Abstract
Introduction
Intraoperative periprosthetic fracture, one of the most frequent complications of total hip arthroplasty, is a very important factor that affects rehabilitation, hospitalization time, and cost of treatment. Osteoporosis is common in total hip arthroplasty patients and likely contributes to the increasing incidence of periprosthetic fracture. Despite this awareness, preoperative and postoperative osteoporosis evaluations remain insufficient. The purpose of this study was to evaluate the relationships between the occurrence of intraoperative periprosthetic fractures and both bone mineral density (BMD) and osteoporosis-related biomarkers.
Materials and Methods
This single-center retrospective study included a total of consecutive 487 hip joints of patients with a mean age of 65.5 ± 11.8 years who underwent total hip arthroplasty between July 2017 and December 2020. Patients with low BMD defined as T-score < -1.0 versus those with normal BMD were matched by a 1:1 propensity score to balance for patient baseline characteristics, and outcome was analyzed by a modified Poisson regression model. Our primary outcome was the incidence of intraoperative periprosthetic fracture during surgery. We also investigated the effect modification of osteoporosis–related biomarkers, including tartrate-resistant acid phosphatase 5b (TRACP-5b), total procollagen type 1 amino-terminal propeptide (total P1-NP), intact parathyroid hormone (intact PTH), and homocysteine, on osteoporosis and outcomes.
Results
After matching, 250 patients were analyzed. The risk of fracture was significantly higher in patients with low BMD than in normal BMD patients (Incidence rate ratio 5.00 [95% CI 1.11–22.43], p = 0.036). We also observed significant effect of high serum homocysteine on the occurrence of intraoperative fractures (Incidence rate ratio 8.38 × 106 [95% C; 3.44 × 106–2.01 × 107], p < 0.01).
Conclusion
Preoperative osteoporosis and high serum homocysteine levels were risk factors for intraoperative periprosthetic fractures.
Level of evidence
III, A single-center retrospective study.




Similar content being viewed by others
References
Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ (2009) Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res 467:2606–2612. https://doi.org/10.1007/s11999-009-0834-6
Della Rocca GJ, Leung KS, Pape HC (2011) Periprosthetic fractures: epidemiology and future projections. J Orthop Trauma 25(Suppl 2):S66-70. https://doi.org/10.1097/BOT.0b013e31821b8c28
Davidson D, Pike J, Garbuz D, Duncan CP, Masri BA (2008) Intraoperative periprosthetic fractures during total hip arthroplasty. Evaluation and management. J Bone Jt Surg Am 90:2000–2012. https://doi.org/10.2106/JBJS.H.00331
James SJ, Mirza SB, Culliford DJ, Taylor PA, Carr AJ, Arden NK (2014) Baseline bone mineral density and boneturnover in pre-operative hip and knee arthroplasty patients. Bone Joint Res 3:14–19. https://doi.org/10.1302/2046-3758.31.2000218
Lingard EA, Mitchell SY, Francis RM, Rawlings D, Peaston R, Birrell FN, McCaskie AW (2010) The prevalence of osteoporosis in patients with severe hip and knee osteoarthritis awaiting joint arthroplasty. Age Ageing 39:234–239. https://doi.org/10.1093/ageing/afp222
Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ (2009) The epidemiology of revision total hip arthroplasty in the United States. J Bone Jt Surg Am 91:128–133. https://doi.org/10.2106/JBJS.H.00155
Bernatz JT, Brooks AE, Squire MW, Illgen RI, Binkley NC, Anderson PA (2019) Osteoporosis Is common and undertreated prior to total joint arthroplasty. J Arthroplasty 34:1347–1353. https://doi.org/10.1016/j.arth.2019.03.044
Waqas K, Chen J, Koromani F, Trajanoska K, van der Eerden BC, Uitterlinden AG, Rivadeneira F, Zillikens MC (2020) Skin autofluorescence, a noninvasive biomarker for advanced glycation end-products, is associated with prevalent vertebral and major osteoporotic fractures: the Rotterdam Study. J Bone Miner Res 35:1904–1913. https://doi.org/10.1002/jbmr.4096
Behera J, Bala J, Nuru M, Tyagi SC, Tyagi N (2017) Homocysteine as a pathological biomarker for bone disease. J Cell Physiol 232:2704–2709. https://doi.org/10.1002/jcp.25693
Gerdhem P, Ivaska KK, Alatalo SL, Halleen JM, Hellman J, Isaksson A, Pettersson K, Väänänen HK, Akesson K, Obrant KJ (2004) Biochemical markers of bone metabolism and prediction of fracture in elderly women. J Bone Miner Res 19:386–393. https://doi.org/10.1359/JBMR.0301244
van Meurs JB, Dhonukshe-Rutten RA, Pluijm SM, van der Klift M, de Jonge R, Lindemans J, de Groot LC, Hofman A, Witteman JC, van Leeuwen JP, Breteler MM, Lips P, Pols HA, Uitterlinden AG (2004) Homocysteine levels and the risk of osteoporotic fracture. N Engl J Med 350:2033–2041. https://doi.org/10.1056/NEJMoa032546
Bigart KC, Nahhas CR, Ruzich GP, Culvern CN, Salzano MB, Della Valle CJ, Nam D (2020) Does femoral morphology predict the risk of periprosthetic fracture after cementless total hip arthroplasty? J Arthroplasty 35:S359–S363. https://doi.org/10.1016/j.arth.2020.02.048
Kanis JA, Melton LJ, Christiansen C, Johnston CC, Khaltaev N (1994) The diagnosis of osteoporosis. J Bone Miner Res 9:1137–1141. https://doi.org/10.1002/jbmr.5650090802
Takada R, Jinno T, Miyatake K, Hirao M, Kimura A, Koga D, Yagishita K, Okawa A (2018) Direct anterior versus anterolateral approach in one-stage supine total hip arthroplasty. Focused on nerve injury: A prospective, randomized, controlled trial. J Orthop Sci 23:783–787. https://doi.org/10.1016/j.jos.2018.05.005
Takada R, Jinno T, Miyatake K, Hirao M, Yagishita K, Yoshii T, Okawa A (2019) Supine versus lateral position for accurate positioning of acetabular cup in total hip arthroplasty using the modified Watson-Jones approach: a randomized single-blind controlled trial. Orthop Traumatol Surg Res 105:915–922. https://doi.org/10.1016/j.otsr.2019.05.004
Hoshino C, Koga D, Koyano G, Yamauchi Y, Sakai T, Okawa A, Jinno T (2019) Femoral nerve palsy following primary total hip arthroplasty with the direct anterior approach. PLoS ONE 14:e0217068. https://doi.org/10.1371/journal.pone.0217068
Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH (1993) Structural and cellular assessment of bone quality of proximal femur. Bone 14:231–242. https://doi.org/10.1016/8756-3282(93)90146-2
Khanuja HS, Vakil JJ, Goddard MS, Mont MA (2011) Cementless femoral fixation in total hip arthroplasty. J Bone Jt Surg Am 93:500–509. https://doi.org/10.2106/JBJS.J.00774
Stekhoven DJ, Bühlmann P (2012) MissForest–non-parametric missing value imputation for mixed-type data. Bioinformatics 28:112–118. https://doi.org/10.1093/bioinformatics/btr597
Rubin DB, Thomas N (1996) Matching using estimated propensity scores: relating theory to practice. Biometrics 52:249–264
Rubin DB (1997) Estimating causal effects from large data sets using propensity scores. Ann Intern Med 127:757–763. https://doi.org/10.7326/0003-4819-127-8_part_2-199710151-00064
Austin PC (2009) Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 28:3083–3107. https://doi.org/10.1002/sim.3697
Wade SW, Strader C, Fitzpatrick LA, Anthony MS, O’Malley CD (2014) Estimating prevalence of osteoporosis: examples from industrialized countries. Arch Osteoporos 9:182. https://doi.org/10.1007/s11657-014-0182-3
Liu B, Ma W, Li H, Wu T, Huo J, Han Y (2019) Incidence, classification, and risk factors for intraoperative periprosthetic femoral fractures in patients undergoing total hip arthroplasty with a single stem: a retrospective study. J Arthroplasty 34:1400–1411. https://doi.org/10.1016/j.arth.2019.03.031
Maier GS, Kolbow K, Lazovic D, Maus U (2016) The importance of bone mineral density in hip arthroplasty: results of a survey asking orthopaedic surgeons about their opinions and attitudes concerning osteoporosis and hip arthroplasty. Adv Orthop 2016:8079354. https://doi.org/10.1155/2016/8079354
Aro HT, Alm JJ, Moritz N, Mäkinen TJ, Lankinen P (2012) Low BMD affects initial stability and delays stem osseointegration in cementless total hip arthroplasty in women: a 2-year RSA study of 39 patients. Acta Orthop 83:107–114. https://doi.org/10.3109/17453674.2012.678798
Nixon M, Taylor G, Sheldon P, Iqbal SJ, Harper W (2007) Does bone quality predict loosening of cemented total hip replacements? J Bone Jt Surg Br 89:1303–1308. https://doi.org/10.1302/0301-620X.89B10.19038
Franklin J, Malchau H (2007) Risk factors for periprosthetic femoral fracture. Injury 38:655–660. https://doi.org/10.1016/j.injury.2007.02.049
Nakaya R, Takao M, Hamada H, Sakai T, Sugano N (2019) Reproducibility of the Dorr classification and its quantitative indices on plain radiographs. Orthop Traumatol Surg Res 105:17–21. https://doi.org/10.1016/j.otsr.2018.11.008
Blouin S, Thaler HW, Korninger C, Schmid R, Hofstaetter JG, Zoehrer R, Phipps R, Klaushofer K, Roschger P, Paschalis EP (2009) Bone matrix quality and plasma homocysteine levels. Bone 44:959–964. https://doi.org/10.1016/j.bone.2008.12.023
Herrmann M, Wildemann B, Claes L, Klohs S, Ohnmacht M, Taban-Shomal O, Hübner U, Pexa A, Umanskaya N, Herrmann W (2007) Experimental hyperhomocysteinemia reduces bone quality in rats. Clin Chem 53:1455–1461. https://doi.org/10.1373/clinchem.2007.086272
Weinstein AM, Rome BN, Reichmann WM, Collins JE, Burbine SA, Thornhill TS, Wright J, Katz JN, Losina E (2013) Estimating the burden of total knee replacement in the United States. J Bone Jt Surg Am 95:385–392. https://doi.org/10.2106/JBJS.L.00206
Rodan GA, Reszka AA (2003) Osteoporosis and bisphosphonates. J Bone Jt Surg Am 85-A Suppl:8–12
Bouxsein ML, Chen P, Glass EV, Kallmes DF, Delmas PD, Mitlak BH (2009) Teriparatide and raloxifene reduce the risk of new adjacent vertebral fractures in postmenopausal women with osteoporosis. Results from two randomized controlled trials. J Bone Joint Surg Am 91:1329–1338. https://doi.org/10.2106/JBJS.H.01030
Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, Delmas P, Zoog HB, Austin M, Wang A, Kutilek S, Adami S, Zanchetta J, Libanati C, Siddhanti S, Christiansen C, Trial F (2009) Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 361:756–765. https://doi.org/10.1056/NEJMoa0809493
Sato Y, Honda Y, Iwamoto J, Kanoko T, Satoh K (2005) Effect of folate and mecobalamin on hip fractures in patients with stroke: a randomized controlled trial. JAMA 293:1082–1088. https://doi.org/10.1001/jama.293.9.1082
Lindberg-Larsen M, Jørgensen CC, Solgaard S, Kjersgaard AG, Kehlet H, Replacement LFCfF-tHaK (2017) Increased risk of intraoperative and early postoperative periprosthetic femoral fracture with uncemented stems. Acta Orthop 88:390–394. https://doi.org/10.1080/17453674.2017.1302908
Joffe MM, Rosenbaum PR (1999) Invited commentary: propensity scores. Am J Epidemiol 150:327–333. https://doi.org/10.1093/oxfordjournals.aje.a010011
Acknowledgements
We thank Ms. Ellen Roider for English editing.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
NW and TO designed the study, performed data collection, analysis, and interpretation, and drafted the manuscript. KM, RT, YA, and JT contributed to the study design and data interpretation. HK and TY contributed to restructuring the article. AO contributed to the study design and data interpretation. All authors approved the final article.
Corresponding author
Ethics declarations
Conflict of interest
Naoto Watanabe, Takahisa Ogawa, Ryohei Takada, Yusuke Amano, Tetsuya Jinno, Hideyuki Koga, Toshitaka Yoshii, Atsushi Okawa, and Kazumasa Miyatake declare that they have no conflict of interest.
Ethics approval
This study was approved by the Medical Research Ethics Committee of Tokyo Medical and Dental University,
Patient confidentiality and consent for publication
All study subjects provided informed consent and consented to publication. The study protocol conformed to the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
402_2023_4989_MOESM1_ESM.pptx
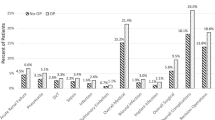
Supplementary Table 1. The baseline characteristics with missing values. DDH: Developmental dysplasia of the hip. OA: Osteoarthritis. ION: Idiopathic osteonecrosis of the femoral head. SIF: Subchondral insufficiency fracture. RDC: Rapidly destructive coxarthropathy. ALS: modified Watson-Jones supine approach. ALA: modified Watson-Jones lateral Approach. PLA: Posterolateral approach. DAA: Direct anterior approach
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Watanabe, N., Ogawa, T., Takada, R. et al. Association of osteoporosis and high serum homocysteine levels with intraoperative periprosthetic fracture during total hip arthroplasty: a propensity-score matching analysis. Arch Orthop Trauma Surg 143, 7219–7227 (2023). https://doi.org/10.1007/s00402-023-04989-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04989-6