Abstract
Introduction
Open diaphyseal tibial fractures are the most common long-bone fractures and require a rapid approach to prevent devastating complications. Current literature reports the outcomes of open tibial fractures. However, there is no robust, up-to-date research on the predictive indicators of infection severity in a large open tibial fracture patient cohort. This study investigated the predictive factors of superficial infections and osteomyelitis in open tibial fractures.
Materials and methods
A retrospective analysis of the tibial fracture database was carried out from 2014 to 2020. Criteria for inclusion was any tibial fracture including tibial plateau, shaft, pilon or ankle, with an open wound at the fracture site. Exclusion criteria included patients with a follow-up period of less than 12 months and who are deceased. A total of 235 patients were included in our study, of which 154 (65.6%), 42 (17.9%), and 39 (16.6%) developed no infection, superficial infection, or osteomyelitis, respectively. Patient demographics, injury characteristics, fracture characteristics, infection status and management details were collected for all patients.
Results
On multivariate modelling, patients with BMI > 30 (OR = 2.078, 95%CI [1.145–6.317], p = 0.025), Gustilo-Anderson (GA) type III (OR = 6.120, 95%CI [1.995–18.767], p = 0.001), longer time to soft tissue cover (p = 0.006) were more likely to develop a superficial infection, and patients with wound contamination (OR = 3.152, 95%CI [1.079–9.207], p = 0.036), GA-3 (OR = 3.387,95%CI [1.103–10.405], p = 0.026), longer to soft tissue cover (p = 0.007) were more likely to develop osteomyelitis.
Univariate analysis also determined that risk factors for superficial infection were: BMI > 35 (OR = 6.107, 95%CI [2.283–16.332], p = 0.003) and wound contamination (OR = 2.249, 95%CI [1.015–5.135], p = 0.047); whilst currently smoking (OR = 2.298, 95%CI [1.087–4.856], p = 0.025), polytrauma (OR = 3.212, 95%CI [1.556–6.629], p = 0.001), longer time to definitive fixation (p = 0.023) were for osteomyelitis. However, none of these reached significance in multivariate analysis.
Conclusion
Higher GA classification is a significant risk factor for developing superficial infection and osteomyelitis, with a stronger association with osteomyelitis, especially GA 3C fractures. Predictors for superficial infection included BMI and time to soft tissue closure. Time to definitive fixation, time to soft tissue closure, and wound contamination were associated with osteomyelitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Long bone fractures occur at a frequency of 11.5 per 100,000 person-years, with open tibial diaphysis fractures being the most common [1, 2]. 24% of all tibial fractures are open [1, 3]. Tibial fractures have a higher risk of being open than other long bones due to the limited soft tissue surrounding the tibia [1, 2]. These fractures typically occur bimodally: young males sustain high-impact injuries, and the elderly sustain low-energy fragility fractures [4]. The Gustilo-Anderson (GA) classification is widely used to classify open tibial fractures, with 3C fractures being the most severe and requiring vascular involvement [5, 6]. Open tibial fractures have surgical challenges due to poor soft tissue coverage, bone defects and high contamination risk [6]. This high contamination risk can lead to the development of osteomyelitis, with reports of open tibial fracture infection rates being as high as 29% [7,8,9,10]. Furthermore, the development of osteomyelitis will impose additional challenges and causes devastating consequences, including non-union, osteonecrosis, and amputation. Various other complications have also been reported in the literature [11,12,13,14].
Open long bone fractures are an orthopaedic emergency as they have catastrophic consequences if not managed rapidly and effectively [15,16,17]. Acute management is according to the British Orthopaedic Association Standards for Trauma and Orthopaedics (BOAST) 4 criteria, a collaboration between the British Association of Plastic, Reconstructive and Aesthetic Surgeons (BAPRAS) and BOAST [18]. General management principles include a timely multi-disciplinary approach, rapid administration of intravenous prophylactic antibiotics, realignment and splinting of the limb, meticulous wound debridement and soft tissue cover within 72 h after injury [18].
Current reports discuss the epidemiology of open tibial fractures, and they have investigated the short and long-term outcomes of post-traumatic open tibial fractures [2, 12]. However, there has yet to be an up-to-date robust report on the prognostic indicators of infection severity from a large cohort of open tibial fractures.
In this study, we sought to answer:
-
(1)
What is the current incidence of the development of superficial infection to deep infections in open tibial fractures?
-
(2)
Are patient and fracture characteristics predictive of superficial and deep infections in open tibial fractures?
-
(3)
Are environmental and temporal factors predictive of superficial and deep infections in open tibial fractures?
Methods
Patient cohort
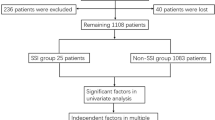
A retrospective analysis of the Epic systemsTM database at a single trauma centre was carried out from September 2014 to September 2020. The inclusion criteria were any patient with a tibia fracture, including the tibial plateau, shaft, pilon or ankle, with an open wound at the fracture site. Exclusion criteria were any patients that had a follow-up of fewer than 12 months or were deceased. This yielded 268 open tibial fractures from a major trauma centre database. Three patients were transferred to other hospitals for treatment after admission to the emergency department. Eighteen patients had incomplete notes or were lost to follow-up, and twelve patients passed away within a month of injury due to complications from the original injury trauma. A total of 235 patients were included in our study, of which 159 (65.6%), 45 (17.9%), and 39 (16.6%) had no infection, superficial infection, or osteomyelitis, respectively.
Definitions and coding
Patients were grouped according to infection outcomes. Superficial infection was defined as cellulitis over the fracture site, soft tissue abscesses, or positive microbiology samples from the tissue around the injury site, in addition to clinical signs of infection. Osteomyelitis was defined as clinical or radiological signs of osteomyelitis, in addition to positive bone debridement microbiology samples on debridement, infective non-union, infective bone loss or infective malunion or infected metalwork. Patients that did not fit the criteria above were classified as having “no infection”.
Mode of injury was classified into broad categories: falls, road traffic accidents, and crushes (including struck-by-a vehicle and pedestrian accidents). Definitive fixation was defined as the final operation to fix the fracture, including open reduction internal fixation (ORIF), external fixation (fine wire or with pins, FWF), non-operative joint fusion and amputation. The time to definitive soft tissue cover was defined as the time from admission to when the most thorough final soft tissue cover was achieved. Soft tissue cover included wound dressing (saline-soaked gauze), vacuum-assisted closure, skin graft and skin flap.
Data collection
Patient, fracture, and wound characteristics were collected for all included patients, and management details and infection outcomes were also included. Patient characteristics included age, gender, smoking status, diabetic status and body mass index (BMI). Fracture characteristics included injury mode, time of injury, presence of polytrauma, fibula fracture status, and GA classification. Wound characteristics included wound contamination. Management details included time to the first procedure, time to definitive soft tissue cover, time to definitive fixation and type of definitive fixation. Infection status was collected according to our definition above, and then patients were grouped into no infection, superficial infection and osteomyelitis.
Data analysis
Statistical analysis was performed by univariate analysis and multicollinearity diagnostics, followed by multivariate model generation, with PSS v28.0 being used. Univariate analysis was conducted with odds ratios for binary categorical independent variables, and bivariate regression for continuous independent variables for both non-infection versus superficial infection, as well as non-infection versus osteomyelitis.
A cut-off of p < 0.2 was used to determine which independent variables in the univariable calculations to include in the multivariable modelling, for both “no infection vs superficial infection” and “no infection vs osteomyelitis” comparisons. Each variable for inclusion in the multivariate model had its variance inflation factor (VIF) checked, to ensure there was no strong multicollinearity between the independent variables that could impact the validity of the multivariate model. A cut-off of VIF > 5 was used to exclude variables.
Multivariable analysis was performed to elucidate which variables were significant for “non infection vs superficial infection” and “non infection vs osteomyelitis”, with p < 0.05 considered statistically significant.
For categorical variables with more than two possible groups, a combination strategy was performed to achieve clinically relevant groupings for odds ratio computations, e.g. for smoking (current smoker comparison: ‘never smoked + ex-smoker vs smoker, have ever smoked comparison: never smoked vs ‘ex-smoker + current smoker’).
For continuous variables, the entire range was divided into groups when appropriate, e.g. for age, a cut-off of 60 years was used, and for BMI, the clinical designations of classes (normal weight, overweight, obese) were used. For time to procedures, no obvious cut-offs or groupings were available, so they were only analysed directly in the multivariate model.
Results
Patients and injury characteristics
The demographic data breakdown of all three infection groups is shown in Table 1.
Predictors of osteomyelitis, superficial infection, and no infection
Patients who had GA type III fractures, wound contamination, longer time to soft tissue cover, and BMI over 30, especially if over 35, were significantly more likely to develop a superficial infection (Table 2). Patients with GA type III, wound contamination, polytrauma, longer time to soft tissue cover, longer time to definitive fixation, or currently smoking are more likely to develop osteomyelitis (Table 3).
A threshold of p < 0.2 was used to determine which variables from univariate analysis would be considered for inclusion in the multivariate model. After multicollinearity diagnostics for both models, none of the remaining variables was excluded, as the VIF did not reach 5 for any of them. The multivariate models for superficial infection and osteomyelitis are displayed in Tables 4 and 5, respectively.
On multivariate modelling, patients with BMI > 30, GA type III, and longer time to soft tissue cover were more likely to develop a superficial infection. Patients with wound contamination at injury, GA type III and longer time to soft tissue cover were more likely to develop osteomyelitis.
Discussion
This study involved a large-scale analysis of risk factors for infection severity in open tibia fractures. Infections were stratified into superficial infection and osteomyelitis, and we found that BMI was associated with superficial infection, whilst time to definitive fixation, time to definitive soft tissue cover, and wound contamination was associated with osteomyelitis. GA classification was associated with both superficial infection and osteomyelitis, with more severe forms having a stronger association with osteomyelitis.
Early debridement of open tibia fractures
The ideal treatment protocol for open tibia fractures is still controversial, however, all agree upon the need for irrigation and debridement [19,20,21]. Some studies, for example, Pollak et al. have reported no correlation between time of care, including debridement and rate of infections or infection severity [22, 23]. However, if they were admitted within 6 h post-injury, they had a lower infection rate [23]. This is supported by a historic precedent/ evidence of a ‘6-h’ window that debridement must be performed within. However, this is largely unsubstantiated [24,25,26], as only one study with 47 open tibia fractures concluded that surgical debridement within 5 h was associated with fewer infections [27]. However, they did not consider that their cohorts had different injury severity. Some studies have also suggested that earlier debridement leads to worse outcomes. However, these were biased toward treating the most severe cases earliest [28]. Contamination load and overall bacterial growth time are important determinants of infection severity. For example, caseating necrotic wound diameter grows steadily within hours of bacterial contamination, with virulent strains leading to a more rapid increase in bacterial count, especially in deep wounds with low oxygen partial pressures and in areas with poor blood supply like the tibia [29]. After adjusting for confounding factors such as fracture type and injury grade, our cohort showed that the time to definitive soft tissue cover and definitive fixation was associated with the risk of developing osteomyelitis, suggesting the importance of timely management of open tibia fractures. Given the fact that it is unethical to randomise patients with severe trauma based on time to treatment, prospective cohort-style studies may still be the most practical in investigating the relationship between time to treatment and outcomes.
Correlation of Gustilo-Anderson classification to infection and poorer outcomes
Our study utilised the Gustilo-Anderson classification for open tibia fractures, despite one study reporting an average interobserver agreement of 60% [30]. The original classification system by Gustilo did not subdivide type III fractures. However, this was eventually amended after Gustilo et al. realised that the incidence of complications could not be accurately determined [31]. Gaebler et al. suggested that type III GA fractures led to a higher chance of deep infection. Nevertheless, only 43.3% of their patients had open fractures, and they did not subdivide the type III fractures, which limits the usefulness of their results in open tibia fracture research [32]. Schemitsch et al. reported many risk factors associated with poorer prognosis after intramedullary nailing of open tibia fractures, such as whether or not the nail was reamed. However, they failed to include GA classification in their analysis and simply excluded type IIIc open fractures [33]. Our study found a significant relationship between GA classification and infection severity, which agrees with many retrospective cohort studies in the literature. Harley et al. determined that a strong predictor for infection was GA type (type I had a 2% rate; type III had a 22% rate) [34]. However, studies like these are confounded by the significant number of comorbidities in open tibia fracture patients, such as diabetes, intra-operative factors such as blood loss and operative time, as well as external factors such as tobacco and alcohol use, all of which can influence functional and clinical outcomes [17, 35]. Furthermore, the type of definitive fixation performed on open tibial fracture patients, namely intramedullary nails (IMN), screws and plating, or external fixation with frames, has an impact on rates of infection as well as overall complication rates [36]. The patient data we received showed predominantly IMNs for definitive fixation, which could explain our lower infection rates when compared to the literature. IMNs fixation has been associated with superior post-operative outcomes and is the preferred mode of definitive internal fixation amongst trauma surgeons [37, 38].
Correlation between body habitus and infection
BMI was found to be associated with superficial infections but not osteomyelitis. In a national prospective cohort study involving 159,720 patients, obesity was linked to a 1.1–4.4 fold increase in developing a superficial infection compared with normal weight [39]. The reasons for this are multifactorial. Obesity is associated with a chronic inflammatory state, and metabolic factors such as increased insulin resistance and hyperglycaemia that are characteristic of obese patients could render patients susceptible to infections [40]. Obese patients could have different injury patterns after blunt and severe trauma [41], coupled with prolonged recovery and immobility after trauma. They are more likely to have central lines inserted for longer periods of time due to difficulty with peripheral venous access [42]. Furthermore, mechanical factors can increase the superficial infection rate. These include increased local surgical site trauma due to increased tissue retraction and adipose tissue content; prolonged operative times; and decreased perioperative tissue oxygenation [43].
Deep infections vs osteomyelitis
The literature is currently unclear on the definition of osteomyelitis and what is necessary for its diagnosis. Most papers have a variety of criteria and require one or more criteria to be met. These criteria can include signs on imaging [44,45,46,47]; positive cultures or histology from bone biopsies or debridement [46,47,48]; or sinuses or abscesses during surgery [44,45,46]. The emphasis on which of these findings is essential vs optional varies by paper. We, therefore, decided to use a definition which was based on the majority of papers we read which supported that microbiological results are preferable [46,47,48].
Limitations
Being a retrospective observational study, we relied upon the accuracy of patient’s notes and attendance at follow-up clinics. The single-centre nature of the study also can restrict the scope of patients treated. However, being a major trauma centre with a dedicated bone infection team means that there will be good variation and diversity of patients and they are unlikely to be followed up in other settings. This, combined with the wide range of patient factors studied and the long-time frame investigated enhances the external validity of our results. With traumatic injury cases, investigating fixation methods in a prospective manner, negating the impact of the specific situation and surgeons’ experiences, can be difficult to justify ethically and implement. Nevertheless, future studies involving multiple centres could further elucidate underlying factors for infection.
In our study, we grouped various anatomical locations of tibial fractures, such as ankle, plateau, pilon and shaft, together into the same cohort. While there is inherent heterogeneity within this group, we feel that for open fractures specifically, this is justified given the underlying mechanisms of infection (e.g. wound contamination, vasculature and subsequent post-injury compromise, and delay in wound closure) are quite similar within that specific area of the lower limb.
Lastly, we classified fractures by GA type, rather than by AO classification. We felt this was appropriate given the degree of soft tissue damage is a stronger predictor of infective processes at the time of injury, rather than the degree of comminution or articular involvement. Furthermore, with AO classification more commonly used in research activities rather than clinical practice, we feel that the GA type is more suitable for clinicians when risk stratifying at the time of injury.
Conclusion
Open tibial fractures are the most common open long bone fractures and are notorious for developing infections during rehabilitation. Our study demonstrated GA classification is a significant indicator for both superficial infection and deep infection, with a stronger association with osteomyelitis, especially GA IIIC fractures. Other predictors for superficial infections included BMI and type of definitive fixation. Furthermore, time to definitive fixation, type of definitive fixation, time to definitive soft tissue cover, and wound contamination was associated with osteomyelitis. As FWF is typically used for patients with more complex fractures, they have a significantly increased chance of osteomyelitis and superficial infection compared to those with ORIF for definitive fixation. Patients who undergo ORIF tend to have faster definitive soft tissue closure and reduced contact with the external environment from metalwork. However, determining the definitive fixation method is difficult to do validly and ethically, and thus we recommend surgeons employ their own expertise in the area combined with the risk stratification of other factors reported in our study. Furthermore, it is pertinent that the BOAST 4 guidelines are followed and practitioners provide rapid intravenous prophylactic antibiotics to patients with wound contamination, a history of smoking or increased BMI to decrease the risk of developing infection.
References
Court-Brown CM, Caesar B (2006) Epidemiology of adult fractures: a review. Injury 37(8):691–697
Weber CD, Hildebrand F, Kobbe P, Lefering R, Sellei RM, Pape H-C et al (2019) Epidemiology of open tibia fractures in a population-based database: update on current risk factors and clinical implications. Eur J Trauma Emerg Surg 45(3):445–453
Hundal RS, Weick J, Hake M (2021) Management of open segmental tibial fractures. J Orthop Trauma 35:S50
Lee A, Geoghegan L, Nolan G, Cooper K, Super J, Pearse M et al (2022) Open tibia/fibula in the elderly: a retrospective cohort study. JPRAS Open 1(31):1–9
Kim PH, Leopold SS (2012) Gustilo-Anderson classification. Clin Orthop Relat Res 470(11):3270–3274
Cross WW, Swiontkowski MF (2008) Treatment principles in the management of open fractures. Indian J Orthop 42(4):377–386
Griffin M, Malahias M, Khan W, Hindocha S (2012) Update on the management of open lower limb fractures. Open Orthop J 30(6):571–577
Griffin M, Malahias M, Hindocha S, Khan W (2012) Update on the management of compound lower limb fractures. Open Orthop J 30(6):518–524
Yusof NM, Khalid KA, Zulkifly AH, Zakaria Z, Amin MAM, Awang MS et al (2013) Factors associated with the outcome of open tibial fractures. Malays J Med Sci 20(5):47–53
Rajasekaran S, Babu JN, Dheenadhayalan J, Shetty AP, Sundararajan SR, Kumar M et al (2006) A score for predicting salvage and outcome in Gustilo type-IIIA and type-IIIB open tibial fractures. J Bone Jt Surg Br Vol 88(10):1351–1360
Munir MA, Tandiabang PA, Prihantono (2020) Internal fixation of delayed union of fracture with chronic osteomyelitis due to Staphylococcus epidermidis: a case report. Ann Med Surg (Lond) 56:56–60
Momodu II, Savaliya V (2022) Osteomyelitis. StatPearls [Internet]. StatPearls Publishing, Treasure Island
Feldman V, Segal D, Atzmon R, Ron I, Nyska M, Ohana N et al (2021) Amputation versus primary nonoperative management of chronic osteomyelitis involving a pedal digit in diabetic patients. J Am Podiatr Med Assoc 111(4):2
Faglia E, Clerici G, Caminiti M, Curci V, Somalvico F (2013) Influence of osteomyelitis location in the foot of diabetic patients with transtibial amputation. Foot Ankle Int 34(2):222–227
Ford AN, Harkin EA, Lyons MM, Summers HD, Hecht GG, Lack WD et al (2021) Clinical and radiographic predictors of nonunion in open tibial shaft fractures. Orthopedics 44(3):142–147
Border JR (1995) Death from severe trauma: open fractures to multiple organ dysfunction syndrome. J Trauma 39(1):12–22
Dickson DR, Moulder E, Hadland Y, Giannoudis PV, Sharma HK (2015) Grade 3 open tibial shaft fractures treated with a circular frame, functional outcome and systematic review of the literature. Injury 46(4):751–758
. BOA (2021) BOAST-open fractures [Internet]. https://www.boa.ac.uk/resources/boast-4-pdf.html. Accessed 15 Aug 2021
Gustilo RB, Anderson JT (1976) Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Jnt Surg Am 58(4):453–458
Byrd HS, Spicer TE, Cierney G (1985) Management of open tibial fractures. Plast Reconstr Surg 76(5):719–730
Gregory P, Sanders R (1995) The management of severe fractures of the lower extremities. Clin Orthop Relat Res 318:95–105
Yokoyama K, Itoman M, Shindo M, Kai H (1995) Contributing factors influencing type III open tibial fractures. J Trauma 38(5):788–793
Pollak AN, Jones AL, Castillo RC, Bosse MJ, MacKenzie EJ, LEAP Study Group (2010) The relationship between time to surgical debridement and incidence of infection after open high-energy lower extremity trauma. J Bone Jt Surg Am 92(1):7–15
Crowley DJ, Kanakaris NK, Giannoudis PV (2007) Irrigation of the wounds in open fractures. J Bone Jnt Surg Br 89(5):580–585
Khatod M, Botte MJ, Hoyt DB, Meyer RS, Smith JM, Akeson WH (2003) Outcomes in open tibia fractures: relationship between delay in treatment and infection. J Trauma 55(5):949–954
Webb LX, Bosse MJ, Castillo RC, MacKenzie EJ, LEAP Study Group (2007) Analysis of surgeon-controlled variables in the treatment of limb-threatening type-III open tibial diaphyseal fractures. J Bone Jt Surg Am 89(5):923–928
Kindsfater K, Jonassen EA (1995) Osteomyelitis in grade II and III open tibia fractures with late debridement. J Orthop Trauma 9(2):121–127
Okike K, Bhattacharyya T (2006) Trends in the management of open fractures. A critical analysis. J Bone Jt Surg Am 88(12):2739–2748
Hunt TK (1981) Surgical wound infections: an overview. Am J Med 70(3):712–718
Brumback RJ, Jones AL (1994) Interobserver agreement in the classification of open fractures of the tibia. The results of a survey of two hundred and forty-five orthopaedic surgeons. J Bone Jt Surg Am 76(8):1162–1166
Gustilo RB, Mendoza RM, Williams DN (1984) Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma 24(8):742–746
Gaebler C, Berger U, Schandelmaier P, Greitbauer M, Schauwecker HH, Applegate B et al (2001) Rates and odds ratios for complications in closed and open tibial fractures treated with unreamed, small diameter tibial nails: a multicenter analysis of 467 cases. J Orthop Trauma 15(6):415–423
Schemitsch EH, Bhandari M, Guyatt G, Sanders DW, Swiontkowski M, Tornetta P et al (2012) Prognostic factors for predicting outcomes after intramedullary nailing of the tibia. J Bone Jt Surg Am 94(19):1786–1793
Harley BJ, Beaupre LA, Jones CA, Dulai SK, Weber DW (2002) The effect of time to definitive treatment on the rate of nonunion and infection in open fractures. J Orthop Trauma 16(7):484–490
Nyquist F, Berglund M, Nilsson BE, Obrant KJ (1997) Nature and healing of tibial shaft fractures in alcohol abusers. Alcohol Alcohol 32(1):91–95
Vallier HA, Le TT, Bedi A (2008) Radiographic and clinical comparisons of distal tibia shaft fractures (4 to 11 cm proximal to the plafond): plating versus intramedullary nailing. J Orthop Trauma 22(5):307–311
Tu YK, Lin CH, Su JI, Hsu DT, Chen RJ (1995) Unreamed interlocking nail versus external fixator for open type III tibia fractures. J Trauma 39(2):361–367
Henley MB, Chapman JR, Agel J, Harvey EJ, Whorton AM, Swiontkowski MF (1998) Treatment of type II, IIIA, and IIIB open fractures of the tibial shaft: a prospective comparison of unreamed interlocking intramedullary nails and half-pin external fixators. J Orthop Trauma 12(1):1–7
Thelwall S, Harrington P, Sheridan E, Lamagni T (2015) Impact of obesity on the risk of wound infection following surgery: results from a nationwide prospective multicentre cohort study in England. Clin Microbiol Infect 21(11):1008.e1–8
Czupryniak L, Strzelczyk J, Pawlowski M, Loba J (2004) Mild elevation of fasting plasma glucose is a strong risk factor for postoperative complications in gastric bypass patients. Obes Surg 14(10):1393–1397
Boulanger BR, Milzman D, Mitchell K, Rodriguez A (1992) Body habitus as a predictor of injury pattern after blunt trauma. J Trauma 33(2):228–232
El-Solh A, Sikka P, Bozkanat E, Jaafar W, Davies J (2001) Morbid obesity in the medical ICU. Chest 120(6):1989–1997
Kabon B, Nagele A, Reddy D, Eagon C, Fleshman JW, Sessler DI et al (2004) Obesity decreases perioperative tissue oxygenation. Anesthesiology 100(2):274–280
Wang C, Li Y, Huang L et al (2010) Comparison of two-staged ORIF and limited internal fixation with external fixator for closed tibial plafond fractures. Arch Orthop Trauma Surg 130:1289–1297. https://doi.org/10.1007/s00402-010-1075-6
Cui X, Chen H, Rui Y, Niu Y, Li H (2018) Two-stage open reduction and internal fixation versus limited internal fixation combined with external fixation: a meta-analysis of postoperative complications in patients with severe Pilon fractures. J Int Med Res 46(7):2525–2536. https://doi.org/10.1177/0300060518776099
Sheehy SH, Atkins BA, Bejon P, Byren I, Wyllie D, Athanasou NA, Berendt AR, McNally MA (2010) The microbiology of chronic osteomyelitis: prevalence of resistance to common empirical anti-microbial regimens. J Infect 60(5):338–343. https://doi.org/10.1016/j.jinf.2010.03.006
CDC (2022) CDC/NHSN surveillance definitions for specific types of infections. https://www.cdc.gov/nhsn/pdfs/pscmanual/17pscnosinfdef_current.pdf. Accessed 25 May 2022
Kessler L, Piemont Y, Ortega F, Lesens O, Boeri C, Averous C, Meyer R, Hansmann Y, Christmann D, Gaudias J, Pinget M (2006) Comparison of microbiological results of needle puncture vs. superficial swab in infected diabetic foot ulcer with osteomyelitis. Diabet Med 23(1):99–102. https://doi.org/10.1111/j.1464-5491.2005.01764.x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest.
Ethical approval
Ethical approval was granted by the local ethics committee of our institution. This study received the project number 10219 on 15 December 2021.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, J., Lu, V., Zhou, A.K. et al. Predictors for infection severity for open tibial fractures: major trauma centre perspective. Arch Orthop Trauma Surg 143, 6579–6587 (2023). https://doi.org/10.1007/s00402-023-04956-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04956-1