Abstract
Introduction
The purpose of this multi-centre study was to assess external rotation in a large cohort following reverse shoulder arthroplasty (RSA) at a minimum follow-up of 2 years, and identify factors that influence postoperative and/or net-improvement of external rotation.
Methods
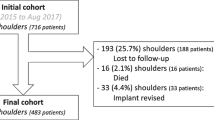
The authors retrospectively reviewed records of 743 RSAs performed between January 2015 and August 2017 by 16 surgeons that participated in a large national society symposium; 193 (25.7%) were lost to follow-up, 16 (2.1%) died, and 33 (4.4%) were revised with implant exchange, which left 501 available for assessment at 2.0–5.5 years. Pre- and post-operative active forward elevation, active external rotation (ER1), active internal rotation (IR1) and constant score (CS) were collected. Regression analyses were performed to determine associations of patient demographics, surgical and implant parameters, rotator cuff muscles status and radiographic angles with ER1.
Results
Multivariable analyses revealed postoperative ER1 decreased with age (β, − 0.35), increased with lateralisation shoulder angle (LSA) (β, 0.26), and was better in shoulders operated by the antero-superior (AS) approach (β, 11.41), but worse in shoulders with absent/atrophic teres minor muscles (β, − 10.06). Net-improvement of ER1 increased with LSA (β, 0.39), was better with inlay stems (β, 8.33) and BIO RSA (β, 6.22), but worse in shoulders operated for primary OA with rotator cuff (RC) tears (β, − 16.26), for secondary OA due to RC tears (β, − 16.06), or for mRCT (β, − 18.96).
Conclusions
This large multi-centre study revealed that, at a minimum of 2 years following RSA, ER1 improved by 16.1°. Postoperative ER1 was better in shoulders which had normal or hypertrophic teres minor muscles, were operated by the AS approach, or with greater LSA. Net-improvement of ER1 was better in shoulders with inlay stems, with BIO RSA, or with greater LSA, but worse in shoulders with rotator cuff deficiency.
Level of evidence
IV.

Similar content being viewed by others
Availability of data and material
The authors would consider making raw data available on request.
Code availability (software application or custom code)
Not applicable.
References
Imai S (2021) Restoration of external rotation following a lateral approach for glenoid bony increased-offset reverse shoulder arthroplasty. JB JS Open Access. https://doi.org/10.2106/jbjs.Oa.20.00136
Puzzitiello RN, Moverman MA, Menendez ME, Hart PA, Kirsch J, Jawa A (2021) Rotator cuff fatty infiltration and muscle atrophy do not impact clinical outcomes after reverse total shoulder arthroplasty for glenohumeral osteoarthritis with intact rotator cuff. J Shoulder Elbow Surg 30(11):2506–2513. https://doi.org/10.1016/j.jse.2021.03.135
Nabergoj M, Onishi S, Lädermann A, Kalache H, Trebše R, Bothorel H, Collin P (2021) Can lateralization of reverse shoulder arthroplasty improve active external rotation in patients with preoperative fatty infiltration of the infraspinatus and teres minor? J Clin Med. https://doi.org/10.3390/jcm10184130
Collin P, Liu X, Denard PJ, Gain S, Nowak A, Lädermann A (2018) Standard versus bony increased-offset reverse shoulder arthroplasty: a retrospective comparative cohort study. J Shoulder Elbow Surg 27(1):59–64. https://doi.org/10.1016/j.jse.2017.07.020
Collotte P, Gauci MO, Vieira TD, Walch G (2022) Bony increased-offset reverse total shoulder arthroplasty (BIO-RSA) associated with an eccentric glenosphere and an onlay 135° humeral component: clinical and radiological outcomes at a minimum 2-year follow-up. JSES Int 6(3):434–441. https://doi.org/10.1016/j.jseint.2021.12.008
Dimock R, Fathi Elabd M, Imam M, Middleton M, Godenèche A, Narvani AA (2021) Bony increased-offset reverse shoulder arthroplasty: a meta-analysis of the available evidence. Shoulder Elbow 13(1):18–27. https://doi.org/10.1177/1758573220916848
Kwapisz A, Rogers JP, Thigpen CA, Shanley E, Newton E, Adams KJ, Alexander R, Hawkins RJ, Kissenberth MJ, Tokish JM, Pill SG (2021) Infraspinatus or teres minor fatty infiltration does not influence patient outcomes after reverse shoulder arthroplasty with a lateralized glenoid. JSES Int 5(1):109–113. https://doi.org/10.1016/j.jseint.2020.09.019
Paclot J, Saab M, Szymanski C, Maynou C, Amouyel T (2021) A low teres minor index of trophicity negatively impacts the functional outcomes of reverse shoulder arthroplasty. Orthop Traumatol Surg Res 107(4):102902. https://doi.org/10.1016/j.otsr.2021.102902
Young BL, Connor PM, Schiffern SC, Roberts KM, Hamid N (2020) Reverse shoulder arthroplasty with and without latissimus and teres major transfer for patients with combined loss of elevation and external rotation: a prospective, randomized investigation. J Shoulder Elbow Surg 29(5):874–881. https://doi.org/10.1016/j.jse.2019.12.024
Koch M, Schmidt C, Kerschbaum M, Winkler T, Pfeifer CG, Greiner S (2021) Reversed shoulder arthroplasty leads to significant histological changes of the deltoid muscle: a prospective intervention trial. Arch Orthop Trauma Surg 141(7):1149–1154. https://doi.org/10.1007/s00402-020-03503-6
Kääb MJ, Kohut G, Irlenbusch U, Joudet T, Reuther F (2022) Reverse total shoulder arthroplasty in massive rotator cuff tears: does the Hamada classification predict clinical outcomes? Arch Orthop Trauma Surg 142(7):1405–1411. https://doi.org/10.1007/s00402-021-03755-w
Greiner S, Schmidt C, Herrmann S, Pauly S, Perka C (2015) Clinical performance of lateralized versus non-lateralized reverse shoulder arthroplasty: a prospective randomized study. J Shoulder Elbow Surg 24(9):1397–1404. https://doi.org/10.1016/j.jse.2015.05.041
Müller M, Greve F, Crönlein M, Zyskowski M, Pesch S, Biberthaler P, Kirchhoff C, Beirer M (2022) Reconstruction or replacement? A challenging question in surgical treatment of complex humeral head fractures in the elderly. Arch Orthop Trauma Surg 142(11):3247–3254. https://doi.org/10.1007/s00402-021-04124-3
Neer CS 2nd, Craig EV, Fukuda H (1983) Cuff-tear arthropathy. J Bone Jt Surg Am 65(9):1232–1244
Hamada K, Fukuda H, Mikasa M, Kobayashi Y (1990) Roentgenographic findings in massive rotator cuff tears. A long-term observation. Clin Orthop Relat Res 254:92–96
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC (1994) Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 304:78–83
Lippe J, Spang JT, Leger RR, Arciero RA, Mazzocca AD, Shea KP (2012) Inter-rater agreement of the Goutallier, Patte, and Warner classification scores using preoperative magnetic resonance imaging in patients with rotator cuff tears. Arthroscopy 28(2):154–159. https://doi.org/10.1016/j.arthro.2011.07.016
Walch G, Edwards TB, Boulahia A, Nové-Josserand L, Neyton L, Szabo I (2005) Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg 14(3):238–246. https://doi.org/10.1016/j.jse.2004.07.008
Boutsiadis A, Lenoir H, Denard PJ, Panisset JC, Brossard P, Delsol P, Guichard F, Barth J (2018) The lateralization and distalization shoulder angles are important determinants of clinical outcomes in reverse shoulder arthroplasty. J Shoulder Elbow Surg 27(7):1226–1234. https://doi.org/10.1016/j.jse.2018.02.036
Simovitch R, Flurin PH, Wright T, Zuckerman JD, Roche CP (2018) Quantifying success after total shoulder arthroplasty: the substantial clinical benefit. J Shoulder Elbow Surg 27(5):903–911. https://doi.org/10.1016/j.jse.2017.12.014
Simovitch R, Flurin PH, Wright T, Zuckerman JD, Roche CP (2018) Quantifying success after total shoulder arthroplasty: the minimal clinically important difference. J Shoulder Elbow Surg 27(2):298–305. https://doi.org/10.1016/j.jse.2017.09.013
Nunes J, Andrade R, Azevedo C, Ferreira NV, Oliveira N, Calvo E, Espregueira-Mendes J, Sevivas N (2022) Improved clinical outcomes after lateralized reverse shoulder arthroplasty: a systematic review. Clin Orthop Relat Res 480(5):949–957. https://doi.org/10.1097/corr.0000000000002065
Austin PC, Steyerberg EW (2015) The number of subjects per variable required in linear regression analyses. J Clin Epidemiol 68(6):627–636. https://doi.org/10.1016/j.jclinepi.2014.12.014
Van de Kleut ML, Yuan X, Teeter MG, Athwal GS (2022) Bony increased-offset reverse shoulder arthroplasty vs. metal augments in reverse shoulder arthroplasty: a prospective, randomized clinical trial with 2-year follow-up. J Shoulder Elbow Surg 31(3):591–600. https://doi.org/10.1016/j.jse.2021.11.007
Simovitch RW, Helmy N, Zumstein MA, Gerber C (2007) Impact of fatty infiltration of the teres minor muscle on the outcome of reverse total shoulder arthroplasty. J Bone Jt Surg Am 89(5):934–939. https://doi.org/10.2106/jbjs.F.01075
Wiater BP, Koueiter DM, Maerz T, Moravek JE Jr, Yonan S, Marcantonio DR, Wiater JM (2015) Preoperative deltoid size and fatty infiltration of the deltoid and rotator cuff correlate to outcomes after reverse total shoulder arthroplasty. Clin Orthop Relat Res 473(2):663–673. https://doi.org/10.1007/s11999-014-4047-2
Boileau P, Watkinson DJ, Hatzidakis AM, Balg F (2005) Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg 14(1 Suppl S):147s–161s. https://doi.org/10.1016/j.jse.2004.10.006
Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Molé D (2004) Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Jt Surg Br 86(3):388–395. https://doi.org/10.1302/0301-620x.86b3.14024
Puskas GJ, Catanzaro S, Gerber C (2014) Clinical outcome of reverse total shoulder arthroplasty combined with latissimus dorsi transfer for the treatment of chronic combined pseudoparesis of elevation and external rotation of the shoulder. J Shoulder Elbow Surg 23(1):49–57. https://doi.org/10.1016/j.jse.2013.04.008
De Fine M, Sartori M, Giavaresi G, De Filippis R, Agrò G, Cialdella S, Fini M, Pignatti G (2022) The role of subscapularis repair following reverse shoulder arthroplasty: systematic review and meta-analysis. Arch Orthop Trauma Surg 142(9):2147–2156. https://doi.org/10.1007/s00402-020-03716-9
Meshram P, Joseph J, Zhou Y, Srikumaran U, McFarland EG (2022) Lateralized glenosphere reverse shoulder arthroplasty: inlay and onlay designs have similar clinical outcomes in patients with glenohumeral osteoarthritis. J Shoulder Elbow Surg 31(4):747–754. https://doi.org/10.1016/j.jse.2021.08.016
Larose G, Fisher ND, Gambhir N, Alben MG, Zuckerman JD, Virk MS, Kwon YW (2022) Inlay versus onlay humeral design for reverse shoulder arthroplasty: a systematic review and meta-analysis. J Shoulder Elbow Surg 31(11):2410–2420. https://doi.org/10.1016/j.jse.2022.05.002
Jackson GR, Meade J, Young BL, Trofa DP, Schiffern SC, Hamid N, Saltzman BM (2023) Onlay versus inlay humeral components in reverse shoulder arthroplasty: a systematic review and meta-analysis. Shoulder Elbow 15(1):4–13. https://doi.org/10.1177/17585732211067171
Loucas R, Kriechling P, Loucas M, El Nashar R, Gerber C, Wieser K (2022) Reverse total shoulder arthroplasty in patients with type B2, B3, and type C glenoids: comparable clinical outcome to patients without compromised glenoid bone stock-a matched pair analysis. Arch Orthop Trauma Surg 142(12):3687–3695. https://doi.org/10.1007/s00402-021-03939-4
Dubiel MJ, Kolz JM, Tagliero AJ, Larson DR, Maradit Kremers H, Cofield RR, Sperling JW, Sanchez-Sotelo J (2022) Analysis of patient characteristics and outcomes related to distance traveled to a tertiary center for primary reverse shoulder arthroplasty. Arch Orthop Trauma Surg 142(7):1421–1428. https://doi.org/10.1007/s00402-021-03764-9
Gillespie RJ, Garrigues GE, Chang ES, Namdari S, Williams GR Jr (2015) Surgical exposure for reverse total shoulder arthroplasty: differences in approaches and outcomes. Orthop Clin North Am 46(1):49–56. https://doi.org/10.1016/j.ocl.2014.09.015
Acknowledgements
Contributors of ReSurg: Jacobus H Müller6, Aude Hibon6, Luca Nover6, Mo Saffarini6.
Funding
The authors are grateful to ELSAN for funding the statistical analysis and manuscript preparation for this study.
Author information
Authors and Affiliations
Consortia
Contributions
LD: Data collection, interpretation of findings and manuscript writing. AG: Study design, data collection, interpretation of findings and manuscript editing. CN: Study design, data collection, interpretation of findings and manuscript editing. RA: Study design, data collection, interpretation of findings and manuscript editing. JHM: Manuscript writing. AH: Project management, data collection, and coordination. LN: Statistical analysis, tables and figures. MS: Interpretation of findings, manuscript writing. JG: Procurement of funding, study design, data collection, interpretation of findings manuscript editing.
Ethics declarations
Conflict of interest
LD, RA states that they have no conflicts of interest. AG and JG reports fees from Tornier SAS outside of the submitted work. CN reports support from DePuy Synthes outside the submitted work.
Consent for publication
All authors approve the submission.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of “ReSurg” are listed in acknowledgements section.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ducharne, L., Godenèche, A., Nérot, C. et al. Factors that affect external rotation following reverse shoulder arthroplasty: a retrospective multi-centre study on 501 shoulders. Arch Orthop Trauma Surg 143, 6487–6496 (2023). https://doi.org/10.1007/s00402-023-04935-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04935-6