Abstract
Introduction
Fractures of the proximal femur accompanied by a fracture of the femoral shaft are relatively rare, with a reported prevalence between 1 and 12%. Multiple surgical options are available, consisting of treatment with a single implant or with double implants. Controversy exists about the optimal management. A systematic review and pooled analysis were performed to assess the most reliable treatment for bifocal femoral fractures of the femur.
Materials and methods
A literature search was conducted on July 15, 2022. Selected studies were screened on title and abstract by two researchers independently, and full texts were read by both authors. Emphasis was put on adverse events such as postoperative infection, healing complications, malalignment, and functional outcome using either a single implant or double implants.
Results
For the proximal femoral fractures, no significant difference could be confirmed for avascular necrosis of the femoral neck (5.1% for single implant and 3.8% for double implants), nonunion (6.4% for single implant and 7.8% for double implants), or varus malalignment (6.6% for single implant and 10.9% for double implants). This study also suggests that the number of implants is irrelevant for complications of the femoral shaft regarding the rates of postoperative infection and healing complications. Pooled rates of bone healing complications were 1.6–2.7-fold higher when patients were treated with a single implant, but statistical significance could not be confirmed. For hardware failure, revision surgery, leg length discrepancy, and functional outcome, no difference between the two groups was found either.
Conclusions
The pooled proportions of all postoperative complications had overlapping confidence intervals; thus, no inference about a statistically significant difference on the number of implants used for treating ipsilateral fractures of the femur can be made. Both treatment groups showed a similar functional outcome at the last moment of follow-up, with more than 75% of the patients reporting a good outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bifocal fractures of the femur have first been reported in the early fifties [1, 2]. Fractures of the femoral neck or trochanteric fractures accompanied by a fracture of the femoral shaft are rare. The reported prevalence of these bifocal fractures ranges between 1 and 12% [3,4,5,6,7,8,9]. These injuries are usually the result of high-energy trauma (HET) and occur mostly in polytraumatized young adults [10]. AO-type A3, AO-type B, and AO-type C femoral shaft fracture patterns are more often part of a bifocal injury [11].
Due to the extent of trauma, femoral neck fractures are easily missed during the primary survey. Previous literature reports that up to 30% of femoral neck fractures are missed [10, 12], and increased awareness showed a decline in missed fractures [9, 13]. In bifocal fractures, the femoral shaft fracture is usually accompanied by a fracture of the femoral neck, but up to 28% is accompanied by a trochanteric fracture [11, 14, 15].
Besides diagnostic challenges, the management of bifocal fractures of the femur can be challenging as well. To regain function, anatomic reduction of the femoral neck fracture, restoring the length and alignment of the femoral shaft fracture, and create a stable osteosynthesis should be the goal of initial surgical management. Since the first reports various treatment options that are developed, literature reports up to 50 possible treatment options for bifocal fractures of the femur. These treatment modalities can be divided into two groups, namely management with a single implant or with a separate implant for each fracture, referred to as double implants. Treatment with a single implant allows the physician to treat both fractures with one single device showing various results [16,17,18,19,20,21,22]. The alternative is using separate implants for each fracture [9, 12, 23,24,25,26,27,28,29]. Several authors recommend to prioritize fixation of the femoral neck to prevent further risk of the blood supply of the femoral head [30, 31].
Controversy still exists about the optimal management of bifocal femur fractures. Using a single implant or double implants has shown good results, although mostly in small numbers [19, 20, 27, 32,33,34,35]. A systematic review and pooled analysis was performed to assess the outcome in bifocal fractures of the femur on adverse events such as postoperative infection, healing complications, malalignment, and functional outcome using either on the two types of treatment.
Materials and method
Literature search strategy
This systematic review with pooled analysis was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses criteria [36]. With the help of a biomedical information specialist, a literature search was completed on July 15, 2022. Embase, Medline Ovid, Cinahl, Web of Science, Cochrane, and Google scholar were used in the search. The databases were searched on terms related to “femoral shaft fractures” combined with “proximal femur fracture”, “femoral neck fracture” and their abbreviations and synonyms. The search strings used for each database are shown in Appendix 1 of the supplemental material.
Inclusion criteria were studies that described adult patients that were treated operatively for combined acute fractures of the femoral shaft and the proximal femur using either a single implant or with double implants. Fractures of the proximal femur included fractures of the femoral neck and trochanteric fractures. Studies that did not publish about primary treatment (e.g., treatment of delayed or nonunion) or studies that reported non-original data (e.g., systematic reviews or meta-analysis), case series, or biomechanical studies were excluded. Studies published before 2000 were excluded as well to remove the older generation of intramedullary nails; therefore, emphasis was put on most recent generations of intramedullary nails. Duplicate studies were removed.
First, selected studies were screened on title and abstract by two researchers independently (JDC and EMMVL). Second, full texts were read by both authors. In both screenings, a consensus was reached by discussion. When any inconsistencies remained after discussion, the third author (MHJV) was consulted. All inconsistencies were resolved by consensus. If a full text was not available, the corresponding author was contacted by the first author (JDC) by e-mail. Data from studies not published in English were extracted with the help of a narrative speaker of the language of the publication.
Data extraction
Data were extracted by two authors (JDC and EMMVL) independently, using a predefined data sheet. The following data were collected: (1) general information and demographic information (i.e., number of patients, number of fractures, sex, and age), (2) injury characteristics (i.e., trauma mechanism, associated injuries, and injury severity score), (3) treatment characteristics (i.e., operation time, blood loss during operation, number of patients treated with a single implant, and number of patients treated with a double implant), and (4) clinical outcome (i.e., adverse events, revision surgery, and functional outcome).
Patients treated with a single implant were considered a distinct group, and patients treated with a double implant were considered a distinct group. A single implant treatment was defined as one implant treating both injuries. In treatment with a double implant, each fracture is fixated with a separate device (e.g. cannulated hip screws or sliding hip screw for the femoral neck fracture and retrograde nailing for the femoral shaft fracture, or antegrade intramedullary nailing with cannulated hip screws).
Assessment of quality selected studies
The quality of each included study was assessed using the methodologic index for nonrandomized studies (MINORS), which is a validated instrument for nonrandomized surgical studies [37]. Seven items are selected for assessing non-comparative studies, and additionally five items are selected for assessing of comparative studies. Ideally non-comparative studies can score 16 points and comparative studies 24 points. Patients were stratified into a group with patients treated with a single implant for both fractures and a group with patients in whom the fractures were treated with a separate implant (double implant group). The quality of the studies is shown in Appendix 2 of the supplemental material.
Analysis
Data were analyzed using MedCalc Statistical Software version 18.2.1 (MedCalc Software bvba, Ostend, Belgium; http:/www.medcalc.org; 2018). Pooled estimates were reported with their 95% confidence intervals (CI). Cochran’s Q-test and the I2 were used to quantify the heterogeneity. For the pooled analysis, a fixed effects model was used when the I2 was lower than 40%, and a random effects model was used when the I2 was higher than 40%. For each outcome, forest plots and funnel plots were used to assess publication bias. The funnel plots showed no substantial anomalies that raised the suspicion of a publication bias. The forest plots of each outcome are shown in Appendix 3, and the funnel plots are shown in Appendix 4 of the supplemental material. Numeric data of the forest plots are shown in Tables 2, 3 and 4.
Results
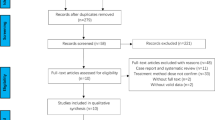
A total of 2530 studies were identified with the search strategy (Fig. 1). After de-duplication and screening the title and abstract of all records, 84 studies remained for full-text analysis. After assessing full text, 34 articles were excluded based on the exclusion criteria. In total, 50 articles (1310 patients) were included in the final analysis [3,4,5,6,7,8,9, 12, 18,19,20,21, 23,24,25,26,27,28,29, 32,33,34,35, 38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64]. There were six prospective studies and 44 retrospective articles. General data for all studies are presented in Table 1. The majority of the patients were male and sustained a concomitant fracture of the femur as result of high-energy trauma. Of the patients, 625 were treated with a single implant and 660 were treated with a double implant. Mean follow-up ranged from 12 to 78 months.
Operation time and perioperative blood loss
Only seven studies reported sufficient data concerning operation time and perioperative blood loss [19, 28, 49, 54, 59, 61, 62]. Table 2 shows the pooled analysis for operation time and perioperative blood loss for both treatment groups. It also shows the number of studies, the number of patients for which data were available, and the result of the heterogeneity test. The pooled operation time for single implants was 133 min. (95% CI 98–169 min.) versus 150 min. (95% CI 124–177 min.) for patients treated with a double implant [19, 28, 49, 54, 59, 61, 62]. The overlapping confidence intervals suggest that operation time is unrelated to the number of implants.
In the group treated with a single implant, pooled perioperative blood loss was 334 mL (95% CI 152–516 mL) compared to 373 mL (95% CI 233–512 mL) in patients treated with a double implant [19, 54, 59, 61, 62].
Adverse events of the femoral neck fractures
In patients treated with a single implant, postoperative infection was seen in 6.1% (95% CI 1.1–14.4%) of the patients (Table 3) [21, 38, 55]. Insufficient data were available concerning postoperative infection in patients treated with a double implant. Most avascular necrosis (AVN) was found in the single implant group with 5.1% (95% CI 2.8–8.5%) of the patients versus 3.8% (95% CI 1.5–7.2%) in patients treated with a double implant [4, 7, 9, 12, 18, 21, 25, 46, 49, 55, 59, 62, 63]. The overlapping confidence intervals do not suggest evidence of a difference between the type of treatment and the risk of AVN. Nonunion of the femur neck was noted in 6.4% (95% CI 3.9–9.4%) when treated with a single implant and in 8.2% (95% CI 5.3–11.6%) when treated with a separate device for each fracture [3,4,5, 7,8,9, 12, 18, 21, 25, 26, 28, 32, 33, 43, 45,46,47,48,49,50, 55, 56, 61]. Varus malunion was noted in 6.6% of the patients in the single implant group (95% CI 3.9–10.1%) and in 10.9% in the double implant group (95% CI 6.6–16.2%) [3,4,5, 7, 9, 21, 24,25,26,27, 38, 41, 42, 44, 46, 49, 52, 55, 57, 61, 63]. The pooled rates were higher for the double implant group but the overlapping confidence intervals suggest that nonunion and varus malunion of the femur neck are unrelated to the number of implants used.
Adverse events of the femoral shaft fractures
Higher rates of infection were found when treated with double implants 9.2% (95% CI 5.2–14.3%) versus 5.8% (95% CI 2.9–10.2%) when treated with a single implant [4, 21, 27, 28, 54, 55, 61, 62, 64]. The overlap in 95% confidence intervals does not suggest a superior treatment. In all bone healing-related complications, treatment with a single implant showed 1.6–2.7-fold higher pooled rates compared to patients treated with double implants, which is, respectively, 19.9% (95% CI 9.3–33.3%) in single implants versus 10.8% (95% CI 7.1–15.4%) in double implants for delayed union [4, 6, 7, 9, 21, 27, 38, 46, 49, 52, 53, 56, 61, 62, 64]. Nonunion was seen in 17.3% (95% CI 11.1–24.6%) in single implant versus 14.2% (95% CI 8.8–20.7%) in double implants [4, 5, 9, 12, 18, 20, 21, 23,24,25, 27, 29, 33, 34, 39, 43,44,45, 47, 50, 53,54,55,56,57,58, 60, 61, 63]. Malunion was seen in 17.5% (95% CI 4.9–35.7%) when treated with a single implant versus 6.4% (95% CI 1.3–15.0%) in patients treated with double implants [9, 20, 25, 26, 52, 57]. However, the overlapping confidence intervals showed no convincing evidence of a statistical difference between the two groups.
General adverse events
Hardware failure was noted in 11.4% (95% CI 4.9–20.2%) of patients treated with a single implant versus 9.9% (95% CI 4.9–17.5%) in patients treated with a double implant [4, 7, 20, 23, 24, 27, 42, 45, 46, 50, 53, 57]. The reoperation rate was 18.4% (95% CI 11.6–26.4%) versus 17.0% (95% CI 12.2–22.5%), respectively, for single implants and for double implants [3, 7, 9, 18,19,20,21, 24, 27, 32, 34, 38, 41, 42, 44, 45, 47, 49, 50, 53,54,55,56]. The overlapping confidence intervals suggested no relationship between these complications and the number of implants.
Functional outcome
Leg length discrepancy was found in 12.4% (95% CI 8.5–17.3%) of the patients treated with a single implant and in 8.8% (95% CI 2.9–17.4%) of the patients treated with a double implant [4, 7, 20, 27, 38, 44,45,46, 49, 50, 53, 55, 56] (Table 4).
The Friedman and Wyman criteria were used in most studies as a tool to measure the functional outcome [65]. Patients treated with a single implant showed a good outcome according to the Friedman and Wyman criteria in 75.9% (95% CI 67.2–83.6%) versus 77.0% (95% CI 70.9–82.6%) for patients treated with double implants [3, 5, 23,24,25, 27,28,29, 34, 35, 39, 40, 46,47,48,49,50, 53,54,55,56,57, 64]. Overlapping confidence intervals suggesting the number of implants are irrelevant to the functional outcome.
Discussion
Concomitant fractures of the proximal femur and the femoral shaft present a difficult management problem for the physician. Controversy exist about the number of implants that should be used and which fracture should be prioritized in stabilization. Therefore, a pooled analysis was conducted to analyze the effect of the number of implant used and the amount of adverse events and the functional outcome. This systematic review and pooled analysis found overlapping confidence intervals for complications after surgery for concomitant fractures of the femur. Regarding the femoral neck, no significant difference could be confirmed for postoperative infection, avascular necrosis of the femoral neck, nonunion, or varus malalignment. This study could not confirm the superiority of either single of double implant with respect to the risk of postoperative infection and healing complications. The same was true for hardware failure, revision surgery, leg length discrepancy, and functional outcome.
The primary goal of the treatment should be based on: (1) adequate anatomic reduction of the proximal femur fracture and the femoral shaft fracture; (2) restore alignment, length, and rotation of the femur; and (3) provide a stable construct for both fractures. Achieving this will reduce the risk of complications. Multiple combination implant options are available each with their own advantages. In the early nineties, the indication for the use of reconstruction nails extended to concomitant fractures of the femur with good results [66,67,68]. Some studies suggest that reconstruction nailing has the advantages of a minimal invasive technique, reduced blood loss, and shorter operation time [4, 25, 53, 54, 67]. This pooled analysis showed that this is not necessarily the case with single implants.
Well-known complications of treatment for proximal femur fractures are avascular necrosis, nonunion, and varus malunion. Reported rates of avascular necrosis of the neck range from 0 to 9% in the literature [9, 21, 30, 69]. The hypothesis is that higher rates of avascular necrosis in single implants are expected due to the displacement of the femoral neck when the antegrade nail is inserted [66, 69, 70]. This displacement when rodding the femoral nail could increase the risk of impairment of the blood circulation of the femoral head [31, 70, 71]. This raised the question on which fracture should be stabilized first. The current pooled analysis showed pooled proportions of 3.8% of avascular necrosis when treated with double implants and 5.1% of avascular necrosis of the femoral head when treated with a single implant, which are similar rates in patients with isolated femoral neck fractures [72,73,74].
This study showed comparable nonunion rates of the femoral neck in both treatment groups, respectively, 6.4% for the single implant group and 7.8% when treated with double implants. A prompt anatomic reduction is the best treatment to reduce nonunion rate. The union rate may decrease where the stability of the fixation has been jeopardized [26, 33, 75,76,77,78]. Watson et al. reported that 7 of 8 patients with femoral neck nonunion had significant varus malunion [79]. An accurate reduction is more often accomplished in patients treated with retrograde nailing for the shaft and a separate implant for the neck compared with a cephalomedullary device [26]. Another potential benefit of dual implants lies in the management of complications. The complications of shaft fractures can often be managed without taking out femoral neck fixation when patients are treated with separate devices.
Although the pooled proportions were determined per treatment group and the overlap in confidence intervals, for avascular, necrosis and nonunion does not confirm superiority of either one of the treatment options, the authors prefer to prioritize the neck fracture since avascular necrosis or inadequate reduction can lead to devastation outcome in this relative young population.
Shaft complications
This pooled analysis showed 1.6–2.7-fold higher pooled proportions of healing complications in the patients treated with a single implant for both fractures; however, the overlapping confidence intervals suggesting the number of implants are irrelevant to bone-healing complications. The rate of shaft complications in bifocal fractures is higher than in isolated femoral shaft fractures; this could be explained by the larger amount of energy which is transferred trough the femur during trauma. [3, 4, 7, 33, 45, 49]. Compared with isolated femoral shaft fractures, higher rates of healing complications in bifocal fractures are reported for the femoral shaft [80,81,82,83,84,85]. In the data of this study, we could not derive any contributing factors to nonunion of the femoral shaft, mostly to the lack of studies reporting injury characteristics (such as open fractures) or postoperative instructions. Postoperative factors such as type of implant (especially the type of generation implant), or postoperative weight bearing could be a contributing factor to nonunion. In the studies in this pooled analysis, no difference was observed in the type of implant used, especially the generation of the implants, in nonunion. For postoperative weight bearing, more research is needed, only a few studies reported on postoperative weight bearing after the treatment on bifocal femoral fractures. Previous studies did show factors contributing to nonunion of the femoral shaft; open shaft fractures, unreamed nails, malreduction, prolonged weight bearing, and the use of reconstruction nails [26, 79]. This could explain the higher rates of healing complications for the shaft, but more data are needed as nonunion is the major concern in these types of fractures.
Functional outcome
The functional outcome after concomitant fractures of the proximal femoral and the femoral shaft is good in the majority of patients. This study showed that 75.9% of the patients treated with a single implant showed a good score on the Friedman and Wyman score versus 77.0% for the group treated with double implants. Although frequently used as an instrument to report functional outcome, the Friedman and Wyman score is a non-validated tool to assess functional outcome. However, in other (non-)validated instruments, the functional outcome appears to be good as well [6, 7, 19, 20, 44, 50, 59, 86,87,88].
Limitations
This study has several limitations, which warrants careful interpretation of the findings. First, almost only retrospective studies were included. No randomized controlled trials were retrieved with this search string. Because of the large amount of case series, a comparative meta-analysis between the two groups was impossible; thus, a pooled analysis was conducted. Second, relatively small numbers of studies on certain outcomes were published and the continuous data were not always provided (range, mean, standard deviation, or number of patients). This gives insufficient data in certain domains. Despite these limitations, the strength of this study is the high number of studies included in the analysis (providing data of 50 studies and 1310 patients).
Conclusion
This systematic review and pooled analysis showed that treatment with a single implant and double implant is both suitable options for concomitant fractures of the proximal femur and femur shaft. However, 1.6–2.7-fold higher pooled proportions of healing complications in patients treated with a single implant treating both fractures were observed. All pooled proportions had overlapping confidence intervals, suggesting that currently available data do not confirm a statistically significant association between postoperative complications and the number of implants used for treating ipsilateral fractures of the femur. Both treatment groups showed similar functional outcome at the last moment of follow-up, with still twenty-five percent of the patients reporting bad outcome regardless of the treatment used.
Data availability
Data will be made available upon reasonable request to the corresponding author.
References
Delaney WM, Street DM (1953) Fracture of femoral shaft with fracture of neck of same femur; treatment with medullary nail for shaft and Knowles pins for neck. J Int Coll Surg 19(3):303–312
Becher H (1951) [Nailing of femur neck fracture nailing of femur neck fracture with a concomitant fracture of femur head] Nagelung der Schenkelhalsfraktur bei gleichzeitig bestehender Oberschenkelfraktur. Zentralbl Chir 76(23):1609–1612
Okcu G, Aktuglu K (2003) Antegrade nailing of femoral shaft fractures combined with neck or distal femur fractures. A retrospective review of 25 cases, with a follow-up of 36–150 months. Arch Orthop Trauma Surg 123(10):544–550
Jain P, Maini L, Mishra P, Upadhyay A, Agarwal A (2004) Cephalomedullary interlocked nail for ipsilateral hip and femoral shaft fractures. Injury 35(10):1031–1038
Abalo A, Dossim A, Ouro Bangna AF, Tomta K, Assiobo A, Walla A (2008) Dynamic hip screw and compression plate fixation of ipsilateral femoral neck and shaft fractures. J Orthop Surg (Hong Kong) 16(1):35–38
Peskun C, McKee M, Kreder H, Stephen D, McConnell A, Schemitsch EH (2008) Functional outcome of ipsilateral intertrochanteric and femoral shaft fractures. J Orthop Trauma 22(2):102–106
Vidyadhara S, Rao SK (2009) Cephalomedullary nails in the management of ipsilateral neck and shaft fractures of the femur—one or two femoral neck screws? Injury 40(3):296–303
Schmal H, Strohm PC, Mehlhorn AT, Hauschild O, Südkamp NP (2008) Management of ipsilateral femoral neck and shaft fractures. Unfallchirurg 111(11):886–891
Ostrum RF, Tornetta IP, Watson JT, Christiano A, Vafek E (2014) Ipsilateral proximal femur and shaft fractures treated with hip screws and a reamed retrograde intramedullary nail. Clin Orthop Relat Res 472(9):2751–2758
Alho A (1997) Concurrent ipsilateral fractures of the hip and shaft of the femur. A systematic review of 722 cases. Ann Chir Gynaecol 86(4):326–336
Marins MHT, Pallone LV, Vaz BAD, Ferreira AM, Nogueira-Barbosa MH, Salim R et al (2021) Ipsilateral femoral neck and shaft fractures. When do we need further image screening of the hip? Injury-Int J Care Injured. 52:S65–S69
Cannada LK, Viehe T, Cates CA, Norris RJ, Zura RD, Dedmond B et al (2009) A retrospective review of high-energy femoral neck-shaft fractures. J Orthop Trauma 23(4):254–260
Tornetta IP, Kain MSH, Creevy WR (2007) Diagnosis of femoral neck fractures in patients with a femoral shaft fracture: Improvement with a standard protocol. J Bone Jt Surg Ser A 89(1):39–43
Alho A (1996) Concurrent ipsilateral fractures of the hip and femoral shaft: a meta-analysis of 659 cases. Acta Orthop Scand 67(1):19–28
Shuler TE, Gruen GS, DiTano O, Riemer BL (1997) Ipsilateral proximal and shaft femoral fractures: spectrum of injury involving the femoral neck. Injury 28(4):293–297
Krastman P, Welvaart WN, Breugem SJ, van Vugt AB (2004) The Holland nail: a universal implant for fractures of the proximal femur and the femoral shaft. Injury 35(2):170–178
Casey MJ, Chapman MW (1979) Ipsilateral concomitant fractures of the hip and femoral shaft. J Bone Jt Surg Am 61(4):503–509
Spitler CA, Kiner D, Swafford R, Bruce J, Nowotarski P (2020) Treatment of ipsilateral femoral neck and shaft fractures with cannulated screws and antegrade reconstruction nail. J Orthop Trauma 34(5):E176–E180
Zhao Y, Yu JL, Wang CX, Zhu D, Yu TC (2016) Long Gamma3 compressing interlocking nails with a supplementary cross-cannulated screw for ipsilateral femoral neck and shaft fractures. Int J Clin Exp Med 9(7):14772–14780
Tsarouhas A, Hantes ME, Karachalios T, Bargiotas K, Malizos KN (2011) Reconstruction nailing for ipsilateral femoral neck and shaft fractures. Strateg Trauma Limb Reconstr 6(2):69–75
Dousa P, Bartonicek J, Pavelka T, Lunacek L (2010) Ipsilateralni zlomeniny proximalniho konce a diafyzy femuru. Acta Chir Orthop Traumatol Cech 77(5):378–388
Wu KT, Lin SJ, Chou YC, Cheng HH, Wen PC, Lin CH et al (2020) Ipsilateral femoral neck and shaft fractures fixation with proximal femoral nail antirotation II (PFNA II): technical note and cases series. J Orthop Surg Res 15(1):20
Hung SH, Hsu CY, Hsu SF, Huang PJ, Cheng YM, Chang JK et al (2004) Surgical treatment for ipsilateral fractures of the hip and femoral shaft. Injury 35(2):165–169
Khallaf F, Al-Mosalamy M, Al-Akkad M, Hantira H (2005) Surgical treatment for ipsilateral fractures of femoral neck and shaft. Med Princ Pract 14(5):318–324
Tsai CH, Hsu HC, Fong YC, Lin CJ, Chen YH, Hsu CJ (2009) Treatment for ipsilateral fractures of femoral neck and shaft. Injury 40(7):778–782
Bedi A, Karunakar MA, Caron T, Sanders RW, Haidukewych GJ (2009) Accuracy of reduction of ipsilateral femoral neck and shaft fractures–an analysis of various internal fixation strategies. J Orthop Trauma 23(4):249–253
Kesemenli CC, Tosun B, Kim NS (2012) A comparison of intramedullary nailing and plate-screw fixation in the treatment for ipsilateral fracture of the hip and femoral shaft. Musculoskelet Surg 96(2):117–124
Kang L, Liu H, Ding Z, Ding Y, Hu W, Wu J (2020) Ipsilateral proximal and shaft femoral fractures treated with bridge-link type combined fixation system. J Orthop Surg Res 15(1):399
Oh CW, Kim JW, Oh JK, Apivatthakakul T, Park KH, Hong W (2020) “Reverse miss-a-nail technique” of reconstruction nailing for successful fixation of the ipsilateral femoral neck and shaft fracture. Arch Orthop Trauma Surg 141:959–969
Swiontkowski MF, Hansen ST Jr, Kellam J (1984) Ipsilateral fractures of the femoral neck and shaft. A treatment protocol. J Bone Jt Surg Am. 66(2):260–268
Gautier E, Ganz K, Krugel N, Gill T, Ganz R (2000) Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br 82(5):679–683
Bali K, Gahlot N, Aggarwal S, Goni V (2013) Cephalomedullary fixation for femoral neck/intertrochanteric and ipsilateral shaft fractures: surgical tips and pitfalls. Chin J Traumatol 16(1):40–45
Gary JL, Taksali S, Reinert CM, Starr AJ (2011) Ipsilateral femoral shaft and neck fractures: are cephalomedullary nails appropriate? J Surg Orthop Adv 20(2):122–125
Habib ME, Hannout YS, Shams AF (2012) Treatment of ipsilateral femoral neck and shaft fractures. Life Sci J 9(4):813–817
Lawson E, Madougou S, Chigblo P, Quenum G, Ouangre A, Tidjani F et al (2017) Ipsilateral proximal and shaft femoral fractures. Chin J Traumatol 20(3):155–157
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716
ElShafie MH, Morsey HA, Eid YE (2001) Ipsilateral fracture of the femoral neck and shaft, treatment by reconstruction interlocking nail. Arch Orthop Trauma Su 121(1–2):71–74
Chen CH, Chen TB, Cheng YM, Chang JK, Lin SY, Hung SH (2000) Ipsilateral fractures of the femoral neck and shaft. Injury-Int J Care Injured 31(9):719–722
Lin SH, Lo CW, Cheng SC, Kuo MY, Chin LS (2002) Use of reconstruction nails to manage ipsilateral displaced femoral neck-shaft fractures: assessment of a new approach. J Orthop Surg 10(2):185–193
Barei DP, Schildhauer TA, Nork SE (2003) Noncontiguous fractures of the femoral neck, femoral shaft, and distal femur. J Trauma-Injury Infect Crit Care 55(1):80–86
Daglar B, Bayrakci K, Tasbas BA, Deveci A, Gunel U (2004) [A comparison of different fixation combinations for the treatment of ipsilateral hip and femoral diaphyseal fractures] Ayni taraf kalca ve femur cisim kiriklarinin tedavisinde kullanilan farkli tespit kombinasyonlarinin karsilastirilmasi. Ulus Travma Acil Cerrahi Derg 10(2):123–127
Kakkar R, Kumar S, Singh AK (2005) Cephalomedullary nailing for proximal femoral fractures. Int Orthop 29(1):21–24
Pavelka T, Lihart M, Matejka J, Vyskocil V (2005) [Osteosynthesis of ipsilateral hip and femoral shaft fractures with the PFN-long] Osteosynthese ipsilateraler Frakturen des Femurschaftes und des proximalen Femurs mit dem langen proximalen Femurnagel (PFN-long). Zentralbl Chir 130(2):148–152
Kao HK, Wu CC, Lee PC, Su CY, Fan KF, Tseng IC (2006) Ipsilateral femoral neck and shaft fractures treated with Russell-Taylor reconstruction intramedullary nails. Chang Gung Med J 29(1):79–85
Oh CW, Oh JK, Park BC, Jeon IH, Kyung HS, Kim SY et al (2006) Retrograde nailing with subsequent screw fixation for ipsilateral femoral shaft and neck fractures. Arch Orthop Trauma Surg 126(7):448–453
Oh CW (2007) Comparison of operative methods between retrograde and antegrade nailing for ipsilateral femoral shaft and neck fracture. J Korean Fract Soc 20:135
Shetty MS, Kumar MA, Ireshanavar SS, Sudhakar D (2007) Ipsilateral hip and femoral shaft fractures treated with intramedullary nails. Int Orthop 31(1):77–81
Singh R, Rohilla R, Magu NK, Siwach R, Kadian V, Sangwan SS (2008) Ipsilateral femoral neck and shaft fractures: a retrospective analysis of two treatment methods. J Orthop Traumatol 9(3):141–147
Tsai MC, Wu CC, Hsiao CW, Huang JW, Kao HK, Hsu YT (2009) Reconstruction intramedullary nailing for ipsilateral femoral neck and shaft fractures: main factors determining prognosis. Chang Gung Med J 32(5):563–573
Wang HQ, Han YS, Li XK, Li MQ, Wei YY, Wu ZX (2008) Treatment of ipsilateral femoral neck and shaft fractures. Chin J Traumatol 11(3):171–174
Neto NA, Lins RAB, Kojima KE, Da Cunha BL, Neto JSH, Mercadante MT et al (2010) Outcomes in treatment of diaphiseal femur fractures ipsilateral to the neck or transtrocanteric fracture. Acta Ortop Bras 18(5):255–260
Wang WY, Liu L, Wang GL, Fang Y, Yang TF (2010) Ipsilateral basicervical femoral neck and shaft fractures treated with long proximal femoral nail antirotation or various plate combinations: comparative study. J Orthop Sci 15(3):323–330
Wang WY, Yang TF, Liu L, Pei FX, Xie LM (2012) A comparative study of ipsilateral intertrochanteric and femoral shaft fractures treated with long proximal femoral nail antirotation or plate combinations. Orthop Surg 4(1):41–46
Gadegone W, Lokhande V, Salphale Y, Ramteke A (2013) Long proximal femoral nail in ipsilateral fractures proximal femur and shaft of femur. Indian J Orthop 47(3):272–277
Park H (2013) Clinical outcomes and prognostic factors of ipsilateral hip and femoral shaft fractures. Eur Orthop Traumatol 5:123–130
von Ruden C, Tauber M, Woltmann A, Friederichs J, Hackl S, Buhren V et al (2015) Surgical treatment of ipsilateral multi-level femoral fractures. J Orthop Surg 10:7
Shin WC, Jang JH, Jung SJ, Moon NH (2020) Advantages and limitations of intramedullary nailing for the surgical treatment of ipsilateral intertrochanteric and femoral shaft fractures: a retrospective comparative study based on propensity score matching. Eur J Trauma Emerg Surg 48:1779–1786
Xiang F, Ye J, Zhang X, Ge J, Tang L, Yang Y (2021) Comparison of three different internal fixation methods in treatment of ipsilateral femoral neck and shaft fracture. Chin J Tissue Eng Res 25(3):403–408
Angelini A, Mavrogenis AF, Crimi A, Georgoulis J, Sioutis S, Bekos A et al (2021) Double fractures of the femur: a review of 16 patients. Eur J Orthop Surg Traumatol 7:1345–1354
Chaudhary R, Samal N, Chaudhary S (2021) Ipsilateral neck/inter-trochanteric and mid-shaft femoral fractures treated with dual construct implants. J Pharm Res Int 33(58a):426–434
Rana R, Behera H, Behera S II, Amrit G, Singh M (2021) Outcomes of ipsilateral femoral neck and shaft fractures treated with proximal femoral nail antirotation 2. Cureus. 13(10):e18511
Wei YP, Lin KC (2021) Dual-construct fixation is recommended in ipsilateral femoral neck fractures with infra-isthmus shaft fracture: a STROBE compliant study. Medicine 100(17):e25708
Singh S, Ravi A, Maurya PK, Surana R, Rai A (2021) Outcome analysis of dual implant osteosynthesis for ipsilateral proximal and shaft femur fractures: do we need cephalomedullary nails? Cureus 13(7):e16613
Friedman RJ, Wyman ET Jr (1986) Ipsilateral hip and femoral shaft fractures. Clin Orthop Relat Res 208:188–194
Ostermann PA, Henry SL (1994) [Treatment of the ipsilateral femur shaft and femur neck fractures with the Russell-Taylor reconstruction nail] Die Behandlung ipsilateraler Femurschaft- und Schenkelhalsfrakturen mit dem Russell-Taylor-Rekonstruktionsnagel. Chirurg 65(11):1042–1045
Bose WJ, Corces A, Anderson LD (1992) A preliminary experience with the Russell-Taylor reconstruction nail for complex femoral fractures. J Trauma-Injury Infect Crit Care 32(1):71–76
Hoover GK, Browner BD, Cole JD, Comstock CP, Cotler HB (1991) Initial experience with a second generation locking femoral nail: the Russell-Taylor reconstruction nail. Contemp Orthop 23(3):199–208
Wiss DA, Sima W, Brien WW (1992) Ipsilateral fractures of the femoral neck and shaft. J Orthop Trauma 6(2):159–166
Bennett FS, Zinar DM, Kilgus DJ (1993) Ipsilateral hip and femoral shaft fractures. Clin Orthop Relat Res 296:168–177
Lu Y, Uppal HS (2019) Hip FRACTURES: relevant anatomy, classification, and biomechanics of fracture and fixation. Geriatr Orthop Surg Rehabil 10:2151459319859139
Weil YA, Safran O, Greenberg A, Mosheiff R, Liebergall M, Khoury A (2014) Outcome of proximal femoral fractures caused by cycling in the young and mid-aged. Injury 45(8):1251–1255
Sharma A, Sethi A, Sharma S (2018) Comparative analysis of treatment of basicervical femur fractures in young adults with CCS, DHS, and PFN. Rev Bras Ortop 53(6):783–787
Barquet A, Mayora G, Guimaraes JM, Suarez R, Giannoudis PV (2014) Avascular necrosis of the femoral head following trochanteric fractures in adults: a systematic review. Injury 45(12):1848–1858
Hernefalk L, Messner K (1996) Rigid osteosynthesis decreases the late complication rate after femoral neck fracture. The influence of three different osteosynthesis devices evaluated in 369 patients. Arch Orthop Trauma Surg 115(2):71–74
Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM (1995) The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Jt Surg Am 77(7):1058–1064
Upadhyay A, Jain P, Mishra P, Maini L, Gautum VK, Dhaon BK (2004) Delayed internal fixation of fractures of the neck of the femur in young adults. A prospective, randomised study comparing closed and open reduction. J Bone Jt Surg Br. 86(7):1035–1040
Garden RS (1971) Malreduction and avascular necrosis in subcapital fractures of the femur. J Bone Joint Surg Br 53(2):183–197
Watson JT, Moed BR (2002) Ipsilateral femoral neck and shaft fractures—complications and their treatment. Clin Orthop Relat R 399:78–86
Winquist RA, Hansen ST Jr, Clawson DK (1984) Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Jt Surg Am 66(4):529–539
Karadimas EJ, Papadimitriou G, Theodoratos G, Papanikolaou A, Maris J (2009) The effectiveness of the antegrade reamed technique: the experience and complications from 415 traumatic femoral shaft fractures. Strateg Trauma Limb Reconstr 4(3):113–121
Hussain N, Hussain FN, Sermer C, Kamdar H, Schemitsch EH, Sternheim A et al (2017) Antegrade versus retrograde nailing techniques and trochanteric versus piriformis intramedullary nailing entry points for femoral shaft fractures: a systematic review and meta-analysis. Can J Surg 60(1):19–29
Ricci WM, Bellabarba C, Evanoff B, Herscovici D, DiPasquale T, Sanders R (2001) Retrograde versus antegrade nailing of femoral shaft fractures. J Orthop Trauma 15(3):161–169
Yoon RS, Gage MJ, Galos DK, Donegan DJ, Liporace FA (2017) Trochanteric entry femoral nails yield better femoral version and lower revision rates1A large cohort multivariate regression analysis. Injury 48(6):1165–1169
Wolinsky PR, McCarty E, Shyr Y, Johnson K (1999) Reamed intramedullary nailing of the femur: 551 cases. J Trauma-Injury Infect Crit Care 46(3):392–399
Sanders R, Regazzoni P (1989) Treatment of subtrochanteric femur fractures using the dynamic condylar screw. J Orthop Trauma 3(3):206–213
Frihagen F, Grotle M, Madsen JE, Wyller TB, Mowinckel P, Nordsletten L (2008) Outcome after femoral neck fractures: a comparison of Harris Hip Score, Eq-5d and Barthel Index. Injury 39(10):1147–1156
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Jt Surg Am. 51(4):737–755
Acknowledgements
We would like to thank Sabrina Meertens-Gunput, biomedical information specialist of the medical library from Erasmus MC, University Medical Center Rotterdam, Rotterdam, the Netherlands, for developing and assisting with the literature search strategy. Also, we would like to thank Xing Gao, MD and PhD candidate, for helping with the translation of articles in Chinese or Korean.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. There are no statements to declare relating contributorship, data sharing, or ethics approval.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. D. Cnossen declares that he has have no conflict of interests or any competing interests. E. M. M. van Lieshout declares that she has have no conflict of interests or any competing interests. M. H. J. declares that he has have no conflict of interests or any competing interests.
Ethical approval
The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The local Medical Research Ethics Committee exempted this study (ref. no. MEC-2016-348).
Informed consent
Not applicable, review study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cnossen, J.D., Van Lieshout, E.M.M. & Verhofstad, M.H.J. Surgical management of bifocal femoral fractures: a systematic review and pooled analysis of treatment with a single implant versus double implants. Arch Orthop Trauma Surg 143, 6229–6241 (2023). https://doi.org/10.1007/s00402-023-04950-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04950-7