arthroplasty treated with arthroscopic debridement and continuous antibiotic irrigation system. Indian J Orthopaed 47(1):93–97. https://doi.org/10.4103/0019-5413.106925
Chaiyakit P, Meknavin S, Hongku N, Onklin I (2021) Debridement, antibiotics, and implant retention combined with direct intra-articular antibiotic infusion in patients with acute hematogenous periprosthetic joint infection of the knee. BMC Musculoskelet Disord 22(1):557. https://doi.org/10.1186/s12891-021-04451-x
Gaillard-Campbell D, Gross TP, Webb L (2021) Antibiotic delivery via hickman catheter for the treatment of prosthetic joint infection. Orthopedics 44(3):e395–e401. https://doi.org/10.3928/01477447-20210414-12
Ji B, Li G, Zhang X, Xu B, Wang Y, Chen Y, Cao L (2022) Effective single-stage revision using intra-articular antibiotic infusion after multiple failed surgery for periprosthetic joint infection : a mean seven years’ follow-up. Bone Joint J 104(7):867–874. https://doi.org/10.1302/0301-620X.104B7.BJJ-2021-1704.R1
Perry CR, Pearson RL (1991) Local antibiotic delivery in the treatment of bone and joint infections. Clin Orthop Relat Res 263:215–226
Tsumura H, Ikeda S, Ono T, Itonaga I, Taira H, Torisu T (2005) Synovectomy, debridement, and continuous irrigation for infected total knee arthroplasty. Int Orthop 29(2):113–116. https://doi.org/10.1007/s00264-004-0626-2
Ji B, Wahafu T, Li G, Zhang X, Wang Y, Momin M, Cao L (2019) Single-stage treatment of chronically infected total hip arthroplasty with cementless reconstruction: results in 126 patients with broad inclusion criteria. Bone Joint J 101(4):396–402. https://doi.org/10.1302/0301-620X.101B4.BJJ-2018-1109.R1
National Institutes of Health (2023) Study quality assessment tools. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed 14 Apr 2023
Christopher ZK, McQuivey KS, Deckey DG, Haglin J, Spangehl MJ, Bingham JS (2021) Acute or chronic periprosthetic joint infection? Using the ESR ∕ CRP ratio to aid in determining the acuity of periprosthetic joint infections. J Bone Joint Infect 6(6):229–234. https://doi.org/10.5194/jbji-6-229-2021
Kapadia BH, Berg RA, Daley JA, Fritz J, Bhave A, Mont MA (2016) Periprosthetic joint infection. Lancet (Lond Engl) 387(10016):386–394. https://doi.org/10.1016/S0140-6736(14)61798-0
Huotari K, Peltola M, Jämsen E (2015) The incidence of late prosthetic joint infections: a registry-based study of 112,708 primary hip and knee replacements. Acta Orthop 86(3):321–325. https://doi.org/10.3109/17453674.2015.1035173
Kuo CL, Chang JH, Wu CC, Shen PH, Wang CC, Lin LC, Shen HC, Lee CH (2011) Treatment of septic knee arthritis: comparison of arthroscopic debridement alone or combined with continuous closed irrigation-suction system. J Trauma 71(2):454–459. https://doi.org/10.1097/TA.0b013e3181ec4734
Schurman DJ, Hirshman HP, Kajiyama G, Moser K, Burton DS (1978) Cefazolin concentrations in bone and synovial fluid. J Bone Joint Surg Am 60(3):359–362
Parvizi J, Zmistowski B, Adeli B (2010) Periprosthetic joint infection: treatment options. Orthopedics 33(9):659. https://doi.org/10.3928/01477447-20100722-42
Ometti M, Delmastro E, Salini V (2022) Management of prosthetic joint infections: a guidelines comparison. Musculoskelet Surg 106(3):219–226. https://doi.org/10.1007/s12306-021-00734-7
Lazic I, Scheele C, Pohlig F, von Eisenhart-Rothe R, Suren C (2021) Treatment options in PJI—is two-stage still gold standard? J Orthop 23:180–184. https://doi.org/10.1016/j.jor.2020.12.021
Kunutsor SK, Whitehouse MR, Blom AW, Beswick AD, INFORM Team (2015) Re-infection outcomes following one- and two-stage surgical revision of infected hip prosthesis: a systematic review and meta-analysis. PLoS ONE 10(9):e0139166. https://doi.org/10.1371/journal.pone.0139166
Kunutsor SK, Whitehouse MR, Lenguerrand E, Blom AW, Beswick AD, INFORM Team (2016) Re-infection outcomes following one- and two-stage surgical revision of infected knee prosthesis: a systematic review and meta-analysis. PLoS ONE 11(3):e0151537. https://doi.org/10.1371/journal.pone.0151537
Bosco F, Cacciola G, Giustra F, Risitano S, Capella M, Vezza D, Barberis L, Cavaliere P, Massè A, Sabatini L (2023) Characterizing recurrent infections after one-stage revision for periprosthetic joint infection of the knee: a systematic review of the literature. Eur J Orthopaed Surg Traumatol Orthopedie Traumatol 33(7):2703–2715. https://doi.org/10.1007/s00590-023-03480-7
Corona PS, Vicente M, Carrera L, Rodríguez-Pardo D, Corró S (2020) Current actual success rate of the two-stage exchange arthroplasty strategy in chronic hip and knee periprosthetic joint infection. Bone Joint J 102(12):1682–1688. https://doi.org/10.1302/0301-620X.102B12.BJJ-2020-0792.R1
Okafor CE, Nghiem S, Byrnes J (2023) One-stage revision versus debridement, antibiotics, and implant retention (DAIR) for acute prosthetic knee infection: an exploratory cohort study. Arch Orthop Trauma Surg 143(9):5787–5792. https://doi.org/10.1007/s00402-023-04891-1
Leta TH, Lygre SHL, Schrama JC, Hallan G, Gjertsen JE, Dale H, Furnes O (2019) Outcome of revision surgery for infection after total knee arthroplasty: results of 3 surgical strategies. JBJS Rev 7(6):e4. https://doi.org/10.2106/JBJS.RVW.18.00084
Gallo J, Smizanský M, Radová L, Potomková J (2009) Porovnání lécebných postupů pouzívaných v terapii infekce kloubních náhrad kycle a kolena [Comparison of therapeutic strategies for hip and knee prosthetic joint infection]. Acta Chir Orthop Traumatol Cech 76(4):302–309
Kunutsor SK, Whitehouse MR, Blom AW, Board T, Kay P, Wroblewski BM, Zeller V, Chen SY, Hsieh PH, Masri BA, Herman A, Jenny JY, Schwarzkopf R, Whittaker JP, Burston B, Huang R, Restrepo C, Parvizi J, Rudelli S, Honda E, Global Infection Orthopaedic Management Collaboration (2018) One- and two-stage surgical revision of peri-prosthetic joint infection of the hip: a pooled individual participant data analysis of 44 cohort studies. Eur J Epidemiol 33(10):933–946. https://doi.org/10.1007/s10654-018-0377-9
Walkay S, Wallace DT, Balasubramaniam VSC, Maheshwari R, Changulani M, Sarungi M (2022) Outcomes of debridement, antibiotics and implant retention (DAIR) for periprosthetic joint infection in a high-volume arthroplasty centre. Indian J Orthopaed 56(8):1449–1456. https://doi.org/10.1007/s43465-022-00655-y
Nurmohamed FRHA, van Dijk B, Veltman ES, Hoekstra M, Rentenaar RJ, Weinans HH, Vogely HC, van der Wal BCH (2021) One-year infection control rates of a DAIR (debridement, antibiotics and implant retention) procedure after primary and prosthetic-joint-infection-related revision arthroplasty—a retrospective cohort study. J Bone Joint Infect 6(4):91–97. https://doi.org/10.5194/jbji-6-91-2021
Deijkers RL, van Elzakker EPM, Pijls BG (2020) Debridement, antibiotics, and implant retention with the direct anterior approach for acute periprosthetic joint infection following primary THA. JB JS Open Access 5(2):e0062. https://doi.org/10.2106/JBJS.OA.19.00062
Azzam KA, Seeley M, Ghanem E, Austin MS, Purtill JJ, Parvizi J (2010) Irrigation and debridement in the management of prosthetic joint infection: traditional indications revisited. J Arthroplasty 25(7):1022–1027. https://doi.org/10.1016/j.arth.2010.01.104
Blom AW, Taylor AH, Pattison G, Whitehouse S, Bannister GC (2003) Infection after total hip arthroplasty. The Avon experience. J Bone Joint Surg Br 85(7):956–959. https://doi.org/10.1302/0301-620x.85b7.14095
Crockarell JR, Hanssen AD, Osmon DR, Morrey BF (1998) Treatment of infection with débridement and retention of the components following hip arthroplasty. J Bone Joint Surg Am 80(9):1306–1313. https://doi.org/10.2106/00004623-199809000-00009
Manrique J, Komnos GA, Tan TL, Sedgh S, Shohat N, Parvizi J (2019) Outcomes of superficial and deep irrigation and debridement in total hip and knee arthroplasty. J Arthroplasty 34(7):1452–1457. https://doi.org/10.1016/j.arth.2019.03.032
Wouthuyzen-Bakker M, Sebillotte M, Lomas J, Taylor A, Doufares EB, Murillo O, Parvizi J, Shohat N, Reinoso JC, Sánchez RE, Fernandez-Sampedro M, Senneville E, Huotari K, Barbero JM, Garcia-Cañete J, Lora-Tamayo J, Ferrari MC, Vaznaisiene D, Yusuf E, Aboltins C (2019) Clinical outcome and risk factors for failure in late acute prosthetic joint infections treated with debridement and implant retention. J Infect 78(1):40–47. https://doi.org/10.1016/j.jinf.2018.07.014
Hirakawa K, Stulberg BN, Wilde AH, Bauer TW, Secic M (1998) Results of 2-stage reimplantation for infected total knee arthroplasty. J Arthroplasty 13(1):22–28. https://doi.org/10.1016/s0883-5403(98)90071-7
Mittal Y, Fehring TK, Hanssen A, Marculescu C, Odum SM, Osmon D (2007) Two-stage reimplantation for periprosthetic knee infection involving resistant organisms. J Bone Joint Surg Am 89(6):1227–1231. https://doi.org/10.2106/JBJS.E.01192
Tornero E, García-Oltra E, García-Ramiro S, Martínez-Pastor JC, Bosch J, Climent C, Morata L, Camacho P, Mensa J, Soriano A (2012) Prosthetic joint infections due to Staphylococcus aureus and coagulase-negative staphylococci. Int J Artif Organs 35(10):884–892. https://doi.org/10.5301/ijao.5000148
Barberán J (2006) Management of infections of osteoarticular prosthesis. Clin Microbiol Infect 12(Suppl 3):93–101. https://doi.org/10.1111/j.1469-0691.2006.01400.x
Wolf CF, Gu NY, Doctor JN, Manner PA, Leopold SS (2011) Comparison of one and two-stage revision of total hip arthroplasty complicated by infection: a Markov expected-utility decision analysis. J Bone Joint Surg Am 93(7):631–639. https://doi.org/10.2106/JBJS.I.01256
Azzam K, McHale K, Austin M, Purtill JJ, Parvizi J (2009) Outcome of a second two-stage reimplantation for periprosthetic knee infection. Clin Orthop Relat Res 467(7):1706–1714. https://doi.org/10.1007/s11999-009-0739-4
Nayfeh T, Whiteside LA, Hirsch M (2004) Direct exchange treatment of septic total joint arthroplasty with intra-articular infusion of antibiotics: technique and early results. Orthopedics 27(9):987–988. https://doi.org/10.3928/0147-7447-20040901-40
Thakrar RR, Horriat S, Kayani B, Haddad FS (2019) Indications for a single-stage exchange arthroplasty for chronic prosthetic joint infection: a systematic review. Bone Joint J. 101(1):19–24. https://doi.org/10.1302/0301-620X.101B1.BJJ-2018-0374.R1
Razii N, Clutton JM, Kakar R, Morgan-Jones R (2021) Single-stage revision for the infected total knee arthroplasty: the Cardiff experience. Bone Joint Open 2(5):305–313. https://doi.org/10.1302/2633-1462.25.BJO-2020-0185.R1
Brunt ACC, Gillespie M, Holland G, Brenkel I, Walmsley P (2022) Results of “two-in-one” single-stage revision total knee arthroplasty for infection with associated bone loss : prospective five-year follow up. Bone Joint Open 3(2):107–113. https://doi.org/10.1302/2633-1462.32.BJO-2021-0148.R1
Ham A, Goyal N, Harris IA, Chen DB, MacDessi SJ (2016) Infection rates with use of intra-articular pain catheters in total knee arthroplasty. ANZ J Surg 86(5):391–394. https://doi.org/10.1111/ans.13486
McDonald DA, Siegmeth R, Deakin AH, Kinninmonth AW, Scott NB (2012) An enhanced recovery programme for primary total knee arthroplasty in the United Kingdom–follow up at one year. Knee 19(5):525–529. https://doi.org/10.1016/j.knee.2011.07.012
Anagnostakos K, Wilmes P, Schmitt E, Kelm J (2009) Elution of gentamicin and vancomycin from polymethylmethacrylate beads and hip spacers in vivo. Acta Orthop 80(2):193–197. https://doi.org/10.3109/17453670902884700
Stanton IC, Murray AK, Zhang L, Snape J, Gaze WH (2020) Evolution of antibiotic resistance at low antibiotic concentrations including selection below the minimal selective concentration. Commun Biol 3(1):467. https://doi.org/10.1038/s42003-020-01176-w
Nadeem SF, Gohar UF, Tahir SF, Mukhtar H, Pornpukdeewattana S, Nukthamna P, Moula Ali AM, Bavisetty SCB, Massa S (2020) Antimicrobial resistance: more than 70 years of war between humans and bacteria. Crit Rev Microbiol 46(5):578–599. https://doi.org/10.1080/1040841X.2020.1813687
Funding
On behalf of all the authors, the corresponding author states that there is no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all the authors, the corresponding author states that there is no conflict of interest.
Ethical approval
On behalf of all the authors, the corresponding author states that there was no ethical approval needed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bruyninckx, S., Metsemakers, W.J., Depypere, M. et al. Local antibiotic delivery via intra-articular catheter infusion for the treatment of periprosthetic joint infection: a systematic review. Arch Orthop Trauma Surg (2024). https://doi.org/10.1007/s00402-024-05341-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00402-024-05341-2