Abstract
Background
The use of 3D planning to guide corrective osteotomies of the lower extremity is increasing in clinical practice. The use of computer-tomography (CT) data acquired in supine position neglects the weight-bearing (WB) state and the gold standard in 3D planning involves the manual adaption of the surgical plan after considering the WB state in long-leg radiographs (LLR). However, this process is subjective and dependent on the surgeons experience. A more standardized and automated method could reduce variability and decrease costs.
Purpose
The aim of the study was (1) to compare three different three-dimensional (3D) planning modalities for medial open-wedge high tibial osteotomy (MOWHTO) and (2) to describe the current practice of adapting NWB CT data after considering the WB state in LLR. The purpose of this study is to validate a new, standardized approach to include the WB state into the 3D planning and to compare this method against the current gold standard of 3D planning. Our hypothesis is that the correction is comparable to the gold standard, but shows less variability due compared to the more subjective hybrid approach.
Methods
Three surgical planning modalities were retrospectively analyzed in 43 legs scheduled for MOWHTO between 2015 and 2019. The planning modalities included: (1) 3D hybrid (3D non-weight-bearing (NWB) CT models after manual adaption of the opening angle considering the WB state in LLR, (2) 3D NWB (3D NWB CT models) and (3) 3D WB (2D/3D registration of 3D NWB CT models onto LLR to simulate the WB state). The pre- and postoperative hip-knee-ankle angle (HKA) and the planned opening angle (°) were assessed and differences among modalities reported. The relationship between the reported differences and BMI, preoperative HKA (LLR), medial meniscus extrusion, Outerbridge osteoarthritis grade and joint line convergence angle (JLCA) was analyzed.
Results
The mean (std) planned opening angle of 3D hybrid did not differ between 3D hybrid and 3D WB (0.4 ± 2.1°) (n.s.) but was higher in 3D hybrid compared to 3D NWB (1.1° ± 1.1°) (p = 0.039). 3D WB demonstrated increased preoperative varus deformity compared to 3D NWB: 6.7 ± 3.8° vs. 5.6 ± 2.7° (p = 0.029). Patients with an increased varus deformity in 3D WB compared to 3D NWB (> 2 °) demonstrated more extensive varus alignment in LLR (p = 0.009) and a higher JLCA (p = 0.013).
Conclusion
Small intermodal differences between the current practice of the reported 3D hybrid planning modality and a 3D WB approach using a 2D/3D registration algorithm were reported. In contrast, neglecting the WB state underestimates preoperative varus deformity and results in a smaller planned opening angle. This leads to potential under correction in MOWHTO, especially in patients with extensive varus deformities or JLCA.
Clinical Relevance
Incorporating the WB state in 3D planning modalities has the potential to increase accuracy and lead to a more consistent and reliable planning in MOWHTO. The inclusion of the WB state in automatized surgical planning algorithms has the potential to reduce costs and time in the future.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Preoperative planning for lower extremity realignment surgery is widely based on two-dimensional (2D) weight-bearing (WB) long-leg radiographs (LLR), as this modality allows the quantification of the leg axis deviation under WB load [1]. Over the last years, surgical planning modalities based on computed tomography (CT) reconstructed three-dimensional (3D) models have been proposed [2,3,4]. 3D models can provide the surgeon with a more detailed understanding of the underlying deformity. The use of 3D deformity analysis and surgical planning supports the surgeon in the accurate execution of the pre-defined plan through surgical navigation, such as patient-specific instruments [2]. This allows the concomitant correction in multiple planes and prevents unintentional alterations in sagittal or axial alignment during lower extremity corrections [5,6,7]. Despite these advancements using 3D planning and navigation, the models rely solely on CT imaging acquired in a non-weight-bearing (NWB) supine position, neglecting the impact of the WB state on the limb (subsequently referred to as 3D NWB) [8, 9]. Therefore, in current practice the surgeon needs to adapt the surgical correction based on 3D NWB CT models after considering the extent of preoperative deformity under WB conditions in LLR (subsequently referred to as 3D hybrid). However, this decision is dependent on the individual surgeon’s experience and therefore the planning modality lacks standardization and validation, which leads to undesired variability, limited reproducibility and comparability in the literature up to date. Additionally, manual planning is associated with higher costs and time, which could be addressed with automated planning algorithms in the future. D.
Previous studies have investigated the use of 3D/2D registration algorithms to transform CT imaging data onto 2D x-ray modalities for various clinical use cases [10]. For corrective osteotomies of the lower extremities, Roth. et al. proposed a registration algorithm to transform the 3D NWB CT model into the WB state [11]. The 3D/2D registration of 3D NWB CT models onto biplanar standing LLR enables 3D surgical planning under consideration of the WB state (subsequently referred to as 3D WB).
However, the use of a 3D WB modality to plan medial open-wedge high tibial osteotomies (MOWHTO) has not been studied yet and differences to current planning approaches (3D NWB and 3D hybrid) are not validated. Therefore, the aim of this study is to validate a new, standardized approach to include the WB state into the 3D planning and to compare this method against the current gold standard of 3D planning. Our hypothesis is that the correction is comparable to the gold standard, but shows less variability due compared to the more subjective hybrid approach.
Methods
Study cohort
After ethical approval (ID 2017 ? 01616), 59 consecutive legs identified from a previous study that underwent biplanar LLR and a standardized lower extremity CT protocol at our institution from 2015 to 2019 were screened [11]. Inclusion criteria comprised a complete pre- and postoperative biplanar LLR, a standardized CT protocol (including the hip, knee and ankle joints) and complete documentation of the preoperative surgical planning.
After excluding patients with insufficient preoperative documentation of the surgical planning or deformity analysis (n = 9), torsional realignment (n = 2), extensive flexion position in LLR (> 20°) (n = 3), a shaft correction (n = 1), and a planned varization (n = 1), 43 legs (41 patients) planned for an MOWHTO due to medial knee degeneration or focal chondral defects that underwent cartilage surgery were available for definitive analysis. Demographic characteristics are summarized in Table 1.
We sought to analyze three different preoperative planning methods: (1) the current standard planning modality at our institution 3D NWB CT model-based planning which was manually adapted based on standing LLR (referred to as 3D hybrid), (2) 3D NWB CT model-based planning (referred to as 3D NWB), and 3)3D NWB CT model-based planning after a 3D/2D registration onto standing LLR to simulate the WB state (referred to as 3D WB). The three modalities are explained in detail in the paragraphs hereafter. The preoperative planning was retrospectively reviewed for each patient and modality (3D hybrid, 3D NWB, 3D WB).
Radiographic assessment
Radiographic assessment of leg alignment included biplanar standing LLR (EOS Imaging, Paris, France). The frontal LLR was imported to mediCAD® software (Hectec GmbH, Altdorf, Germany) and calibrated. After manual definition of landmarks (center of the femoral head, apex of the greater trochanter, femoral and tibial joint line, medial and lateral border of the femoral condyles and tibial plateau, medial and lateral border of the talus, and the joint line of the talus), automatic deformity analysis is performed by the software according to Paley et al. [12]. Preoperative deformity analysis included HKA (°) (+ varus, - valgus), mechanical medial proximal tibia angle (°) (mMPTA) and mechanical lateral distal femoral angle (°) (mLDFA). Joint line convergence angle (°) (JLCA) (+ lateral opening, - medial opening) was measured in standing x-ray. Additionally, medial meniscus extrusion (mm) [13] and Outerbridge grade of the medial compartment [14] were assessed in preoperative magnetic-resonance imaging(MRI) if preoperative MRI was available by a blinded investigator who was not involved in clinical care of the patients. Preoperative leg alignment and MRI findings are summarized in Table 1.
Computer-tomography protocol and three-dimensional models
All patients underwent preoperative supine CT of the lower extremity according to a standardized protocol (MyOsteotomy, Medacta, Castel San Pietro, Switzerland) comprising all anatomical structures of interest: hip center, proximal femur, knee center with distal femur and proximal tibia, ankle joint center with distal tibia, distal fibula and talus. 3D surface models of the lower extremities were created using global threshold segmentation and region growing with MIMICS software (MIMICS, Materialize, Belgium) and imported into the in-house developed surgical planning software (Xxxxxxxxxx). A 3D coordinate system was defined according to the International Society of Biomechanics (ISB) [15]. The hip center was defined as the center of a sphere, fitted to the femoral head. The knee center was defined as the midpoint between the intercondylar eminences on the tibial plateau and the ankle center was defined as the center of the distal articular surfaces of the tibia and fibula [8].
Planning modalities
For all planning modalities the preoperative HKA (referred to as HKA pre) (°), planned postoperative HKA (referred to as HKA post) (°) and the planned opening angle (°) were measured. The extent of correction to shift the weight-bearing line (WBL) 50–65% on the tibial plateau was defined on an individual basis, considering the indication for realignment, concomitant lateral and patellofemoral degeneration and the joint line obliquity (mMPTA < = 93°) as described by Feucht et al. [16]. The aimed postoperative correction (% of WBL on tibial plateau) was identical in all planning modalities.
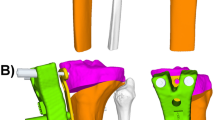
3D hybrid
3D planning for lower extremity realignment surgery represents the state-of-the art method at our institution. After preliminary planning of realignment surgery in 3D NWB CT [2], the definitive planned opening angle is manually adapted by the treating surgeon after considering the extent of deformity in standing LLR and is therefore referred to as 3D hybrid. Increasing the initially suggested opening angle of the 3D NWB plan was considered in patients with increased HKA in LLR compared to the 3D NWB model, to adjust for the missing WB state in the 3D models. For each 3D model, HKA pre and HKA post were measured as the projected 2D angle in the frontal plane between a line defined by hip and knee center, and a line defined by knee and ankle center. The medial opening angle of the tibia was calculated around a single 3D axis of rotation. This 3D planning modality has been previously described and demonstrated excellent reliability [2, 5, 17] (Fig. 1, left).
Overview of planning modalities. The planned correction of the mechanical leg axis was analyzed in 3D hybrid (left), 3D non-weight-bearing (NWB) (middle) and 3D weight-bearing (WB) modality (right) for each patient. Left: 3D hybrid is based on NWB 3D CT models and adapted by the surgeon after consideration of WB information from the long-leg-radiograph (LLR) (red box). Middle: 3D NWB relies solely on NWB information from supine acquired 3D CT models. Right: 3D WB allowed the analysis of 3D models in the WB-state after 3D/2D registration of NWB CT models onto standing LLR. The mannikin indicates the lying or standing position during image acquisition for each modality
3D non-weight-bearing (NWB)
3D NWB planning relies solely on the CT models obtained in a supine position without additional information of the WB state. The protocol included exactly the same CT scan, creation of 3D models, definition of joint centers and measurements as described above for the 3D hybrid method. However, the deformity analysis and correction were based on supine imaging only and the WB state was not considered (Fig. 1, middle).
3D (weight-bearing (WB)
The consideration of the WB state in 3D planning represents a novel planning modality [11]. An intensity-based algorithm was used to register NWB CT scans onto standing LLR to transform the patient-specific 3D models into the WB state. After annotation of the corresponding anatomical landmarks (ankle center, knee center, hip center) in EOS and CT NWB [11], the registration algorithm detects the optimal position by comparing intensity values between the LLR and digitally reconstructed radiographs (DRR) generated from CT using the same geometry as the EOS system [18]. The registration was executed using ImFusion Suite software (ImFusion GmbH, Munich, Germany). Once registration to the WB state was completed, the measurement of HKA pre and HKA post was performed as described for the 3D hybrid method (Fig. 1, right).
Mean differences between the opening angle of 3D hybrid, 3D NWB and 3D WB were calculated. Additionally, the influence of body-mass index (BMI), preoperative HKA in LLR, medial compartment osteoarthritis grade (Outerbridge) [14], medial meniscus extrusion and JLCA on the reported differences were investigated.
Statistical analysis
The normal distribution of the data was tested with Shapiro-Wilk’s test. Data are reported as mean ± standard deviation (std) or counts (percentages).
Differences between planned correction of HKA among the three planning modalities were tested with Friedman’s test and post-hoc tests were Bonferroni corrected. The planned opening angle for the three methods were analyzed using equivalence testing after calculating tge effect sizes (Cohen’s D) assuming a clinically meaningful border that demonstrates equivalence with a 90% CI of -0.5 to 0.5°. The relationship between the adaption of the opening angle, BMI, preoperative HKA, medial compartment osteoarthritis grade, medial meniscus extrusion, JLCA and the reported differences of 3D NWB and 3D WB were analyzed using Spearman’s rank correlation (rs). Characteristics between a subgroup of patients with > 2° difference between preoperative varus alignment in 3D WB compared to 3D NWB and a subgroup with < 2° difference were reported (metric: student’s t-test, categoric: Chi-Square test). Significance was set at the level of p < 0.05. Data were analyzed with SPSS version 26 (SPSS Inc, Chicago, IL, USA).
Results
The mean (std) planned opening angle did not differ between 3D hybrid and 3D WB (0.4 ± 2.1°) (n.s.) but was higher in 3D hybrid compared to 3D NWB (1.1° ± 1.1°) (p = 0.039) (Fig. 2). The 3D hybrid and 3D WB demonstrated equivalence (Cohen’s D CI: -0.25 to 0.46), whereas the 3D hybrid and 3D NWB were non-equivalent (Cohen’s D CI: -0.61 to 0.09). The detailed results of all planning modalities are listed in Table 2. The adapted correction based on LLR in the 3D hybrid method correlated with the difference between preoperative HKA of CT WB and NWB rs =0.54 (p = 0.001).
Planned correction of hip-knee ankle angle (HKA) among modalities. Boxplots depicts median (line), IQR (box), minimum and maximum (whisker), and outliers (stars) among planning modalities Preoperative deformity of hip-knee-ankle angle (HKA) was significantly smaller in 3D NWB compared to 3D WB (p = 0.029, Bonferroni corrected, depicted by *). The opening angle was significantly higher in the 3D hybrid method compared to the 3D NWB (p = 0.039, Bonferroni corrected, depicted by +). The remaining measurements did not differ among the three planning modalities (n.s.)
Discussion
The most important finding of this study is that the described 3D hybrid and 3D WB modality for planning lower extremity realignment demonstrated small intermodal differences, while the 3D NWB approach significantly underestimated the preoperative varus deformity and therefore resulted in a decreased planned opening angle in MOWHTO. The simulation of the WB state with the described 3D/2D registration algorithm represents a valid alternative to the current standard 3D hybrid planning approach. While the differences for 2D planning methods for HTO have been studied before [19], this is the first study to report the differences among state-of-the art 3D planning methods for corrective osteotomies with and without consideration of the WB state.
Preoperative planning of MOWHTO allows the identification of the deformity site and subsequent accurate lower extremity realignment [20]. Accurate surgical planning and execution are crucial to avoid under- and over correction and adequately unload the degenerative medial compartment [21, 22] without creating an oblique joint line [23, 24]. Therefore, currently conventional planning still relies on standing 2D LLR, which allows the consideration of the WB state. While the adaption towards 3D planning modalities has gained attention, including the WB state has only been proposed recently [11]. This study is the first to report the differences between different 3D modalities (WB vs. NWB) in surgical planning of lower extremity realignment. The analyzed surgical planning in 3D WB allows a reliable planning with a mean difference of 0.4° compared to the current standard planning using the 3D hybrid method. Including the WB information in an automatized planning algorithm, without the need of a cumbersome method to account for the missing WB information in 3D CT models acquired in supine position could potentially reduce cost, time and undesired surgeon-dependent variability in the future [25].
The extent of preoperative varus deformity and increasing JLCA were identified as contributing factors that explain the difference between preoperative HKA of 3D NWB and 3D WB. Patients with increasing varus deformity under WB load demonstrated increasing meniscus extrusion and medial cartilage degeneration, however, not significant in our cohort. An increase of preoperative varus deformity shifts the load to the medial side of the knee and may explain the differences of preoperative HKA between 3D NWB and 3D WB in the presence of medial compartment degeneration and joint space narrowing. The combination of cartilage degeneration, meniscus extrusion and ligament laxity on the lateral side leads to closing of the medial articular joint space under load and is in line with previous findings [26,27,28,29]. However, several other factors contributing to the reported differences between 3D WB and 3D NWB need to be considered. First, LLR measurements are dependent on patient positioning, knee flexion and beam height [30] and therefore influence the 3D/2D registration of the reported 3D WB protocol. Second, the 3D WB modality inherently includes the reported translational and rotational registration errors [11].
A limitation of this study is that the surgical planning was retrospectively reviewed in a single-center cohort. Therefore, the decision to adapt the 3D hybrid method by the treating surgeon is based on multiple factors and only the main ones could be described in the current study. However, this represents current clinical practice, especially as the optimal amount of leg axis correction remains controversial [16, 31]. Additionally, the analyzed cohort included patients planned for MOWHTO with varus deformity only. Therefore, these findings need to be validated for femoral-sided and valgus corrections in further studies. Future research should focus on automatic inclusion of the WB state in 3D planning to minimize undesired user-dependent heterogeneity in surgical planning of lower extremity realignment.
Conclusion
Small intermodal differences between the current practice of the reported 3D hybrid planning modality and a 3D WB approach using a 2D/3D registration algorithm were reported. In contrast, neglecting the WB state underestimates preoperative varus deformity and results in a smaller planned opening angle. This leads to potential under correction in MOWHTO, especially in patients with extensive varus deformities or JLCA.
Clinical relevance
Incorporating the WB state in 3D planning modalities has the potential to increase accuracy and lead to a more consistent and reliable planning in MOWHTO. The inclusion of the WB state in automatized surgical planning algorithms has the potential to reduce costs and time in the future.
References
Pape D, Seil R, Adam F, Rupp S, Kohn D, Lobenhoffer P (2004) [Imaging and preoperative planning of osteotomy of tibial head osteotomy]. Orthopade 33(2):122–134. https://doi.org/10.1007/s00132-003-0585-0
Fucentese SF, Meier P, Jud L, Köchli GL, Aichmair A, Vlachopoulos L et al (2020) Accuracy of 3D-planned patient specific instrumentation in high tibial open wedge valgisation osteotomy. J Exp Orthop 7(1):7. https://doi.org/10.1186/s40634-020-00224-y
Ellis RE, Tso CY, Rudan JF, Harrison MM (1999) A surgical planning and guidance system for high tibial osteotomy. Comput Aided Surg 4(5):264–274. https://doi.org/10.1002/(SICI)1097-0150(1999)4:5<264::AID-IGS4>3.0.CO;2-E
Fürnstahl PSA, Graf M, Vlachopoulos L, Fucentese S, Wirth S (2016) S urgical treatment of long-bone deformities: 3D preoperative planning and patient-specific instrumentation. Computational radiology for orthopaedic interventions. Springer, New York, pp 123–149
Hodel S, Zindel C, Jud L, Vlachopoulos L, Fürnstahl P, Fucentese SF (2021) Influence of medial open wedge high tibial osteotomy on tibial tuberosity-trochlear groove distance. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06574-z
Jud L, Vlachopoulos L, Häller TV, Fucentese SF, Rahm S, Zingg PO (2020) The impact of mal-angulated femoral rotational osteotomies on mechanical leg axis: a computer simulation model. BMC Musculoskelet Disord 21(1):50. https://doi.org/10.1186/s12891-020-3075-1
Flury A, Hoch A, Hodel S, Imhoff FB, Fucentese SF, Zingg PO (2022) No relevant mechanical leg axis deviation in the frontal and sagittal planes is to be expected after subtrochanteric or supracondylar femoral rotational or derotational osteotomy. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06843-x
Jud L, Roth T, Fürnstahl P, Vlachopoulos L, Sutter R, Fucentese SF (2020) The impact of limb loading and the measurement modality (2D versus 3D) on the measurement of the limb loading dependent lower extremity parameters. BMC Musculoskelet Disord 21(1):418. https://doi.org/10.1186/s12891-020-03449-1
León-Muñoz VJ, López-López M, Martínez-Martínez F, Santonja-Medina F (2020) Comparison of weight-bearing full-length radiographs and computed-tomography-scan-based three-dimensional models in the assessment of knee joint coronal alignment. Knee 27(2):543–551. https://doi.org/10.1016/j.knee.2019.11.017
Unberath M, Gao C, Hu Y, Judish M, Taylor RH, Armand M et al (2021) The impact of machine learning on 2D/3D Registration for Image-guided interventions: a systematic review and perspective. Front Robot AI 8:716007. https://doi.org/10.3389/frobt.2021.716007
Roth T, Carrillo F, Wieczorek M, Ceschi G, Esfandiari H, Sutter R et al (2021) Three-dimensional preoperative planning in the weight-bearing state: validation and clinical evaluation. Insights Imaging 12(1):44. https://doi.org/10.1186/s13244-021-00994-8
Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A (1994) Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am 25(3):425–465
Costa CR, Morrison WB, Carrino JA (2004) Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol 183(1):17–23. https://doi.org/10.2214/ajr.183.1.1830017
OUTERBRIDGE RE (1961) The etiology of chondromalacia patellae. J Bone Joint Surg Br 43. https://doi.org/10.1302/0301-620X.43B4.752. -B:752-7
Wu G, Siegler S, Allard P, Kirtley C, Leardini A, Rosenbaum D et al (2002) ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion–part I: ankle, hip, and spine. Int Soc Biomech J Biomech 35(4):543–548. https://doi.org/10.1016/s0021-9290(01)00222-6
Feucht MJ, Minzlaff P, Saier T, Cotic M, Südkamp NP, Niemeyer P et al (2014) Degree of axis correction in valgus high tibial osteotomy: proposal of an individualised approach. Int Orthop 38(11):2273–2280. https://doi.org/10.1007/s00264-014-2442-7
Fürnstahl PSA, Graf M, Vlachopoulos L, Fucentese S, Wirth S Surgical treatment of long-bone deformities: 3D preoperative planning and patient-specific instrumentation. Comput Radiol Orthop Interventions 2016:p. 123–149
Goitein M, Abrams M, Rowell D, Pollari H, Wiles J (1983) Multi-dimensional treatment planning: II. Beam’s eye-view, back projection, and projection through CT sections. Int J Radiat Oncol Biol Phys 9(6):789–797. https://doi.org/10.1016/0360-3016(83)90003-2
Matsushita T, Watanabe S, Araki D, Nagai K, Hoshino Y, Kanzaki N et al (2021) Differences in preoperative planning for high-tibial osteotomy between the standing and supine positions. Knee Surg Relat Res 33(1):8. https://doi.org/10.1186/s43019-021-00090-7
Feucht MJ, Winkler PW, Mehl J, Bode G, Forkel P, Imhoff AB et al (2021) Isolated high tibial osteotomy is appropriate in less than two-thirds of varus knees if excessive overcorrection of the medial proximal tibial angle should be avoided. Knee Surg Sports Traumatol Arthrosc 29(10):3299–3309. https://doi.org/10.1007/s00167-020-06166-3
El-Azab HM, Morgenstern M, Ahrens P, Schuster T, Imhoff AB, Lorenz SG (2011) Limb alignment after open-wedge high tibial osteotomy and its effect on the clinical outcome. Orthopedics 34(10):e622–e628. https://doi.org/10.3928/01477447-20110826-02
Jung WH, Takeuchi R, Chun CW, Lee JS, Ha JH, Kim JH et al (2014) Second-look arthroscopic assessment of cartilage regeneration after medial opening-wedge high tibial osteotomy. Arthroscopy 30(1):72–79. https://doi.org/10.1016/j.arthro.2013.10.008
Goshima K, Sawaguchi T, Shigemoto K, Iwai S, Fujita K, Yamamuro Y (2019) Osteotomy Arthrosc 35(10):2898–908e. https://doi.org/10.1016/j.arthro.2019.04.030. Comparison of Clinical and Radiologic Outcomes Between Normal and Overcorrected Medial Proximal Tibial Angle Groups After Open-Wedge High Tibial
Nakayama H, Schröter S, Yamamoto C, Iseki T, Kanto R, Kurosaka K et al (2018) Large correction in opening wedge high tibial osteotomy with resultant joint-line obliquity induces excessive shear stress on the articular cartilage. Knee Surg Sports Traumatol Arthrosc 26(6):1873–1878. https://doi.org/10.1007/s00167-017-4680-x
Mitterer JA, Huber S, Schwarz GM, Simon S, Pallamar M, Kissler F et al (2023) Fully automated assessment of the knee alignment on long leg radiographs following corrective knee osteotomies in patients with valgus or varus deformities. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-023-05151-y
Goto N, Okazaki K, Akiyama T, Akasaki Y, Mizu-Uchi H, Hamai S et al (2019) Alignment factors affecting the medial meniscus extrusion increases the risk of osteoarthritis development. Knee Surg Sports Traumatol Arthrosc 27(8):2617–2623. https://doi.org/10.1007/s00167-018-5286-7
Lee YS (2022) Editorial Commentary: patient-specific instrumentation for knee high tibial osteotomy addresses the Bony but not the soft-tissue aspect of deformity correction. Arthroscopy 38(9):2759–2760. https://doi.org/10.1016/j.arthro.2022.05.008
Kim JE, Kim DH, Lee JI, Choi HG, Jung YS, Lee SH et al (2021) Difference of preoperative varus-valgus stress radiograph is effective for the correction accuracy in the preoperative planning during open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 29(4):1035–1044. https://doi.org/10.1007/s00167-020-06076-4
Jeong HW, Shim SJ, Park SY, Lee YS (2023) Analysis of the determinant factor of the medial joint space width after medial opening wedge high tibial osteotomy. Arch Orthop Trauma Surg 143(8):4879–4888. https://doi.org/10.1007/s00402-023-04818-w
a HCNabWPGaNvEaHWaCHSbRJBSaRJHC. The need for a standardized whole leg radiograph guideline: the effects of knee flexion, leg rotation, and X-ray beam height. 1. Journal of Cartilage & Joint Preservation; (2021)
Strecker W, Dickschas J, Harrer J, Müller M (2009) [Arthroscopy prior to osteotomy in cases of unicondylar osteoarthritis]. Orthopade 38(3):263–268. https://doi.org/10.1007/s00132-008-1390-6
Funding
Open access funding provided by University of Zurich
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest or funding
This study was partially funded by the Swiss National Science Foundation (Grant Nr. 320030_182352/1).
Sandro Fucentese is a consultant for Medacta SA (Switzerland), Zimmer Biomet (USA), Smith & Nephew (United Kingdom) and Karl Storz SE & Co. KG (Germany). Sandro Fucentese is a board member of the EKA-ESSKA osteotomy expert group.
The remaining offers have nothing to disclose.
Ethics
Written informed consent was obtained from all patients and ethics protocol was approved by the Cantonal Ethics Committee Zurich (ID 2017 − 01616).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hodel, S., Arn-Roth, T., Haug, F. et al. The influence of the weight-bearing state on three-dimensional (3D) planning in lower extremity realignment – analysis of novel vs. state-of-the-art planning approaches. Arch Orthop Trauma Surg 144, 1989–1996 (2024). https://doi.org/10.1007/s00402-024-05289-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-024-05289-3